Abstract
The Kidd blood group is clinically significant since the Jk antibodies can cause acute and delayed transfusion reactions as well as hemolytic disease of newborn (HDN). In general, HDN due to anti-Jkb incompatibility is rare and it usually displays mild clinical symptoms with a favorable prognosis. Yet, we apparently experienced the second case of HDN due to anti-Jkb with severe clinical symptoms and a fatal outcome. A female patient having the AB, Rh(D)-positive boodtype was admitted for jaundice on the fourth day after birth. At the time of admission, the patient was lethargic and exhibited high pitched crying. The laboratory data indicated a hemoglobin value of 11.4 mg/dL, a reticulocyte count of 14.9% and a total bilirubin of 46.1 mg/dL, a direct bilirubin of 1.1 mg/dL and a strong positive result (+++) on the direct Coomb's test. As a result of the identification of irregular antibody from the maternal serum, anti-Jkb was detected, which was also found in the eluate made from infant's blood. Despite the aggressive treatment with exchange transfusion and intensive phototherapy, the patient died of intractable seizure and acute renal failure on the fourth day of admission. Therefore, pediatricians should be aware of the clinical courses of hemolytic jaundice due to anti-Jkb, and they should be ready to treat this disease with active therapeutic interventions.
The majority of the serious alloimmune hemolysis cases are still due to RhD incompatibility, although ABO maternal-fetal incompatibility is a much more commonly seen disorder. A much smaller fraction of the patients with hemolytic disease of the newborn (HDN) are due to sensitization to Kell, Duffy, Kidd and other Rh antigens (1, 2). The administration of rhesus immunoglobulin (Ig) prophylaxis to the RhD-negative pregnant patients has dramatically decreased the frequency of HDN. At the same time, the proportion of cases that has been caused by Kell, Duffy, Kidd and other Rh antigen incompatibility has increased from the previous estimates of 1% to 3% (3).
Among these antigen groups, the Kidd blood group system was discovered by Allen et al. in 1951 in a mother who had no history of transfusion, and the women had given birth to an infant with mild hemolytic disease that was due to anti-Jka (4). The antithetical anti-Jkb was reported by Plaut et al. (5) in 1953. Anti Jkb can cause hemolytic disease that is usually a mild and has a benign prognosis (6). In contrast the authors of this study experienced a fatal case of a newborn who exhibiting severe HDN associated with anti-Jkb.
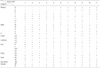
A female patient having the AB, Rh(D)-positive boodtype was admitted for jaundice on the fourth day after being born. The baby was born following a normal vaginal delivery by 39-yr-old mother having birth history of gravida 4, para 2. Her body weight was 3,000 g, and her gestational age was 37 weeks and 5 days. The mother's past history was unremarkable. There was no history for transfusions of blood, plasma or any blood derivatives. The first and second siblings were treated with phototherapy due to neonatal hyperbilirubinemia. At the time of admission, the patient was lethargic and exhibited high pitched crying, she had a normal Moro-reflex, but there was decreased respond to stimulation. The laboratory data indicated a hemoglobin value of 11.4 mg/dL, a reticulocyte count of 14.9% and the appearance of moderate anisocytosis and severe polychromasia in the peripheral blood smear. The seroanalysis showed a total bilirubin of 46.1 mg/dL, a direct bilirubin of 1.1 mg/dL, blood urea nitrogen (BUN) 16 mg/dL, creatinine 0.5 mg/dL, sodium 143 mEq/L, potassium 3.8 mEq/L, chloride 112 mEq/L and a strong positive result (+++) on the direct Coombs test. As a result of the identification of irregular antibody from the maternal serum, anti-Jkb was detected by the Median Diagnostic GmbH Data-Cyte Plus Kit (Median Diagnostic GmbH, Dudingen, Switzerland) (Table 1), which was also found in the eluate made from infant's blood.
She was treated with exchange transfusion and intensive phototherapy for 3 days. A total bilirubin was decreased (16 mg/dL), but she had a convulsion with azotemia and electrolytes imbalance; BUN 41 mg/dL, creatinine 2.2 mg/dL, sodium 134 mEq/L, potassium 8.2 mEq/L, chloride 98 mEq/L. The emergent peritoneal dialysis was initiated under the diagnosis of acute renal failure. Despite the aggressive treatment with peritoneal dialysis and anticonvulsant therapy, the patient died of intractable seizure and acute renal failure on the fourth day of admission. The results of tandem mass screening for metabolic disease revealed normal values. All the specimen cultures showed no growth.
Consequently, the HDN was very likely due to Jkb incompatibility since the fetal bloodtype was AB, Rh-positive and Jkb (+), while the mother was indicated as AB, Rh-positive and Jkb (-).
The Kidd blood group is a major antigenic system in human erythrocytes, and this antigen system is defined by two antithetical specificities, Jka and Jkb, and a third rare recessive gene, Jk, that produces neither Jka nor Jkb antigens (7). The Kidd antigens are localized on a 43 kDa red blood cell integral membrane protein that functions as a urea transporter (8). JKA and JKB are alternate, autosomally inherited codominant alleles. The Kidd blood group is clinically significant since Jk antibodies can cause acute and delayed transfusion reactions as well as HDN.
