Abstract
Common complications of Henoch-Schönlein purpura (HSP) that lead to surgical intervention include intussusception, perforation, necrosis, and massive gastrointestinal bleeding. Acute appendicitis is rarely seen as a complication of HSP. A seven-year-old boy was admitted for arthralgia, abdominal pain, hematochezia, melena, and purpuric rash on the lower extremities. On admission day abdominal ultrasonography was normal, but on day 5, he became pyrexial and developed right iliac fossa pain and tenderness with guarding. Ultrasonography showed distended appendix surrounded by hyperechoic inflamed fat. On exploration an acutely inflamed, necrotic appendix was removed and grossly there was an appendiceal perforation in the appendiceal tip. Microscopically some of the small blood vessels in the submucosa showed fibrinoid necrosis with neutrophilic infiltrations. The authors report the case of a child who developed acute perforative appendicitis requiring appendectomy while on treatment for HSP.
Henoch-Schönlein purpura (HSP) is the most common vasculitic disease of childhood. It is a multisystem disorder affecting predominantly the skin, joints, gastrointestinal tract, and kidneys (1). Gastrointestinal manifestation is common occurring in about two thirds of children with HSP (1, 2). Clinically gastrointestinal tract involvement may manifest as colicky abdominal pain, vomiting, melena, hematochezia, and hematemesis. Vasculitic involvement of the ileum or ascending colon may produce signs that mimic acute appendicitis and lead to an unnecessary appendectomy (2-4). This misdiagnosis has been reported to occur as often as 5-7% in two series (1, 4). Acute appendicitis has been reported on rare occasions in conjunction with HSP (2, 5-7). We report a boy with HSP who has shown to have an appendicitis.
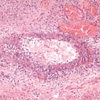
A 7-yr-old boy presented with left knee joint pain, abdominal pain, and purpuric rash on the lower extremities. He was managed with oral prednisolone and supportive care under the impression of HSP at the private clinic for three days. However above symptoms did not improve. Additionally abdominal distension, diarrhea, hematochezia, and melena were developed, so he was transferred to our hospital. On admission, laboratory investigations revealed hemoglobin 12.5 g/dL, white blood cell count 19,200/µL, platelet count 388,000/µL, C-reactive protein 0.69 mg/dL, blood urea nitrogen 11.3 mg/dL, and serum creatinine 0.7 mg/dL. Serum electrolyte, liver enzymes, blood coagulation tests, antinuclear antibody, rheumatoid factor, antistreptolysin O, and urinalysis were normal. Abdominal radiography showed air-fluid levels and abdominal ultrasonography was normal. The patient was treated with intravenous hydration and 1 mg/kg per day methylprednisone. At follow up, the clinical findings such as arthralgia, abdominal pain, bloody stool, and purpuric rash improved gradually over four days. On the 5th hospital day he became pyrexial and developed right iliac fossa pain and tenderness with guarding. White blood cell count was 21,900/µL and C-reactive protein was 8.58 mg/dL. Ultrasonography showed distended appendix surrounded by hyperechoic inflamed fat. On abdominal exploration there was an appendiceal perforation in the appendiceal tip, and pus was present in the periappendiceal area. Microscopically the appendix showed hemorrhagic ulceration of mucosa, gangrenous necrosis throughout wall, and the mucosa showed abundant infiltration of inflammatory cells and eosinophilic fibrinoid materials. Some of the small blood vessels in the submucosa showed fibrinoid necrosis with neutrophilic infiltrations (Fig. 1). Following the operation the colicky abdominal pain, fever, and leukocytosis were resolved, but two days after operation he developed scalp edema, scrotal swelling, and purpuric rash on buttock. Two weeks after operation he was discharged without any clinical symptoms, however microscopic hematuria (5-9 RBC/HPF) has persisted subsequent two months. Six months after operation his recovery was complete.
HSP is a form of systemic vasculitis characterized by vascular wall deposits of predominantly IgA typically involving small vessels in skin, gut, and glomeruli and associated with purpura, colic, hematuria, and arthralgia or arthritis (1). Intra-abdominal manifestations are due to gastrointestinal submucosal and subserosal hemorrhage and edema. Affected children suffer from abdominal pain with or without distension, nausea, vomiting, hematemesis, melena, and bloody stools. Common problems of HSP that lead to surgical intervention include intussusception, perforation, necrosis, and massive gastrointestinal bleeding. Abdominal symptoms and signs of HSP may precede the emergence of the rash, making initial diagnosis difficult, and may even result in unnecessary laparotomy (1, 4, 6). Vasculitic involvement of the ileum or ascending colon may produce signs that mimic acute appendicitis and lead to an unnecessary appendectomy (2-4). This misdiagnosis has been reported to occur as often as 5-7% in two series (1, 4). A correct initial diagnosis is difficult to make when the abdominal complaints precede the onset of rash or if the abdominal signs are localized to the right iliac fossa. Acute appendicitis has been reported on rare occasions in conjunction with HSP (2, 5-7), but is not described in most reported series (1, 8-11). In three cases of appendicitis (2, 6, 7), purpura was not present at the time of surgical treatment. Two patients had rather stormy postoperative courses of continuous abdominal pain, purpura, and nephritis (2, 6). One patient died of uremia 12 weeks after operation (2). In our patient, purpura was observed prior to operation and colicky abdominal pain was subsided after the surgical intervention. Postoperative scrotal swelling in our case could have been due to scrotal involvement which occurs 2-38% of the cases (12). Acute appendicitis in this boy could have been purely coincidental. However, the light-microscopic observations of fibrinoid necrosis with neutrophilic infiltrations in the small vessels of his appendix are highly suggestive of HSP vasculitis.
Serial ultrasonography may helpful to monitor the progression of gastrointestinal involvement in HSP. Although acute appendicitis is rare complications of HSP, a clinical suspicion of acute appendicitis in a child with HSP should not delay operative intervention so as to confirm the diagnosis. Earlier diagnosis and prompt treatment of intra-abdominal complications of HSP will reduce the mortality.
Figures and Tables
References
1. Katz S, Borst M, Seekri I, Grosfeld JL. Surgical evaluation of Henoch-Schönlein purpura: experience with 110 children. Arch Surg. 1991. 126:849–854.

