Abstract
The objective of this study was to review the natural history of extrapulmonary small cell carcinoma (EPSCC) with specific emphasis on clinical features, response to treatment and survival. The records of all patients (n=34) with EPSCC treated at Yeungnam University Medical Center and Catholic University of Daegu Medical Center between 1998 and 2005 were retrieved and reviewed. The primary sites of tumor were the esophagus and thymus in 6 patients (17.6%) each, pancreas and stomach in 5 patients each (14.7%); other sites included were the cervix, abdominal lymph nodes, abdominal wall, bladder, colon, maxillary sinus, nasal cavity, ovary, parotid gland and liver. Twenty three patients out of 34 had limited disease. The median survival of all patients was 14 months. Independent prognostic factors included stage and primary tumor location. The prognosis for the patients with extensive disease and in the gastrointestinal group was unfavorable. EPSCC is a non homogeneous disease entity. As a result of its frequent recurrence, multimodal therapy has a better outcome even in cases of limited disease. Combination chemotherapy plays a central role for treatment of extensive disease in EPSCC. Further multicenter studies are now needed to determine more details regarding disease subclass and optimal treatment modality.
Since its initial description by Duguid and Kennedy in 1930, extrapulmonary small cell carcinoma (EPSCC) is recognized as a clinicopathological entity distinct from small cell carcinoma of the lung (SCLC) (1-3). However, it is still at times confused with metastatic SCLC. The vast majority of small cell carcinomas (SCC) develop from the lung, but only 2.5% of SCC are present at extrapulmonary sites (4, 5). Unlike SCLC, the natural history of most cases of EPSCC remains uncovered and therefore optimal therapy cannot be determined (4).
The clinical course of the tumor in patients with EPSCC, is generally aggressive and often recurrent (6). The treatment of patients with EPSCC has been similar to protocols used SCLC. Because of its relative chemosensitive nature, the majority of EPSCC patients have been treated with cisplatinum-based regimens for chemotherapy (7). Because it is a systemic disease, localized treatment alone promises only limited survival; therefore, even at early stage, multimodality therapy is preferred.
The purpose of our study was to review the experience with EPSCC with the specific emphasis on clinical features, responses to treatment and survival.
The tumor registry databases at the Yeungnam University Medical Center and Catholic University of Daegu Medical Center were reviewed. Between 1998 and 2005, there were total 818 patients who diagnosed small cell carcinoma and 34 cases were in extrapulmonary sites (4.1%). We retrieved and reviewed the records of all 34 patients; the variables analyzed were: demographic findings, ECOG performance status, and location of primary tumor, stage, treatment modality and response to therapy.
By definition, patients were included if they had no parenchymal lung lesion found on chest CT scan, normal sputum cytology and/or bronchoscopic examination. The histological criteria for the diagnosis of EPSCC was similar to that of SCLC: round to spindle-shaped small cells with dense nuclei, inconspicuous nucleoli, and sparse cytoplasm (8). All cases expressed a neuroendocrine antigen such as chromogranin A and/or synaptophysin as a result of immunohistochemistry analysis. Patients with a well differentiated neuroendocrine tumor, mixed histologic type or Merkel cell carcinoma of the skin were excluded.
In most of the cases, treatment was similar to in cases of SCLC, so, the patients were divided into 2 groups, limited or extensive disease in accordance with the SCLC staging system. Limited disease (LD) was defined as a localized tumor with or without regional lymph node involvement that was easily encompassed within a radiation field. Any extension beyond the locoregional boundaries was defined as extensive disease (ED) (2).
Assessment of response was carried out using the criteria of World Health Organization criteria. Complete response (CR) was defined as complete resolution of disease by physical and radiographic examination, absence of new lesions and disease related symptoms. Partial response (PR) was defined as ≥50% reduction in the sum of the products of perpendicular measurements of all sites of measurable disease; progressive disease (PD) was defined as a ≥25% increase. Stable disease (SD) was defined by any condition other than objective response or PD.
