Abstract
Bacterial infection may be a critical trigger for variceal bleeding. Antibiotic prophylaxis can prevent rebleeding in patients with acute gastroesophageal variceal bleeding (GEVB). The aim of the study was to compare prophylactic third generation cephalosporins with on-demand antibiotics for the prevention of gastroesophageal variceal rebleeding. In a prospective trial, patients with the first acute GEVB were randomly assigned to receive prophylactic antibiotics (intravenous cefotaxime 2 g q 8 hr for 7 days, prophylactic antibiotics group) or to receive the same antibiotics only when infection became evident (on-demand group). Sixty-two patients in the prophylactic group and 58 patients in the on-demand group were included for analysis. Antibiotic prophylaxis decreased infection (3.2% vs. 15.5%, p=0.026). The actuarial rebleeding rate in the prophylactic group was significantly lower than that in the ondemand group (33.9% vs. 62.1%, p=0.004). The difference of rebleeding rate was mostly due to early rebleeding within 6 weeks (4.8% vs. 20.7%, p=0.012). On multivariate analysis, antibiotic prophylaxis (relative hazard: 0.248, 95% confidence interval (CI): 0.067-0.919, p=0.037) and bacterial infection (relative hazard: 3.901, 95% CI: 1.053-14.448, p=0.042) were two independent determinants of early rebleeding. In conclusion, antibiotic prophylaxis using third generation cephalosporins can prevent bacterial infection and early rebleeding in patients with the first acute GEVB.
Gastroesophageal variceal bleeding (GEVB) is the most serious complication of portal hypertension and represents the leading cause of death in patients with liver cirrhosis. The patients who survive the initial episode of GEVB have a risk of recurrent bleeding approaching 80% at 2 yr (1). Failure to control bleeding and early rebleeding are the most important prognostic factors influencing the 6-week outcome of these patients (2). Rebleeding is associated with an increased risk of exsanguinations, development of liver failure, encephalopathy, and sepsis which contribute to mortality (3). Over the past two decades, many new treatment modalities have been introduced to improve the management of variceal bleeding, including endoscopic injection sclerotherapy (EIS) and variceal ligation (EVL), and new vasoactive agents such as terlipressin and somatostatin (4). Among them, EIS has been replaced almost universally by EVL, because EVL eradicates varices and provides a lower variceal rebleeding rate with fewer secondary effects than EIS does (5). However, the rebleeding rate following endoscopic treatment is still high; at around 25-50% (6). It is therefore important to define how to further reduce the rebleeding rate.
Bacterial infections are frequently associated with upper gastrointestinal bleeding in cirrhotic patients (7). Bacterial infections are more common in cirrhotic patients with acute GEVB than those admitted to hospital with other forms of decompensation, such as encephalopathy (8). Infection may favour variceal bleeding by increasing sinusoidal pressure and altering hemostasis (9). In fact, endotoxemia secondary to bacterial infection may be the critical trigger for variceal bleeding as it produces a wide series of effects that may predispose the cirrhotic patient to bleeding (10). A recent randomized controlled clinical trial has documented the value of quinolone use in preventing rebleeding (6). Prophylactic quinolone can thus further reduce the rebleeding rate in cirrhotic patients with GEVB. However, the use of prophylactic antibiotics can lead to antibiotic resistance with potentially disastrous consequences. It is necessary to prove the benefit of other antibiotics including third generation cephalosporins in preventing rebleeding in cirrhotic patients with GEVB. Therefore, the aim of this study was to compare prophylactic third generation cephalosporins with on-demand antibiotics for the prevention of gastroesophageal variceal rebleeding.
From June 2000 to December 2004, all patients with cirrhosis admitted with upper gastrointestinal bleeding via our hospital emergency room underwent endoscopy within 12 hr of admission. Male or female patients aged over 18 yr were eligible for inclusion in the study after fulfilling the following criteria: 1) diagnosis of cirrhosis on the basis of previous liver biopsy or clinical, biochemical, and radiologic findings of hepatic failure and portal hypertension; 2) bleeding from esophageal varices or gastric varices; and 3) no signs of infection at admission. The severity of cirrhosis was classified according to Child-Pugh's score (11). GEVB was diagnosed when the emergency endoscopy showed any of the following signs: 1) active bleeding from esophageal varices or gastric varices; 2) stigmata of recent hemorrhage over varices (adherent blood clots); or 3) when there was no other cause of upper gastrointestinal bleeding but fresh blood was found in the stomach. Possible complications of endoscopic treatment were discussed with the patients and their relatives, and written informed consent was obtained before entry into the trial.
Patients were excluded from the study if they met the following criteria. First, the patient had a past history of GEVB, or surgical or endoscopic treatment of gastroesophageal varices. Second, the patient received antibiotics within the last 2 weeks. Third, the patient had a terminal illness of any major organ system, or non hepatic malignancy. Forth, the patient had any other causes of upper gastrointestinal bleeding. The diagnosis of hepatocellular carcinoma (HCC) was based on liver biopsy or two coincidental imaging studies as well as one imaging study associated with alpha fetoprotein (AFP) more than 400 ng/mL (12). The Ethics Committee of Chonnam National University Hospital approved the treatment protocol.