2. Feldt RH, Stickler GB. The gastrointestinal manifestations of anaphylactoid purpura in children. Mayo Clin Proc. 1962. 37:465–473.
3. Choong CK, Beasley SW. Intra-abdominal manifestations of Henoch-Schönlein purpura. J Paediatr Child Health. 1998. 34:405–409.

4. Martinez-Frontanilla LA, Haase GM, Ernster JA, Bailey WC. Surgical complications in Henoch-Schönlein purpura. J Pediatr Surg. 1984. 19:434–436.

5. Um YK, Oh SM, Oh KY, Yoon KA, Chi JG, Choi DH, Kim SC. Acute appendicitis as a complication of Henoch-Schönlein purpura. Pediatr Allergy Respir Dis. 1993. 3:130–137.
6. Mohammed R. Acute appendicitis: a complication of Henoch-Schönlein purpura. J R Coll Surg Edinb. 1982. 27:367.
7. Mir E. Surgical complications in Henoch-Schönlein purpura in childhood. Z Kinderchir. 1988. 43:391–393.

8. Connolly B, O'Halpin D. Sonographic evaluation of the abdomen in Henoch-Schönlein purpura. Clin Radiol. 1994. 49:320–323.
9. Cull DL, Rosario V, Lally KP, Ratner I, Mahour GH. Surgical implications of Henoch-Schönlein purpura. J Pediatr Surg. 1990. 25:741–743.
10. Lindenauer SM, Tank ES. Surgical aspects of Henoch-Schönlein purpura. Surgery. 1966. 59:982–987.
11. Hu SC, Feeney MS, McNicholas M, O'Halpin D, Fitzgerald RJ. Ultrasonography to diagnose and exclude intussusception in Henoch-Schönlein purpura. Arch Dis Child. 1991. 66:1065–1067.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download