Abstract
Eleven skeletally immature adolescents underwent anterior cruciate ligament reconstruction using a transphyseal tibial and femoral tunnel. An autologous quadrupled hamstring tendon was used in all cases and the average follow-up was 77.7 months. Clinical results were evaluated using Lysholm knee scores and a return to pre-injury sports activities. Radiological results were evaluated using side-to-side differences of instrumented laxities and growth disturbances compared with the uninjured side on final follow-up orthoroentgenograms. The mean Lysholm score was 97.8 (range 94-100) and mean side-to-side laxity difference was 2.4 mm (range 1-4). Ten of 11 patients returned to pre-injury sports activity. No patient had a leg length discrepancy of over 1 cm or a significant abnormal angular deformity of the knee joint. Therefore, anterior cruciate ligament reconstruction using the transphyseal tunnel and hamstring autograft in skeletally immature adolescents is believed to be a reliable treatment method, which is not associated with significant leg length discrepancy or abnormal angular deformity of the knee joint.
Injury to the anterior cruciate ligament (ACL) is infrequent in growing patients with immature bones. However, the incidence of this injury type has increased recently due to increased adolescent participation in leisure and sports activities; moreover, the availability of more accurate diagnostic methods has created concern about this problem (1-7).
Nonoperative treatment results in poor compliance and activity limitations, and poses the risk of additional meniscal injury and early arthrosis due to knee instability. On the other hand, arthroscopic ACL reconstruction poses the risk of growth disturbance due to growth plate injury caused by creating the transphyseal tunnel through the distal femur and proximal tibia (8). Thus, we evaluated the results of arthroscopic ACL reconstruction using hamstring tendon in adolescent patients with growth potential.
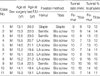
This study included 11 skeletally immature patients from among 445 patients who underwent ACL reconstructions using a hamstring autograft from 1993 to 2001. The patients were all boys of average age 14.7 yr (range 13.1-15.5) at the time of surgery, and aged 21.3 yr (range 19.1-24.0) at the time of the final follow-up (Table 1). The study was approved by the institutional review board of our hospital, and all patients provided informed consent. The average follow-up period was 77.7 months (range 45.0-131). Causes of injury were sports injuries in 10 cases and a traffic accident in one. Associated injuries included medial meniscal injury in 6 cases, lateral meniscal injury in 6, medial collateral injury in 1, and a chondral defect on the medial femoral condyle in one. The average interval between ACL injury and the time of reconstruction was 4.2 months (range 2-12).
All patients underwent intra-articular ACL reconstruction using a standard endoscopic ACL reconstruction technique. A tibial tunnel (7-10 mm, dependent on graft tendon diameter) was drilled through open physes at angles of 55° degrees, and a femoral tunnel (9, 10 mm diameter) was drilled at the 10:30 or 01:30 clock position of the intercondylar notch in the lateral condyle of the femur. An autologous hamstring graft was used. Femoral fixation was performed with staples in one, a Semifix screw (Arthrex, Naples, FL, U.S.A.) in 3, and with a Ligament Anchor screw (LA screw, Solgo, PyeungTaek, Korea) in 7, whilst tibial fixation was done using staples in one and with a biodegradable interference screw in 10 (Linvatec, Largo, FL, U.S.A.) (Table 1).
Clinical outcome was evaluated by comparing, Lysholm knee scores, range of knee motion, degree of knee pain, and degree of returning to a pre-injury sports activity level. Radiographic results were evaluated by comparing knee instability based on measuring anterior translation at the knee treated by ACL reconstruction and at the contralateral knee using a Telos® device (Fa Telos, Medizinisch-Technische GmBH, D-6103 Griesheim, Germany). To compare bone maturities before operation and at the final follow-up, chronological age, physiologic signs of development according to Tanner staging (9), and standing height were measured. Physeal status was determined from knee anteroposterior radiographic findings. Skeletal immaturity was defined when the physes were clearly open in preoperative anteroposterior radiographic views of the knee (Fig. 1A), no adolescent growth spurt occurred, and when the Tanner stage was 1 or 2. Skeletal maturity was defined when physes fusion had either started or was in progress (closing physes) in preoperative anteroposterior radiographic views of the knee (Fig. 1B), and when adolescent growth spurt was past and the Tanner stage was 4 or 5.