Randomization was performed at the time of the therapeutic endoscopy by an investigator after patients met clinical and laboratory entry criteria, lacked exclusions, and gave written informed consent for entry into this study. The allocation of patients to treatment was done by drawing sequentially numbered envelopes, each containing a previously determined, randomly selected assignment based on a table of random numbers. Patients in the prophylactic group received antibiotics treatment after randomization with intravenous cefotaxime 2 gram q 8 hr for 7 days. Patients in the on-demand group received antibiotics only when infection was suspected or established. Antibiotics were changed according to the antibiotic sensitivity profile of cultured microorganisms.
A physical examination, complete blood cell count, chest radiography, urine analysis and culture, blood culture, and ascitic fluid neutrophil count with culture (in patients with ascites) were routinely carried out before randomization. Patients were excluded when the initial bacteriologic examination turned out positive finding. If a new infection was suspected, the same procedures were carried out to assess infection. New infections were suspected when there was fever (>38℃), hypothermia (<36℃), unexplained hemodynamic instability, tachypnea, new onset of chest symptoms, dysuria, deterioration of renal function, bowel habit changes, abdominal pain, abdominal distention, as well as alteration of mental state (6). Respiratory infections were diagnosed by clinical symptoms and signs and positive chest radiography findings. Urinary tract infections were diagnosed by the positive urine culture of ≥105 colonies/mL and associated clinical pictures. The diagnosis of bacteremia was based on positive blood culture and clinical signs or symptoms of infection without other recognized causes. The diagnosis of spontaneous bacterial peritonitis was based on ≥250 neutrophils/µL in ascitic fluid (13). Patients without any identified infection source but with fever >38℃ and leukocytosis >11,000/µL with neutrophilia were considered as having possible infections and received on demand antibiotics. In analyzing the incidence of infection and determining the effect of antibiotic prophylaxis, only infectious episodes occurring during the first hospitalization were considered. Therefore, the infection rate was compared by number of events in this period.
Before endoscopic treatment, octreotide was used. If active bleeding was found during endoscopy, endoscopic treatment was performed immediately. EVL was performed for esophageal varices, and EIS was performed for gastric varices. Two experienced therapeutic endoscopists performed the diagnostic and therapeutic endoscopic procedures. They had 4 yr' experience of standard endoscopy. They did not participate in the postprocedure care of the patients, which was conducted by other physicians. Endoscopy was performed with a standard upper endoscope (Olympus GIF-XQ240, Olympus Optical Co., Ltd., Tokyo, Japan). After endoscopic treatment, octreotide was used for 5 days. EVL was performed by using a varioligator kit with a single-shot device (Top Corp., Tokyo, Japan) and a flexible overtube or multiband ligators (Wilson-Cook Medical, Winston-Salem, NC, U.S.A.). Size of esophageal varices was graded according to Conn's classification (14). Grade I-visible only during one phase of respiration/performance of Valsalva maneuver. Grade II-visible during both phases of respiration. Grade III-3-6 mm. Grade IV-varices of >6 mm. EVL was performed biweekly for the first 6 weeks until the varices were obliterated or reduced to Grade I size and could not be banded any further. Follow-up endoscopy was performed every 3 months and, if unremarkable, was moved to every 6 months. EIS was performed by using intravariceal injection with the 1:1 mixture of 0.5 mL N-butyl-2-cyanoacrylate (Histoacryl blue, Braun-Melsungen, Germany) and 0.5 mL Lipiodol (Guerbet Laboratory, Aulnay-Sous-Bris, France) in each shot.
Rebleeding was defined as one or more of the ongoing bleeding signs including fresh hematemesis, hematochezia, fresh blood aspirated via a nasogastric tube, instability of vital signs, or a reduction of hemoglobin by more than 2 g/dL within 24 hr after initial hemostasis. When rebleeding was suspected, immediate endoscopy was performed. If active bleeding or a fresh blood clot was found at the varices, and if fresh blood was found in the stomach without any other causes of upper gastrointestinal bleeding, rebleeding was confirmed. Bleeding esophageal varices were ligated and bleeding gastric varices were injected with the previously mentioned tissue glue again. Rebleeding within 6 weeks of enrollment after initial control of active bleeding was defined as early rebleeding. Treatment failure was defined as a failure to control active bleeding after two attempts of endoscopic treatment, rebleeding more than twice, or bleeding-related death. Rebleeding index for each patient was calculated by dividing the months of follow-up by the number of rebleeding episodes plus one (6).
Rebleeding rate as a primary outcome was compared between two groups, and secondary outcomes such as rebleeding index, treatment failure, bleeding related death, infection rate, transfusion requirements, and admission duration, were also compared between two groups. Quantitative data were summarized as mean±standard deviation. The Student t test was utilized to compare the mean values of continuous variables, and the chi-square test with Yate's correction or Fisher exact test was utilized for the comparison of discrete variables. Kaplan-Meier analysis with the log-rank test was used to compare differences of actuarial probability of rebleeding and survival between two groups. Univariate analysis and stepwise multivariate analysis were performed to assess the potential risk factors of early rebleeding using the Cox proportion hazards regression. A p value of less than 0.05 was accepted as statistically significant. The analysis was performed with statistical software package (SPSS 13.0 version for Windows, SPSS, Chicago, IL, U.S.A.). This study hypothesized a reduction of rebleeding rate from 45% to 20% by using prophylactic antibiotics (6). According to the sample size calculation, the study would require 54 patients in each group. The type I error and type II error were set to 0.05 and 0.2, respectively.