The SPSS version 11.5 was used for the statistical analysis of a correlation between factors such as ECOG, sex, chemotherapeutic regimen, age, location of tumor and overall survival or response to therapy. The correlation of factors and response to therapy were assessed using the Fischer's exact test; the factors correlated to survival were evaluated using the Log-rank test for univariate analysis. We used Cox-regression analysis for multivariate analysis. Survival was analyzed as the time from diagnosis to death or last follow up. Overall survival was estimated by the Kaplan-Meier methods.
All 34 patients were enrolled; 23 patients were male (67.6%) and the other 11 were female (32.4%). The median age was 56 yr (range, 26-87 yr). Twenty patients (59%) were older than 60 yr of age. Twenty one patients were smokers and among them, 20 patients (95%) were men. All patients had a good performance scale, ECOG 1 or 2.
The primary sites for EPSCC in this series were: the esophagus in 6 patients (17.6%), the thymus in 6 patients (17.6%), the stomach in 5 patients (14.7%), the pancreas in 5 patients (14.7%), the cervix in 2 patients (5.9%); there was 1 patients each (2.9%) for the following sites: abdominal lymph node, abdominal wall, bladder, colon, maxillary sinus, nasal cavity, ovary, parotid gland, prostate and liver. There were more than 50% EPSCC located in the gastrointestinal (GI) tract. So we divided two group: GI group versus non-GI group to evaluate the prognostic factors.
There were 23 patients in the LD and 11 patients were in the ED at diagnosis (Table 1). Comparisons of the GI group versus the non-GI group: there were 11 patients in LD GI group, 7 patients in ED GI group, and 12 patients in LD non-GI group and 4 patients in ED non-GI group, showed no statistically significant difference for the stage at diagnosis between the two groups (p=0.477).
After the initial evaluation and confirmation of the histological diagnosis, 1 patient was lost to follow up.
Among the 23 patients in the LD, 1 patient was lost to follow up. Six patients (26%) had received curative resection with adjuvant chemotherapy and 2 patients (9%) received surgery plus concurrent chemoradiotherapy. Five patients (22%) had received concurrent or sequential adjuvant radiotherapy without surgical resection. Four patients received chemotherapy alone and 2 patients received surgical treatment without chemotherapy and only 1 patient received radiotherapy without chemotherapy. Two patients received only supportive care due to advanced age and refusal of other treatment. Three patients with LD are still alive and remain in a disease free state.
As in SCLC, the most commonly used chemotherapy regimen was the combination of etoposide and platinum compounds (cisplatin or carboplatin) (Table 2). Patients in LD tended to receive multimodality therapy compared to the patients in the ED. Four patients (36%) with ED were treated with systemic chemotherapy alone. The other five patients (45%) also received combination chemotherapy with palliative surgery or radiotherapy. There were 2 patients who had no treatment.
Because the treatment modality for LD varied extensively, we had too few patients to decide the response. Among patients in ED, the response was CR in 1 patient, PR in 2 patients, SD in 4 patients and PD in 2 patients. Including CR and PR, the response rate (RR) for ED patients was about 33%. Statistically significant factors that correlated to the response were not identified in our study by univariate analysis.
Sixteen patients out of the 23 patients who showed response above SD relapsed. Nine patients showed locoreginal recurrence, 4 patients metastasized to brain, 2 patients showed multiple bone metastasis and 1 patient progressed to liver metastasis.
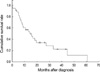
The survival curve for all patients is demonstrated in Fig. 1. The median survival was about 14 months (95% CI 7.88-20.96 months). The one year survival rate was about 56%.
In some disease such as lymphoma and acute myeloid leukemia, the age 60 yr has an independent role for prognosis, so we divided the age groups into an older or younger, with 60 yr as the cut off, for analyzing the correlation of age to survival. Among the factors studied: ages, stage at diagnosis and tumor location were the factors statistically significant in comparison to survival (p=0.0353, p=0.0001 and p=0.0001 respectively). According to multivariate analysis, stage and tumor location also played roles as independent prognostic factors for survival (p=0.00 both), however, age did not have statistical significance (p=0.112).