Anti-Jkb was first described by Plaut et al. in 1953 (5). Most of the reports on anti-Jkb have stated that this condition followed after repeated blood transfusions (9, 10). The first case of anti-Jkb related HDN was reported by Kornstad and Halvorsen in 1958 (11). Up to the present time, only eleven cases of anti-Jkb related HDN have been reported in the medical leterature. Although approximately 20-29% of the Caucasian and Asian population have the phenotype Jk(a+b-) (12-14), introduction of the Jkb antigen into such individuals is rarely associated with clinically manifesting disease. This is apparently due to the fact that Jkb is a poor antigen. Table 2 summarizes the pertinent clinical and serologic data concerning the cases of HDN due to anti-Jkb that have been reported to date (15-22). In all the reported cases, the disease was usually mild to moderate with a benign prognosis. Although all the infants exhibited a strongly positive direct Coombs test, any anemia was either absent or present to only a slight degree.
An additional case of HDN that was apparently due to anti-Jkb has been reported by Kanner (23). This case radically differs from those reported previously in that the woman's third baby was "very jaundiced and anemic", and the baby died at the second day after birth. No other information about the baby was reported. This case has not been included in Table 2 because of insufficient data. The baby in our case was also severely affected at the time of admission and she suffered the neurologic consequences of kernicterus. Despite the medical management with exchange transfusion and intensive phototherapy, the baby died of intractable seizure and acute renal failure at the fourth day after admission.
The pathogenesis of HDN due to anti-Jkb is similar to that of other antibodies. Maternal alloimmunization occurs when a woman's immune system is sensitized to foreign erythrocyte surface antigens that stimulate the production of immunoglobulin G (IgG) antibodies. The most common routes of maternal sensitization are via blood transfusion or by fetomaternal hemorrhage (transplacental passage of fetal erythrocytes), which is associated with delivery, trauma, spontaneous or induced abortion, ectopic pregnancy or invasive obstetrical procedures. In the event of a pregnancy subsequent to becoming alloimmunized, these antibodies can cross the placenta and result in hemolysis of fetal erythrocytes and also anemia, which in turn can lead to potentially disastrous consequences for the fetus (24). Our case and Kanner's cases differ from other reported cases on the maternal history; Kanner's and our case involved the third baby. The first and second babies had been jaundiced, yet they had never been transfused with blood, plasma or any blood derivatives. Therefore, the anti-Jkb antibody production apparently was initiated at the time of pregnancy. We can suggest that both women had three babies with HDN due to anti-Jkb.
Although HDN of anti-Jkb incompatibility is rare malady that generally shows mild clinical symptoms and a favorable prognosis, we experienced the second apparent case of HDN due to anti-Jkb that had severe clinical symptoms and a fatal outcome. Therefore, HDN due to minor blood group instability must be ruled out for all the cases of jaundice occurring 24 hr after birth. Screening and quantification of irregular antibodies are required for early diagnosis as a medical measure to prevent kernicterus through phototherapy and exchange transfusion, and close attention should be paid for possible delayed hemolytic anemia.
As a therapeutic measure, prenatal genotyping for Jkb of the fetal amniotic cells should be done to identify those high risk pregnancies with HDN that are due to anti-Jkb incompatibility, and the genotyping can be done by allele-specific polymerase chain reaction. An allele-specific polymerase chain reaction (ASPCR) assay for prenatal genotyping of the Kidd antigen system in order to identify pregnancies at risk for HDN was developed. The availability of this assay, which can accurately genotype the Kidd blood group system, even in the presence of extensive maternal contamination, provides an important tool in managing pregnancies at risk for Kidd-related HDN (14). For the high risk fetus, intrauterine exchange transfusion (25), serial follow up of the serum bilirubin level and the use of erythropoietin for anemia (26) should be considered.
Figures and Tables
References
1. Moise KJ Jr. Changing trends in the management of red blood cell alloimmunization in pregnancy. Arch Pathol Lab Med. 1994. 118:421–428.
2. Geifman-Holtzman O, Wojtowycz M, Kosmas E, Artal R. Female alloimmunization with antibodies known to cause hemolytic disease. Obstet Gynecol. 1997. 89:272–275.
3. Mentzer WC, Glader BE. Taeusch HW, Ballard RA, editors. Erythrocyte disorders in infancy. Avery's diseases of the newborn. 2004. 8th ed. Philadelphia: W.B Saunders Co;1080–1092.

