Abstract
To evaluate the toxicity and efficacy of a reduced dose intensity (mini-) FOLFOX-4 regimen as a first-line palliative chemotherapy in elderly patients (≥70 yr of age) with advanced colorectal cancer, data from prospective databases at Seoul National University Bundang Hospital and Seoul Municipal Boramae Hospital were analyzed. A total of 20 patients were enrolled between January 2001 and August 2004, and were treated with oxaliplatin 65 mg/m2 on day 1, and with 2-hr infusions of leucovorin 150 mg/m2 followed by a 5-FU bolus (300 mg/m2) and 22-hr continuous infusions (450 mg/m2) for 2 consecutive days every 2 weeks until progression, unacceptable toxicity or patient refusal. Sixteen patients were evaluable for response with an overall response rate of 43.8%. Median progression-free survival was 4.8 months (95% CI: 3.0-6.7) and overall survival was 13.5 months (95% CI: 11.1-16.0). The main side effects were anemia and neutropenia, which were observed in 20.8% and 17.7%, respectively, of the total cycles administered. There were no grade 4 toxicities and only one patient suffered from febrile neutropenia. No grade 3 toxicities occurred except for anemia (5.2%) and vomiting (1.0%). In conclusion, the mini-FOLFOX-4 regimen was found to be well tolerated with acceptable toxicity, and to provide a benefit for elderly patients with colorectal cancer.
Colorectal cancers are primarily diseases of the sixth, seventh, and eighth decades of life. The probability of developing colorectal cancer increases from 0.06% in the first four decades of life to 3-4% in the sixth and seventh decades in the United States (1, 2). Incidence of colorectal cancer is rising and now it ranks fourth common cancer in Korea (3), and this trend is likely to continue as the proportion of elderly in the general population increases.
Chemotherapy has an important role in the management of colorectal cancer. 5-Fluorouracil (5-FU) based adjuvant chemotherapy has resulted in increased disease-free and overall survivals in stage III colon cancer (4), and palliative chemotherapy has extended the lives of patients with metastatic colorectal cancer and improved the quality of life compared with best supportive care (5). Moreover, a number of new agents have become available for the treatment of metastatic colorectal cancer, e.g., oxaliplatin, irinotecan, and capecitabine. The FOLFOX-4 regimen has been found to produce response rates of 30-50%, a progression free survival of 7-9 months, and overall survivals of 16-20 months in a number of phase 2 and 3 trials, and is generally accepted as the standard first line chemotherapy in colorectal cancer (6, 7). Though majority of colorectal cancer patients are elderly, little data is available on the efficacy and safety of the FOLFOX-4 regimen in elderly patients. Moreover, patients above 70 yr of age are underrepresented in clinical trials and are often denied palliative chemotherapy due to a lack of evidence of efficacy and a fear of toxicities (8, 9). In the present study, to minimize toxicity and increase chemotherapy compliance in elderly patients, a reduced dose intensity (mini-) FOLFOX-4 regimen was used. This study was undertaken to evaluate toxicity and efficacy of this mini-FOLFOX-4 regimen in elderly colorectal cancer patients as a first-line palliative chemotherapy.
Using prospective databases, we identified patients older than 70 yr of age with histologically confirmed adenocarcinoma of the colon or rectum and who were treated with the mini-FOLFOX-4 regimen for metastatic or recurrent disease in Seoul National University Bundang Hospital or Seoul Municipal Boramae Hospital. Patients with bidimensionally measurable lesions were included in the study, but patients who received another primary chemotherapy were excluded. Adjuvant chemotherapy was allowed if it had been administered more than 6 months prior to the diagnosis of metastatic or recurrent colorectal cancer. Doses of oxaliplatin and 5-FU in the original FOLFOX-4 regimen were reduced by 25%. Oxaliplatin 65 mg/m2 was administered intravenously over 2 hr on day 1, and this was followed by a bolus injection of 5-FU 300 mg/m2, followed by a two-hour infusions of leucovorin 150 mg/m2, followed by continuous infusion of 5-FU 450 mg/m2 over 22 hr. Leucovorin, 5-FU bolus, and continuous infusion were repeated on day 2 of each 14-day cycle. Treatment was repeated every two weeks until disease progression, unacceptable toxicity or patient refusal. Treatment delays and dose modifications were based on complete blood cell counts taken on the day of the next planned treatment. Toxicity was graded using the National Cancer Institute common toxicity criteria (10). Tumor response was assessed according to standard WHO criteria by CT every 3 to 4 cycles (11). All patients were treated after obtaining informed consent. Data on treatment, toxicity, response, and disease status were prospectively recorded on specially designed forms.