During the study period, 152 patients with the first acute GEVB were recruited and randomized. Eight patients in the prophylactic group and 7 patients in the on-demand group were excluded from analysis due to occult infections. Six patients in the prophylactic group and 11 patients in the on-demand group were excluded due to their refusal to continue in the study. Therefore, 62 patients in the prophylactic group and 58 patients in the on-demand group were included for analysis. Data regarding the clinical characteristics of the patients at entry are outlined in Table 1. There were no significant differences between two groups with respect to age, gender, etiology, association of HCC, Child-Pugh's score, severity of bleeding, endoscopic characteristics, and period of follow-up (Table 1).
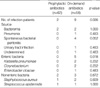
Summary of the infection sources and bacteriology is outlined in Table 2. The incidence of bacterial infection was significantly lower in patient receiving antibiotic prophylaxis (2/62, 3.2% vs. 9/58, 15.5%, p=0.026). Bacteremia and spontaneous bacterial peritonitis were the most common sources of infection. Enteric bacteria were more frequently identified in patients without antibiotic prophylaxis (0/62, 0% vs. 5/58, 8.6%, p=0.018). There were no significant side effects in antibiotic prophylactic group.
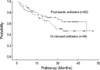
Summary of hemostatic outcome data is outlined in Table 3. The rebleeding rate in the prophylactic group was significantly lower than that in the on-demand group (21/62, 33.9% vs. 36/58, 62.1%, p=0.004). The difference of rebleeding was mostly due to early rebleeding within 6 weeks (3/62, 4.8% vs. 12/58, 20.7%, p=0.012). The cumulative total rebleeding rate and early rebleeding rate were also higher in the on-demand group (Fig. 1, 2). However, there was no significant difference in cumulative late rebleeding rate between the two groups (Fig. 3). The rebleeding sources were not different between the two groups (Table 2). The early rebleeding rate in the infected patients was significantly higher than that in the noninfected patients (4/11, 36.4% vs. 11/109, 10.1%, p=0.031). However, there was no difference in total rebleeding rate between the infected and the noninfected (6/11, 54.5% vs. 52/109, 47.7%, p=0.760). The transfusion requirement was significantly larger in on-demand group than that in prophylactic group (p=0.002). There were no differences in rebleeding index, treatment failure, and duration of hospital stay between the two groups.
Univariate analysis showed the early rebleeding risk significantly linked to antibiotic prophylaxis and bacterial infection (Table 4). On multivariate analysis, antibiotic prophylaxis (relative hazard: 0.248, 95% confidence interval (CI): 0.067-0.919, p=0.037) and bacterial infection (relative hazard: 3.901, 95% CI: 1.053-14.448, p=0.042) were two independent determinants of early rebleeding (Table 5). Univariate analysis showed the late rebleeding risk significantly linked to alcoholics and presence of HCC (Table 6). On multivariate analysis, alcoholics (relative hazard: 1.968, 95% CI: 1.133-3.502, p=0.016) and association with hepatocellular carcinoma (relative hazard: 1.904, 95% CI: 1.035-3.502, p=0.039) were two independent factors predictive of late rebleeding.
Twenty patients and 24 patients died in the prophylactic and on-demand group, respectively. Total mortality and 30-day mortality were not different between the two groups (Table 7). The overall rate of survival was similar between the two groups (Fig. 4). Univariate analysis showed that the survival was significantly related to the presence of HCC, Child-Pugh's score, and bacterial infection (Table 8). On multivariate analysis, presence of HCC (relative hazard: 4.134, 95% CI: 2.261-7.560, p<0.001) and Child-Pugh's score (relative hazard: 1.372, 95% CI: 1.173-1.603, p<0.001) were two independent risk factors determining survival.
In cirrhotic patients, there is a predisposition to intestinal bacterial overgrowth, intestinal dysmotility, and increased intestinal permeability, all leading to an increase in bacterial translocation. Bacterial translocation is the probable source of bacterial byproducts such as endotoxin which can cause an increase in portal pressure, impairment of liver function, and worsening of hemostasis (10). Endotoxemia secondary to bacterial infection may indeed be the critical trigger for variceal bleeding (15). Norfloxacin, ciprofloxacin, and ofloxacin have all been used with these indications (6, 16-21). According to our knowledge, previous studies have never used single third generation cephalosporin for antibiotic prophylaxis for gastrointestinal bleeding. For this reason, third generation cephalosporin can also be used to prevent bacterial infection and rebleeding in cirrhotic patients with an antibacterial resistance after a long term quinolone prophylaxis.