Tunnel diameter percentages of the entire femoral and tibial physeal diameters were evaluated using immediate postoperative anteroposterior radiographic views of the knee. At final follow-ups, comparisons were made with normal sides by measuring leg length discrepancy, and femorotibial, anatomical lateral distal femoral (aLDFA), mechanical lateral distal femoral (mLDFA), and mechanical medial proximal tibial (mMPTA) angles on orthoroentgenograms (Fig. 2). The posterior distal femoral angle (PDFA) and the posterior proximal tibial angle (PPTA) were also compared with those of the normal side on lateral radiographs of both knees.
Statistical analysis was performed using the Mann-Whitney test and SPSS software (SPSS for Windows Release 10.0, Chicago, IL, U.S.A.), and the level of significance was set at p<0.05.
Average Lysholm knee scores improved from 51 points (range 25-63) before operation to 97.8 points (range 94-100) at the final follow-up, at which time no joint motion limitation, knee pain, or clinically significant knee instability were observed by physical examination. Ten of the 11 patients were able to return to preinjury sports activity levels, the remaining patient was able to participate in light jogging, but was not able to participate at his preinjury level.
The average tunnel diameter percentages of entire tibial and femoral physes diameters were 13.8% (range, 10.1-16.0%) and 14.5% (range, 12.5-16.7%), respectively on postoperative anteroposterior radiographs. Anterior displacement testing was performed using a Telos® device with a 20 lb load at the final follow-up to evaluate reconstructed ACL stability, the preoperative average of 13.6 mm (range 6-27) improved to 2.2 mm (range 1-4) at the final follow-up.
Tanner stage was determined before operation and at final follow-up to evaluate bone maturity stage. Most cases were in puberty stages preoperatively, namely, stage 2 in 2 cases, stage 3 in 8 cases, and stage 4 in 1 case, whereas all cases showed stage 5 maturity at final follow-up. The average growth in standing height was 14.1 cm, i.e., from 159.2 cm (range 142-172) before operation to 174.3 cm (range 167-185) at final follow-up. Preoperative evaluation of bone maturity, according to the method described by McCarroll et al. (3), showed immature bone in 7 cases and mature bone in 4; no case presented with epiphyseal fusion. Physes were all fused at the final follow-up based on radiographic anteroposterior views of the knee.
Limb length discrepancy was evaluated at the final follow-up by orthoroentgenography, at which time no case presented with a discrepancy of more than 1 cm. And, knee alignment status evaluations by orthoroentgenography at final follow-up in normal and operated sides showed, average femorotibial angles of 6.5° (range 5-8) and 5.9° (range 4-8), respectively, average aLDFA s of 82.0° (range 79-85) and 81.2° (range 78-86), average mLDFA s of 86.6° (range 80-89) and 86.0° (range 83-90), and average mMPTAs of 86.9° (range 85-88) and 86.45° (range 83-89), respectively (Table 2). None of these results were significantly different by Mann Whitney U statistics (p>0.05) (Fig. 3). PDFAs and PPTAs of operated sides also showed no significant differences versus normal sides on the lateral radiographs of the knee joint (Table 2).
Reported injuries are increasing among teenagers because more adolescents are actively participating in sports and as diagnostic techniques are being further improved. Clanton et al. (10) reviewed 1,749 cases of knee ligament injury and reported only 9 cases of ACL injury in patients under 14 yr of age. Lipscomb and Anderson (11) reported an incidence of 3.4%, and Stanitski et al. (12) reported ACL injury in 63% in an examination of acute hemarthrosis in 70 patients between 7 and 18 yr old. In the present study, we identified ACL injury in 12 patients (2.7%) under the age of 17 yr, among 445 cases that received ACL reconstruction from 1994 to 2001.