Between January 2001 and August 2004, 20 patients ≥70 yr old were enrolled and administered the mini-FOLFOX-4 regimen at Seoul National University Bundang Hospital and at Seoul Municipal Boramae Hospital. All patients had histologically proven adenocarcinoma of the colon or rectum. Patient characteristics are shown in Table 1. Median patient age was 75 yr (range 70-83), and the majority of the study population were male (16 of 20). Eight patients received adjuvant chemotherapy: 5-FU plus leucovorin in six patients, and oral 5-FU in two.
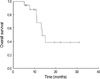
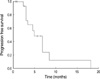
Among twenty patients, 16 patients were evaluable for response. Response evaluations were not possible in four patients; two patients were lost to follow-up after the 1st cycle of treatment and two patients refused further treatment after two cycles, before a response evaluation was conducted. Among the 16 patients evaluable for response, one achieved complete response and 6 partial response, giving an overall response rate per protocol was 43.8% (95% CI: 23.1-66.8) and an overall response rate based on intention-to-treatment analysis was 35% (95% CI: 18.1-56.7). An additional 8 patients achieved stable disease and one progressed. After 19.8 months of median follow-up duration, overall survival was 13.5 months (95% CI: 11.1-16.0) and median progression-free survival was 4.8 months (95% CI: 3.0-6.7). Progression free survival curves and overall survival curves for all patients are shown in Fig. 1, 2. Second line chemotherapy was administered in 13 (65%) patients.
The incidences of main toxicities per cycle and patient are summarized in Table 2. A total of 99 cycles were delivered, and patients received a median of six cycles. The most frequently observed toxicity was anemia, which was reported in 20.8% of the 99 cycles. Neutropenia was mild and occurred in 17.7% of the 99 cycles, and there was only one episode of febrile neutropenia. No grade 3 or 4 toxicities occurred, except for grade 3 anemia and vomiting which were observed in 5 and 1 cycles, respectively. There was no treatment related mortality.
In this study we assessed the clinical efficacy and safety of a mini-FOLFOX-4 regimen in elderly patients with metastatic or recurrent colorectal cancer. This regimen showed a response rate of 43.8% per protocol, a progression free survival of 4.8 months, and a median survival of 13.5 months, and was well tolerated with a <5% incidence of grade 3 or 4 toxicities.
For decades 5-FU was the mainstay palliative chemotherapy for colorectal cancer, until agents such as oxaliplatin and irinotecan were introduced in the 1990's. Combination protocols of oxaliplatin with 5-FU plus leucovorin, known as FOLFOX regimens, have shown remarkable synergy and efficacy in preclinical models and in clinical trials (12). The FOLFOX-4 regimen became the standard therapy for advanced colorectal cancer patients after randomized phase III trials revealed significantly superior, response rates, time to progression, and overall survival of 45%, and 8.7 and 19.5 months, respectively, versus the IFL regimen (31%, 6.9 months, 15.0 months, respectively), which incorporated bolus 5-FU, leucovorin, and another new agent, irinotecan (7). Here, we chose FOLFOX-4 as a first-line palliative chemotherapy in these elderly patients because of its superior efficacy and favorable toxicity profile versus irinotecan, which shows more severe and frequent toxicities such as nausea, vomiting, diarrhea and febrile neutropenia (7). Chemotherapy doses were reduced to decrease toxicities of diarrhea, mucositis and febrile neutropenia, which may be severe and life-threatening in elderly patients.