In our study, third generation cephalosporin was used in order to prevent bacterial infection and rebleeding not only because it is safe and efficacious for enteric Gram-negative bacteria, which are the most common causative organisms in cirrhotic patients with acute gastrointestinal bleeding (16-20), but it also has a benefit of covering Gram positive bacteria. The benefit of third generation cephalosporins for preventing early rebleeding in cirrhotic patients with GEVB by decreasing bacterial infection is proved in our study. The prophylactic effect may not sustain over six weeks. However, the period of the greatest risk of early rebleeding is within the first 48 hr after admission (22). The use of early short term antibiotics is very effective in preventing early rebleeding in cirrhotic patients.
In the present study, univariate analysis showed the early rebleeding risk significantly linked to antibiotic prophylaxis and bacterial infection. And, antibiotic prophylaxis (relative hazard: 0.248, 95% CI: 0.067-0.919, p=0.037) and bacterial infection (relative hazard: 3.901, 95% CI: 1.053-14.448, p=0.042) were two independent determinants of early rebleeding by the multivariate analysis. The results suggest that bacterial infection produces a wide series of effects that may predispose the cirrhotic patient to bleeding (10). Therefore, the effective antibiotic prophylaxis should be considered as an essential treatment to prevent early rebleeding.
In our study, total rebleeding rates were higher than those of previous prospective randomized study (47% vs. 32%) (6). There are several possible explanations for these differences in the rebleeding rates. First, this may be because of a difference in the clinical characteristics of the study population, including habitual alcohol drinking. In our study, alcoholism was the most common etiology of liver cirrhosis compared with other study. Second, the difference in the rebleeding rates may stem from the type of antibiotics (quinolone vs. cephalosporin). In a recent survey, 26% of spontaneous bacterial peritonitis episodes were caused by quinolone resistant Gram negative bacilli over a two year period, related to long term treatment with quinolone (23). Fortunately, quinolone resistant E coli are still sensitive to third generation cephalosporins (9). In addition, there is a substantially increased likelihood of infections from Gram positive bacteria in patients who received quinolone prophylaxis (24). Finally, there was a difference in total follow-up periods between the studies. The total follow-up periods in our study (mean, 22 months) were longer than those in the other study (mean, 9 months) (6). Patients who survived after an initial episode have a risk of rebleeding rate approaching 80% in 2 yr (1). The risk of late rebleeding (more than 6 weeks after the initial episode) is related to such factors as continued alcohol consumption, variceal size, renal failure, degree of liver failure, and presence of HCC (2). Alcohol consumption continues to influence prognosis even after cirrhosis has developed. Patients with clinically compensated cirrhosis who become abstinent have a 90% chance of surviving for 5 yr. In contrast, if these patients continue to drink, their chance of survival falls to about 70% (25). In our study, continued alcohol drinking and the presence of HCC were the most important determinants of the late rebleeding. All alcoholic patients with variceal rebleeding continued their habitual alcohol consumption. Accordingly, there was a trend of more episodes of rebleeding in cirrhotic patients after longer follow-up period without correction of this risk factor. In order to lower the risk of late rebleeding, abstinence of alcohol and effective treatment of HCC should be encouraged.
Although the effect of short-term prophylactic antibiotics in patients with GEVB is proved by the reduction of bacterial infection and early rebleeding rate, these beneficial effects are not reflected in terms of mortality and survival in this study. The lack of influence of antibiotic prophylaxis on mortality is likely because of infection is not an independent predictive factor for survival (6). The small impact of rebleeding on survival is possibly due to the fact that most rebleeding episodes can be further controlled by repeated endoscopic treatments (6). Furthermore, on multivariate analysis, presence of HCC (relative hazard: 4.134, 95% CI: 2.261-7.560, p<0.001) and Child-Pugh's score (relative hazard: 1.372, 95% CI: 1.173-1.603, p<0.001) were the only two independent risk factors determining survival in the present study. Actually, most patients died of hepatic failure or multiorgan failure associated with decreased residual liver function and HCC. However, a recent study reported that in-hospital mortality of patients with cirrhosis and acute variceal bleeding has greatly decreased over the past two decades, in concurrence with an early and combined use of pharmacological and endoscopic therapies and short-term antibiotic prophylaxis (26). The use of prophylactic antibiotics decreased the rate of bacterial infections in randomized controlled trials, and a meta-analysis showed that it was associated with improved survival (27). It warrants larger studies to confirm this benefit of antibiotic prophylaxis on mortality.
In conclusion, antibiotic prophylaxis with third generation cephalosporins can prevent bacterial infection and early rebleeding in patients with the first acute GEVB. Although the results are hopeful, larger studies should be performed to confirm this benefit of antibiotics on mortality.
Figures and Tables
Fig. 1
Actuarial probability of remaining free of rebleeding in the patients in terms of prophylactic and on-demand antibiotics use. The difference between the groups was statistically significant (p=0.0035 by log-rank test).
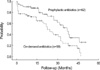
Fig. 2
Actuarial probability of remaining free of early rebleeding in the patients in terms of prophylactic and on-demand antibiotics use. The difference between the groups was statistically significant (p=0.0085 by log-rank test).