Treatment for ACL injury can be performed non-operatively or operatively. Non-operative methods include, activity limitation, rehabilitation, and the use of braces, but the prognosis is not good due to the persistence of knee instability, and the developments of new meniscal injuries and complications such as early arthrosis (4, 10, 13-17). Graf et al. (16) reported the presence of knee instability in their 8 cases, 7 of which were found to have a meniscal injury, and thus opted for ACL reconstruction using a hamstring tendon graft in all 8 cases. They proposed that treatment with braces could not prevent knee instability or meniscal injury development.
Operative methods include primary repair, extraarticular procedures, intraarticular procedures without transphyseal tunnels, and intraarticular procedures with transphyseal tunnels. However, a poor prognosis was reported for primary repair in both adults and children (5, 10, 18). The merit of extraarticular reconstruction lies in the fact that no transphyseal tunnel is created, and thus this procedure poses little risk of growth disturbance, but it suffers from the drawback that the reconstructed ACL is nonisometric, even after a long follow-up, and thus the prognosis could not be concluded (3, 16, 19, 20).
Several reports have been issued on transphyseal ACL reconstruction providing improved isometric graft placement in skeletally immature knees (8, 21-24). The important issues for this procedure are the risk of physeal injury due to the creation of transphyseal tunnels and the risk of growth disturbance. Makela et al. (25) and Guzzanti et al. (26) in their experiment using rabbits observed growth disturbance when transphyseal tunnels diameters accounted for more than 7% of the entire physeal diameter. Moreover, Lipscomb and Anderson (11) reported one case of growth arrest among patients with a semitendinosus graft reconstruction.
McCarroll et al. (8) reported that 55 cases were able to return to normal sports activities, and found no growth disturbance due to physeal injury, leg length discrepancy, or angular deformity after following 60 cases with an average age of 14.2 yr at ACL reconstruction using a patellar tendon. Edward and Grana (21) reported that returning to normal sports activities was possible in 19 of their 21 cases, and also found no leg length discrepancy, angular deformity, or knee malalignment among the 21 cases. Thus, they proposed that although the objective size of the transphyseal tunnel is important, that the degree of physes injury is also due to slanting of the tunnel. Thus, physes injury was found to be minimized by making the transphyseal tunnel in the tibia more vertically at an angle of 60° rather than 50-55°. However, no conclusion was drawn on the maximum size of the transphyseal tunnel in the growth plate in terms of avoiding growth disturbance, although animal and clinical studies have demonstrated the possibility of physeal injury, and therefore, smaller transphyseal tunnels are recommended.
For ACL reconstruction, we prepared a 7-10 mm transphyseal tunnel (tibial tunnel at an angle of 55° and femoral tunnel at the 10:30 or 1:30 clock position). Although we were unable to determine the percentages of entire physis occupied by transphyseal tunnels, they were estimated to range from 10 to 16% of physes diameters on antero-posterior view radiographs. However, no leg length discrepancy of more than 1 cm and no knee malalignment over an average of months of follow-up were observed in our 11 patients.
We conclude that transphyseal ACL reconstruction using a hamstring autograft in skeletally immature adolescents is an effective method of treatment, which achieves regained anterior knee stability. Almost all of our patients returned to their pre-injury sports activity levels, and no case of leg length discrepancy or malalignment was observed.
Figures and Tables
Fig. 1
Roentgenograms of a young patient with a "wide open" skeletally immature physes (A) and of a young patient with a "closing" skeletally mature physes (B).
Fig. 2
Assessment of the knee alignment by using femorotibial angle (A), anatomical lateral distal femoral angle (B), mechanical lateral distal femoral angle (C), mechanical medial proximal tibial angle (D), and posterior distal femoral and posterior proximal tibial angles (E).