Although elderly patients comprise a significant proportion of those with colorectal cancer, they are underrepresented in most clinical trials (8, 9). Several studies performed in Europe and in the United States have reported similar benefits from 5-FU based chemotherapies in the elderly, at maintained dose intensities (13-16). Popescu et al. compared the outcome of palliative chemotherapy in 658 patients with colorectal cancer younger than 70 yr old and in 186 patients older than 70 yr and found no difference between the two groups in terms of dose-intensity, response rate, or median failure-free survival time (16). However, median overall survival was significantly shorter in the older patients (9.6 vs. 11.5 months), though the authors suggested that multiple comorbidities and non-cancer related deaths are likely causes of this shorter overall survival. Data on new agents are even more scarce, and few clinical trials have assessed efficacy and tolerability of palliative FOLFOX regimens in elderly patients with advanced colorectal cancer. Mattioli et al. reported a response rate of 32.6% and Berretta et al. reported similar tolerabilities and response rates for the FOLFOX-2 regimen in patients younger and older than 65 yr (17, 18). The 43.8% response rate achieved in the present study is comparable to those of previous FOLFOX studies, and the overall survival of 13.5 months is comparable to those of most published series in the elderly (15, 16). However, progression free survival was shorter in the present study than in those mentioned above. This may be due to the reduced dose intensities used and the small numbers of cycles given. The median time to response for the FOLFOX-4 regimen was found to be nine weeks in most clinical trials (6). In the present study, a median of six cycles of chemotherapy were given and 9 of the 20 received fewer than five cycles. Of these nine patients, the reasons for stopping chemotherapy were; progressive disease in one, toxicity in one, and patient refusal in seven.
The Mini-FOLFOX-4 regimen showed little toxicity and was found to be remarkably safe in our elderly patients including ten patients with an ECOG performance status of 2. The incidence of oxaliplatin-induced neurotoxicity was lower than those in published series probably due to the low cumulative dose of oxaliplatin given. In most clinical trials, the incidence of sensory symptoms causing functional impairment (grade 3 toxicity) was found to rise after a cumulative dose of 700-800 mg/m2 (6, 19), whereas the median cumulative dose of oxaliplatin administered was only 353.5 mg/m2 in the present study. Moreover, the incidence of neutropenia (17.7%) was much lower in our study than that of grade 3/4 neutropenia in a phase 3 trial (41.7% of patients) by de Gramont et al. (6), which is probably due to the reduced 5-FU bolus dose administered.
Elderly patients are often denied palliative chemotherapy. Surveillance, epidemiologic, and End Results data showed that chemotherapy in advanced colorectal cancer patients falls with increasing age, e.g., the percentages of stage IV colorectal cancer patients treated were 45%, 41%, 27%, 18%, and 5% in those aged 65-69, 70-74, 75-79, 80-84, and 85+ in the United States (20). Currently, there are few data available on the usage of chemotherapy for the treatment of elderly patients in Korea (21-23). In our study, a significant proportion of patients refused further treatment in the absence of progressive disease or due to unacceptable toxicities, and five patients stopped chemotherapy after six cycles for non-medical reasons, many of which were cost-related.
In conclusion, the mini-FOLFOX-4 regimen was found to be well tolerated with little toxicity, and provided similar benefit for the elderly colorectal cancer patients. Reduced intensity FOLFOX-4 may be a valuable option for elderly patients with poor performance or for those that refuse chemotherapy for fear of toxic reactions. Patients with a good performance status could be offered palliative chemotherapy at full dose, and be included in research studies, to provide evidence that chemotherapy is beneficial in elderly patients. Moreover, patient-tailored treatments based on comprehensive geriatric and comorbidity scale assessments, rather than fixed dose reductions based on chronological age alone, may provide more benefit to elderly patients with cancer.
Figures and Tables
References
1. Jemal A, Murray T, Samuels A, Ghafoor A, Ward E, Thun MJ. Cancer statistics, 2003. CA Cancer J Clin. 2003. 53:5–26.