Fig. 3
Actuarial probability of remaining free of late rebleeding in the patients in terms of prophylactic and on-demand antibiotics use. The difference between the groups was not significant (p=0.0943 by log-rank test).

Fig. 4
Actuarial probability of survival in the patients in terms of prophylactic and on-demand antibiotics use. The difference between the groups was not significant (p=0.4165 by log-rank test).
References
1. Graham DY, Smith JL. The course of patients after variceal hemorrhage. Gastroenterology. 1981. 80:800–809.

3. D'amico G, de Franchis R. Upper digestive bleeding in cirrhosis. Post-therapeutic outcome and prognostic indicators. Hepatology. 2003. 38:599–612.
4. Carbonell N, Pauwels A, Serfaty L, Fourdan O, Levy VG, Poupon R. Improved survival after variceal bleeding in patients with cirrhosis over the past two decades. Hepatology. 2004. 40:652–659.

5. de la Peña J, Bullet E, Sanches-Hernández E, Rivero M, Vergara M, Martin-Lorente JL, Garcia Suarez C. EVL Study Group. Variceal ligation plus nadolol compared with ligation for prophylaxis of variceal rebleeding: a multicenter trial. Hepatology. 2005. 41:572–578.

6. Hou MC, Lin HC, Liu TT, Kuo BI, Lee FY, Chang FY, Lee SD. Antibiotic prophylaxis after endoscopic therapy prevents rebleeding in acute variceal hemorrhage: a randomized trial. Hepatology. 2004. 39:746–753.

7. Goulis J, Armonis A, Patch D, Sabin C, Greenslade L, Burroughs AK. Bacterial infection is independently associated with failure to control bleeding in cirrhotic patients with gastrointestinal hemorrhage. Hepatology. 1998. 27:1207–1212.