4. Allen FM, Diamond LK, Niedziela B. A new blood group antigen. Nature. 1951. 167:482.
5. Plaut G, Ikin EW, Mourant AE, Sanger R, Race RR. A new bloodgroup antibody, anti Jkb. Nature. 1953. 171:431.
6. Weinstein L. Irregular antibodies causing hemolytic disease of the newborn: a continuing problem. Clin Obstet Gynecol. 1982. 25:321–332.

7. Issitt PD, Anstee DJ. Issitt P, editor. The Kidd blood group system. Applied Blood Group Serology. 1998. 4th ed. Durham, NC: Montgomery Scientific Publications;655–670.
8. Olives B, Mattei MG, Huet M, Neau P, Martial S, Cartron JP, Bailly P. Kidd blood group and urea transport function of human erythrocytes are carried by the same protein. J Biol Chem. 1995. 270:15607–15610.
9. Sanger R, Race RR, Rosenfield RE, Vogel P. A serum containing anti-s and anti-Jkb. Vox Sang. 1953. 3:115.
10. Rosenfield RE, Ley AB, Haber G, Harris JP. A further example of anti-Jkb. Am J Clin Pathol. 1954. 24:1282–1284.
11. Kornstad L, Halvorsen K. Haemolytic disease of the newborn caused by anti-Jkb. Vox Sang. 1958. 3:94–99.
12. Kelton JG, Heddle NM, Blajchman MA. Blood transfusion. A conceptual approach. 1984. 1st ed. New York: Churchill Livingstone;56.
13. Okubo Y, Yamaguchi H, Nagao N, Tomita T, Seno T, Tanaka M. Heterogeneity of the phenotype Jk(a-b-) found in Japanese. Transfusion. 1986. 26:237–239.

14. Hessner MJ, Pircon RA, Johnson ST, Luhm RA. Prenatal genotyping of Jk(a) and Jk(b) of the human Kidd blood group system by allele-specific polymerase chain reaction. Prenat Diagn. 1998. 18:1225–1231.

15. Geczy A, Eslie M. Second example of hemolytic disease of the newborn caused by anti-Jk-b. Transfusion. 1961. 1:125–127.

16. Wagman E, Bove JR. Anti-Jkb. Hemolytic disease of the newborn caused by anti-Jkb. Am J Clin Pathol. 1964. 41:481–483.
17. Zodin V, Anderson RE. Hemolytic disease of the newborn due to anti-Kidd (Jkb): case report and review of the literature. Pediatrics. 1965. 36:420–422.
18. Lange MM, Lumare A, Corsi C. Hemolytic disease of the newborn caused by anti-Jk-b antibody. Minerva Pediatr. 1974. 26:1765–1767.
19. Kim HO, Kwon OH, Lee SY, Lee YS, Kim SK. A case of hemolytic disease of the newborn due to anti-Jkb. Korean J Hematol. 1986. 21:319–322.
20. Merlob P, Litwin A, Reisner SH, Cohen IJ, Zaizov R. Hemolytic disease of the newborn caused by anti-Jkb. Pediatr Hematol Oncol. 1987. 4:357–360.
21. Tomar V, Dhingra N, Madan N, Faridi MM. Hemolytic disease of the newborn due to maternal anti-Kidd (anti-Jkb). Indian Pediatr. 1998. 35:1251–1253.
22. Park DK, Kim YM, Bae CW, Choi YM, Lee WI. A case of hemolytic disease in a newborn due to Anti-Jkb. Korean J Pediatr. 2003. 46:718–721.
23. Kanner J. Anti-Jkb in erythroblastosis fetalis. Am J Obstet Gynecol. 1962. 83:1253.
24. Nathan DG, Orkin SH, Oski FA. Hematology of Infancy and Childhood. 1998. 5th ed. Philadelphia: W.B Saunders;61–62.
25. Millard DD, Gidding SS, Socol ML, MacGregor SN, Dooley SL, Ney JA, Stockman JA 3rd. Effects of intravascular, intrauterine transfusion on prenatal and postnatal hemolysis and erythropoiesis in severe fetal isoimmunization. J Pediatr. 1990. 117:447–454.

26. Moya FR, Grannum PA, Widness JA, Clemons GK, Copel JA, Hobbins JC. Erythropoietin in human fetuses with immune hemolytic anemia and hydrops fetalis. Obstet Gynecol. 1993. 82:353–358.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download