3. 2002 Annual Report of the Korea Central Cancer Registry. Headquarter of Korea Central Cancer Registry. Accessed 10 May 2005. Available from: URL: http://www.ncc.re.kr.
4. International Multicentre Pooled Analysis of Colon Cancer Trials (IMPACT) investigators. Efficacy of adjuvant fluorouracil and folinic acid in colon cancer. Lancet. 1995. 345:939–944.
5. Glimelius B, Hoffman K, Graf W, Pahlman L, Sjoden PO. The Nordic Gastrointestinal Tumor Adjuvant Therapy Group. Quality of life during chemotherapy in patients with symptomatic advanced colorectal cancer. Cancer. 1994. 73:556–562.

6. de Gramont A, Figer A, Seymour M, Homerin M, Hmissi A, Cassidy J, Boni C, Cortes-Funes H, Cervantes A, Freyer G, Papamichael D, Le Bail N, Louvet C, Hendler D, de Braud F, Wilson C, Morvan F, Bonetti A. Leucovorin and fluorouracil with or without oxaliplatin as first-line treatment in advanced colorectal cancer. J Clin Oncol. 2000. 18:2938–2947.

7. Goldberg RM, Sargent DJ, Morton RF, Fuchs CS, Ramanathan RK, Williamson SK, Findlay BP, Pitot HC, Alberts SR. A randomized controlled trial of fluorouracil plus leucovorin, irinotecan, and oxaliplatin combinations in patients with previously untreated metastatic colorectal cancer. J Clin Oncol. 2004. 22:23–30.

8. Trimble EL, Carter CL, Cain D, Freidlin B, Ungerleider RS, Friedman MA. Representation of older patients in cancer treatment trials. Cancer. 1994. 74:Suppl 7. 2208–2214.

9. Lewis JH, Kilgore ML, Goldman DP, Trimble EL, Kaplan R, Montello MJ, Housman MG, Escarce JJ. Participation of patients 65 years of age or older in cancer clinical trials. J Clin Oncol. 2003. 21:1383–1389.

10. National Cancer Institute: Guidelines for reporting of adverse drug reactions. 1998. Bethesda, MD: National Cancer Institute, Division of Cancer Treatment.
11. Miller AB, Hoogstraten B, Staquet M, Winkler A. Reporting results of cancer treatment. Cancer. 1981. 47:207–214.

12. Raymond E, Faivre S, Woynarowski JM, Chaney SG. Oxaliplatin: mechanism of action and antineoplastic activity. Semin Oncol. 1998. 25(2):Suppl 5. 4–12.
13. Chiara S, Nobile MT, Vincenti M, Lionetto R, Gozza A, Barzaqcchi MC, Sanguineti O, Repetto L, Rosso R. Advanced colorectal cancer in the elderly: results of consecutive trials with 5-fluorouracil-based chemotherapy. Cancer Chemother Pharmacol. 1998. 42:336–340.

14. Kohne CH, Grothey A, Bokemeyer C, Bontke N, Aapro M. Chemotherapy in elderly patients with colorectal cancer. Ann Oncol. 2001. 12:435–442.
15. Magne N, Francois E, Broisin L, Guardiolo E, Ramaioli A, Ferrero JM, Namer M. Palliative 5-fluorouracil-based chemotherapy for advanced colorectal cancer in the elderly: results of 10-year experience. Am J Clin Oncol. 2002. 25:126–130.
16. Popescu RA, Norman A, Ross PJ, Parikh B, Cunningham D. Adjuvant or palliative chemotherapy for colorectal cancer in patients 70 years or older. J Clin Oncol. 1999. 17:2412–2418.

17. Berretta M, Buonadonna A, Rupolo M, Frustaci S, Bearz A, Sorio R, Freschi A, Scalone S, Michieli M, Spina M, Tirelli U, Colussi AM, Cartei G. Comparison between elderly and non-elderly patients, of efficacy and tolerability of FOLFOX2 schedule in advanced colorectal cancer. Proc Am Soc Clin Oncol. 2001. 20:A2195. (abstr).
18. Mattioli R, Massacesi C, Recchia F, Marcucci F, Cappelletti C, Imperatori L, Pilone A, Rocchi M, Cesta A, Laici G, Bonsignori M, Lippe P. High activity and reduced neurotoxicity of bi-fractionated oxaliplatin plus 5-fluorouracil/leucovorin for elderly patients with advanced colorectal cancer. Ann Oncol. 2005. 16:1147–1151.

19. Haller DG. Safety of oxaliplatin in the treatment of colorectal cancer. Oncology (Huntingt). 2000. 14(12):12 Suppl 11. 15–20.
20. Sundararajan V, Grann VR, Jacobson JS, Ahsan H, Neugut AI. Variations in the use of adjuvant chemotherapy for node-positive colon cancer in the elderly: a population-based study. Cancer J. 2001. 7:213–218.
21. Kim HJ, Min WS, Park YH, Park SJ, Lee JW, Jin JY, Han CH, Park CW, Kim CC. Induction chemotherapy for patients with acute myeloid leukemia aged over 60 years. Korean J Hematol. 2003. 38:228–233.
22. Choi JH, Ahn MJ, Ki MR, Oh HS, Lee YY, Choi IY, Kim IS. Clinical prognostic factors and treatment outcome of aggressive non-Hodgkin's lymphoma in elderly patients. Cancer Res Treat. 2001. 33:324–328.

23. Ryu JW, Ryu SB, Park YI. M-VAC chemotherapy for bladder cancer in elderly. Korean J Urol. 1999. 40:1274–1278.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download