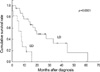
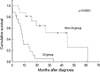
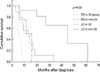
The median survival for the patients with LD was 19.8 months (95% CI 5.2-34.5 months). On the other hand, in patients with ED, the survival was about 7 months (95% CI 4.6-9.7 months). The differences between them in survival were statistically significant (Fig. 2). The median survival for the GI group was shorter than that of non-GI group. The median survival for the GI group was 8 months (95% CI 6.2-10 months) and for the non-GI group, was 44.6 months (95% CI, 19.7-69.5) (Fig. 3). We also evaluated the four groups; LD in GI group, LD in non-GI, ED in GI and ED in non-GI, and the survival was 13.4 months, 44.6 months, 5.2 months and 11.3months each other (log rank p=0.00) (Fig. 4).
Thirty four patients with EPSCC were reviewed and analyzed in our study. EPSCC is a very rare clinicopathological entity (9). In general, the clinical course of this tumor is very aggressive and often recurs after treatment (6).
According to the previous studies, tumors develop from throughout the body in areas such as the head and neck, pancreas, cervix, kidney, urinary tract, prostate and esophagus (10-13). In our study, the most common location for EPSCC were the esophagus (6 patients 17.6%) and the thymus (6 patients 17.6%). The stomach and pancreas accounted for 5 patients each (14.7%). The other sites involved were: cervix, prostate, maxillary sinus, nasal cavity, abdominal lymph nodes, abdominal wall, colon, liver and parotid gland. The prevalence of involved sites is different at different institutions (14).
Among 34 patients, more than 67% of the patients were men (23 patients) and approximately 61.8% of the affected patients had a history of smoking, and 95% of smokers were men. Some studies have suggested that cigarette smoking is associated with EPSCC of particular sites especially the head and neck or esophagus (4). Our study also showed a tendency for this correlation but could not conclude definitively because of the limitations of the retrospective study.
Patients with LD in our study were likely to receive radical surgery or radiotherapy followed by adjuvant chemotherapy. Patients in LD group were considered to have systemic disease therefore, systemic chemotherapy was needed after local treatment. Multimodality therapy is required for the majority of patients with LD to improve overall outcome (15). For patients with ED regardless of site of origin, systemic combination chemotherapy is the most appropriate treatment modality (16, 17). The chemotherapeutic regimens used for treatment of EPSCC were similar to those of SCLC (18). The most common regimens used in our study were the combination of etoposide-cisplatinum (13 patients; 38.2%) or camptothecin-cisplatinum (13 patients; 38.2%).
The response to treatment and median survival in group of patients with this therapy has been disappointing (2). In our study, the response rate of the ED patients was only 33%, more unfavorable than other reports. The cause for the disappointing results requires further study for explanation. There were no statistically significant factors that correlated with the treatment response.
The median survival for all patients was 14 months (95% CI 7.9-21.0). The stage at diagnosis and location of disease, especially for the GI group were independent prognostic factors of survival. The overall survival of the patients with LD was more favorable than for the patients with ED (p=0.0001). In case of LD, more than 50% patients received operation or radiotherapy for local control, maybe it is the main cause of the difference in survival. The overall survival for ED EPSCC in this study was 7 months, and was different from survival for SCLC in ED. The result of EPSCC was unfavorable than SCLC. In SCLC, the median survival of ED patients was about 9 to 12 months (7). The overall survival for patients with SCC of the GI tract was shorter than non-GI tract SCC. SCC of the GI tract is rare and most commonly found in patients of advanced age; previous reports suggest a dismal prognosis (4, 19). The range of median survival is reported to be from several weeks to 6-12 months (20-22). In our study, the median survival of GI group was about 8 months. There were no significant factors identified to differentiate the GI group from the non GI group in our study.
The patients in LD of non-GI group has the longest survival. EPSCC is not metastatic SCLC but similar treatment modalities are used in both disorders; the response and overall survival is not the same. Combination chemotherapy is considered the treatment of choice for EPSCC: however, active local treatment also has an important role in LD EPSCC.
Our study has several limitations related to the retrospective design and the small number of patients. However, the overall survival and independent prognostic factors closely resemble other reports (2). Further prospective multicenter studies are required for better understanding of disease entities and response to treatment modalities.
References
1. Duguid JB, Kennedy AM. Oat-cell tumors of mediastinal glands. J Pathol Bacteriol. 1930. 33:93–99.
2. Richardson RL, Weiland LH. Undifferentiated small cell carcinoma in extrapulmonary sites. Semin Oncol. 1982. 9:484–496.