8. Borzio M, Salerno F, Piantoni L, Cazzaniga M, Angeli P, Bissoli F, Boccia S, Colloredo-Mels G, Corigliano P, Fornaciari G, Marenco G, Pistara R, Salvagnini M, Sangiovanni A. Bacterial infection in patients with advanced cirrhosis: a multicentre prospective study. Dig Liver Dis. 2001. 33:41–48.

9. Wong F, Bernardi M, Balk R, Christman B, Moreau R, Garcia-Tsao G, Patch D, Soriano G, Hoefs J, Navasa M. International Ascites Club. Sepsis in cirrhosis: report on the 7th meeting of the International Ascites Club. Gut. 2005. 54:718–725.

10. Thalheimer U, Triantos CK, Samonakis DN, Patch D, Burroughs AK. Infection, coagulation, and variceal bleeding in cirrhosis. Gut. 2005. 54:556–563.

11. Pugh RN, Murray-Lyon IM, Dawson JL, Peitroni MC, Williams R. Transection of the esophagus for bleeding esophageal varices. Br J Surg. 1973. 60:646–649.
12. Bruix J, Sherman M, LIovet JM, Beaugrand M, Leincioni R, Burroughs AK, Christensen E, Pagliaro L, Colombo M, Rodes J. Clincal management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL Conference. J Hepatol. 2001. 35:421–430.
13. Rimola A, Garcia-Tsao G, Navasa M, Piddock LJ, Planas R, Bernard B, Inadomi JM. International Ascites Club. Diagnosis, treatment and prophylaxis of spontaneous bacterial peritonitis: a consensus document. J Hepatol. 2000. 32:142–153.

14. Conn HO. Ammonia tolerance in the diagnosis of esophageal varices: A comparison of the endoscopic, radiologic, and biochemical techniques. J Lab Clin Med. 1967. 70:442–451.
15. Goulis J, Patch D, Burroughs AK. Bacterial infection in the pathogenesis of variceal bleeding. Lancet. 1999. 353:139–142.

16. Rimola A, Bory F, Teres J, Perez-Ayuso RM, Arroyo V, Rodes J. Oral, nonabsorbable antibiotics prevent infection in cirrhotics with gastrointestinal hemorrhage. Hepatology. 1985. 5:463–467.

17. Soriano G, Guarner C, Tomas A, Villanueva C, Torras X, Gonzalez D, Sainz S, Anguera A, Cusso X, Balanzo J. Norfloxacin prevents bacterial infection in cirrhotics with gastrointestinal hemorrhage. Gastroenterology. 1992. 103:1267–1272.

18. Blaise M, Pateron D, Trinchet JC, Levacher S, Beaugrand M, Pourriat JL. Systemic antibiotic therapy prevents bacterial infection in cirrhotic patients with gastrointestinal hemorrhage. Hepatology. 1994. 20:34–38.

19. Pauwels A, Mostefa-Kara N, Debenes B, Degoutte E, Levy VG. Systemic antibiotic prophylaxis after gastrointestinal hemorrhage in cirrhotic patients with a high risk of infection. Hepatology. 1996. 24:802–826.

20. Hsieh WJ, Lin HC, Hwang SJ, Hou MC, Lee FY, Chang FY, Lee SD. The effect of ciprofloxacin in the prevention of bacterial infection in patients with cirrhosis after upper gastrointestinal bleeding. Am J Gastroenterol. 1998. 93:962–966.

21. Sabat M, Kolle L, Soriano G, Ortiz J, Pamplona J, Novella MT, Villanueva C, Sainz S, Torras J, Balanzo J, Guarner C. Parenteral antibiotic prophylaxis of bacterial infections does not improve cost-efficacy of oral norfloxacin in cirrhotic patients with gastrointestinal bleeding. Am J Gastroenterol. 1998. 93:2457–2462.
22. Comar KM, Sanyal AJ. Portal hypertensive bleeding. Gastroenterol Clin North Am. 2003. 32:1079–1105.

23. Fernandez J, Navasa M, Gomez J, Colmenero J, Vila J, Arroyo V, Rodes J. Bacterial infections in cirrhosis: epidemiological changes with invasive procedures and norfloxacin prophylaxis. Hepatology. 2002. 35:140–148.

24. Campillo B, Dupeyron C, Richardet JP, Mangeney N, Leluan G. Epidemiology of severe hospital-acquired infections in patients with liver cirrhosis: effect of long-term administration of norfloxacin. Clin Infect Dis. 1998. 26:1066–1070.

25. Diehl AM. Liver disease in alcohol abusers: clinical perspective. Alcohol. 2002. 27:7–11.




 PDF
PDF ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download