Fig. 3
Anteroposterior (A) and lateral (B) radiograms, and an orthoroentgenogram (C) of a 21-yr-old male at 7 yr 5 months postoperatively showing a closed physes and no angular deformity or leg length discrepancy compared with the uninjured right side.

Table 2
Clinical and radiological data of 11 patients
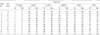
LLD, leg length discrepancy; F-T angle, femorotibial angle; aLDFA, anatomical lateral distal femoral angle; mLDFA, mechanical lateral distal femoral angle; mMPTA, mechanical medial proximal tibial angle; PDTA, posterior distal femoral angle; PPTA, posterior proximal tibial angle; Nr, normal side; Rec, reconstruction side.
References
1. Angel KR, Hall DJ. Anterior cruciate ligament injury in children and adolescents. Arthroscopy. 1989. 5:197–200.

2. Matz SO, Jackson DW. Anterior cruciate ligament injury in children. Am J Knee Surg. 1988. 1:59–65.
3. McCarroll JR, Rettig AC, Shelbourne KD. Anterior cruciate ligament injuries in the young athlete with open physes. Am J Sports Med. 1988. 16:44–47.

4. Micheli LJ. Pediatric and adolescent sports injuries: Recent trends. Exerc Sport Sci Rev. 1986. 14:359–374.
5. Nottage WM, Matsuura PA. Management of complete traumatic anterior cruciate ligament tears in the skeletally immature patient: Current concepts and review of the literature. Arthroscopy. 1994. 10:569–573.

6. Stanitski CL. Anterior cruciate ligament injury in the skeletally immature patient: Diagnosis and treatment. J Am Acad Orthop Surg. 1995. 3:146–158.

7. Sullivan JA. Ligamentous injuries of the knee in children. Clin Orthop Relat Res. 1990. 255:44–50.

8. McCarroll JR, Shelbourne KD, Porter DA, Rettig AC, Murray S. Patellar tendon graft reconstruction for midsubstance anterior cruciate ligament rupture in junior high school athletes. Am J Sports Med. 1994. 22:478–483.

9. Tanner JM, Davies PS. Clinical longitudinal standards for height velocity for North American children. J Pediatr. 1985. 107:317–329.
10. Clanton TO, DeLee JC, Sanders B, Neidre A. Knee ligament injuries in children. J Bone Joint Surg. 1979. 61-A:1195–1201.

11. Lipscomb AB, Anderson AF. Tears of the anterior cruciate ligament in adolescents. J Bone Joint Surg. 1986. 68-A:19–28.

12. Stanitski CL, Harvell JC, Fu F. Observation on acute knee hemarthrosis in children and adolescents. J Pediatr Orthop. 1993. 13:506–510.
13. Aichroth PM, Patel DV, Zorrilla P. The natural history and treatment of rupture of the anterior cruciate ligament in children and adolescents. J Bone Joint Surg. 2002. 84-B:38–41.

14. Bradley GW, Shives TC, Samuelson KM. Ligament injuries in the knee of children. J Bone Joint Surg. 1979. 61-A:588–591.
15. Chick RR, Jackson DW. Tears of the anterior cruciate ligament in young athletes. J Bone Joint Surg. 1978. 60-A:970–973.

16. Graf BK, Lange RH, Fujisaki CK, Landry GL, Saluja RK. Anterior cruciate ligament tears in skeletally immature patients: Meniscal pathology at presentation and after attempted conservative treatment. Arthroscopy. 1992. 8:229–233.

17. Kannus P, Jarvinen M. Knee ligament injuries in adolescents: Eight-year follow-up of conservative management. J Bone Joint Surg. 1988. 70-B:772–776.
18. DeLee JC, Curtis R. Anterior cruciate ligament insufficiency in children. Clin Orthop. 1983. 172:112–118.

19. Brief LP. Anterior cruciate ligament reconstruction without drill holes. Arthroscopy. 1991. 7:350–357.
20. Parker AW, Drez D Jr, Cooper JL. Anterior cruciate ligament injuries in patients with open physes. Am J Sports Med. 1994. 22:44–47.

21. Edwards PH, Grana WA. Anterior cruciate ligament reconstruction in the immature athlete : Long-term results of intra-articular reconstruction. Am J Knee Surg. 2001. 14:232–237.
22. Lo IK, Kirkley A, Fowler PJ, Miniaci A. The outcome of operatively treated anterior cruciate ligament disruptions in the skeletally immature child. Arthroscopy. 1997. 13:627–634.

23. Fuchs R, Wheatley W, Uribe JW, Hechtman KS, Zvijac JE, Schuroff MR. Intra-articular anterior cruciate ligament reconstruction using patellar tendon allograft in skeletally immature patient. Arthroscopy. 2002. 18:824–828.
24. Sobau C, Ellermann A. Anterior cruciate ligament reconstruction with hamstring tendons in young. Unfallchirurg. 2004. 107:676–679.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download