4. Remick SC, Hafez GR, Carbone PP. Extrapulmonary small-cell carcinoma. A review of the literature with emphasis on therapy and outcome. Medicine (Baltimore). 1987. 66:457–471.
5. Henricus FM, Yvonne F. Extrapulmonary small cell carcinoma. South Med J. 2005. 98:345–349.
6. Remick SC, Ruckdeschel JC. Extrapulmonary and pulmonary small cell carcinoma: tumor biology, therapy and outcome. Med Pediatr Oncol. 1992. 20:89–99.
7. Christodoulou C, Skarlos DV. Treatment of small cell lung cancer. Seminar Respir Crit Care Med. 2005. 26:333–341.

8. WHO. The World Health Organization histological typing of lung tumors. Am J Clin Pathol. 1982. 77:123–136.
9. Sengoz M, Abacioglu U, Salepci T, Ereb F, Yumuk F, Turhal S. Extrapulmonary small cell carcinoma: multimodality treatment results. Tumori. 2003. 89:274–277.

10. Fujii H, Aotake T, Horiuchi T, Chiba Y, Imamura Y, Tanaka K. Small cell carcinoma of the gallbladder: a case report and review of 53 cases in the literature. Hepatogastroenterology. 2001. 48:1588–1593.
11. Tsunoda S, Jobo T, Arai M, Imai M, Kanai T, Watanabe J, Obokata A, Kuramoto H. Small cell carcinoma of the uterine cervix: a clinicopathologic study of 11 cases. Int J Gynecol Cancer. 2005. 15:295–300.
12. Shamelian SO, Nortier JW. Extrapulmonary small-cell carcinoma: report of three cases and update of therapy and prognosis. Neth J Med. 2000. 56:51–55.

13. Navneet SM, Paul E, Ronald MB. Therapy and outcome of small cell carcinoma of the kidney. Report of two cases and a systematic review of the literature. Cancer. 2003. 97:1436–1441.
14. Kim JH, Lee SH, Park JN, Kim HY, Lee SI, Nam EM, Park JO, Kim KH, Jung CW, Im YH, Kang WK, Lee MH, Park KC. Extrapulmonary small cell carcinoma: a single-institution experience. Jpn J Clin Oncol. 2004. 34:250–254.
15. Casas F, Ferrer R, Ferrus B, Casals J, Biete A. Primary small cell carcinoma of the esophagus: a review of the literature with emphasis on therapy and prognosis. Cancer. 1997. 80:1366–1372.
16. Nichols GL, Kelsen DP. Small cell carcinoma of the esophagus. The Memorial Hospital experience 1970 to 1987. Cancer. 1989. 64:1531–1533.

17. Huncharek M, Muscat J. Small cell carcionoma of esophagus. The Massachusetts General Hospital experience 1987 to 1993. Chest. 1995. 107:179–181.
18. Lo Re G, Canzonieri V, Veronesi A, Dal Bo V, Barzan L, Zancanaro C, Trovo M. Extrapulmonary small cell carcinoma: a single-institution experience and review of the literature. Ann Oncol. 1994. 5:909–913.
19. Medgyesy CD, Wolff RA, Putnam JB Jr, Ajani JA. Small cell carcinoma of the esophagus: the University of Texas M.D. Anderson Cancer center experience and literature review. Cancer. 2000. 88:262–267.
20. Redman BG, Pazdur R. Colonic small cell undifferentiated carcinoma: a distinct pathological diagnosis with therapeutic implications. Am J Gastroenterol. 1987. 82:382–385.
21. O'Byrne KJ, Cherukuri AK, Khan MI, Farrel RJ, Daly PA, Sweeny EC, Keeling PW. Extrapulmonary small cell gastric carcinoma. A case report and review of the literature. Acta Oncol. 1997. 36:78–80.
22. Wick MR, Wheatherby RP, Weiland LH. Small cell neuroendocrine carcinoma of the colon and rectum: clinical, histologic, and ultrastructural study and immunohistochemical comparison with cloacogenic carcinoma. Hum Pathol. 1987. 18:9–21.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download