Abstract
A 68-yr-old man complaining of sudden, postprandial chest pain visited the emergency room. His symptom had been aggravated during the preceding two days. Upper gastrointestinal contrast study with gastrographin showed leakage of dye from the epiphrenic diverticulum in the lower third of the esophagus. The primary repair was urgently carried out. Upper gastrointestinal contrast study 14 days after operation revealed an esophageal leakage which was small and confined. The patient was managed with conservative treatments such as intravenous hyperali-mentation and broad-spectrum antibiotics. Forty-two days after the operation, a gastrographin swallow study showed the absence of leaks. This is the first report-ed case of a perforated epiphrenic esophageal diverticulum repaired by delayed primary repair in Korea.
Epiphrenic diverticulum is a rare disease that presents with the primary symptoms of dysphagia and regurgitation (1-3). Esophagitis is the most frequent complication, and bleeding may also occur (4, 5). Perforation is an extremely rare complication of epiphrenic diverticulum. The diagnosis of intrathoracic esophageal perforation is frequently delayed. We report here a patient with perforated epiphrenic diverticulum who was diagnosed 3 days after spontaneous rupture and had a primary repair of his perforation. There are no prior reports of delayed primary repair of a perforated epiphrenic esophageal diverticulum in Korea.
A 68-yr-old man was transferred to the emergency room because of sudden postprandial chest pain, which had been aggravated during the previous two days. He had a history of stroke, hypertension and diabetes mellitus for 3 yr, during which time he had been taking antihypertensive, antiplatelet, and antidiabetic medications. Blood pressure was 110/70 mmHg, pulse 120 bpm, and temperature 39℃. Physical examination demonstrated a subcutaneous emphysema in the neck. Laboratory data included white blood cell count of 16,400/µL, hemoglobin value 11.3 g/dL, and platelet count 273×103/µL. Chest radiograph revealed a small air shadow in the neck (Fig. 1). Chest computed tomography showed periesophageal fluid collection in the lower esophagus, more prominent air collection at the left lateral aspect of the lower esophagus, and bilateral minimal pleural effusion (Fig. 2). The radiologist suggested an esophageal perforation and recommended an esophagogram with gastrographin. The esophagogram revealed a perforation with a bulge of 2.5 cm in width in the lower thoracic esophagus (Fig. 3). The patient was emergently operated on, with primary closure for perforation, and proper drainage with insertion of thoracostomy tubes. At the time of surgery, after esophageal dissection and debridement, a perforated esophageal diverticulum was identified and the perforation was revealed in the borderline between mucosal protrusion and muscular fiber (Fig. 4). The mucosal edge of the perforation was identified and approximated using interrupted 4-0 vicryl sutures, and the muscular edge was closed using interrupted 3-0 silk sutures. The closure was reinforced by stripping a large flap of pleura from the posterolateral thoracic cavity and stitching it to the muscular coat of the esophagus all round the sutured perforation. The chest was closed with two thoracostomy tubes. Despite the use of broad spectrum antibiotics postoperatively, the patient's condition deteriorated and follow-up radiography revealed markedly aggravated pulmonary edema, cardiomegaly, and widened mediastinum (Fig. 5) until the 2nd postoperative day. After using cardiotonic and diuretics, the patient was improved his symptom and radiography. A gastrographin swallow study obtained on the 14th postoperative days showed the disappearance of the diverticulum, although there remained small and confined leak from the esophagus (Fig. 6). The patient was managed with non-surgical treatments, such as intravenous hyperalimentation and broad-spectrum antibiotics. A gastrographin swallow study performed on the 42nd postoperative day showed the absence of leaks, and the patient was discharged 2 months after the operation.
Esophageal diverticula are divided into those in the transition zone between the pharynx and the esophagus (Zenker's diverticula), midesophageal diverticula, and those in the lower third of the esophagus (epiphrenic diverticula). Pulsion diverticula of the epiphrenic portion of the esophagus are not as common as those occurring in the cervical portion.
An epiphrenic diverticulum is generally believed to represent a form of pulsion diverticulum caused by markedly increased intraluminal esophageal pressures associated with underlying esophageal motility disorders such as diffuse esophageal spasm (1, 2, 6, 7). In some studies (6, 8), however, diverticula occurred in the absence of esophageal motor disorders and failed to enlarge when low esophageal sphincter pressures were elevated. These studies suggested that epiphrenic diverticula were not always dependent on an esophageal motor disorder. In the present study esophageal motility was normal on gastrographin study.
An epiphrenic diverticulum should be operated on if symptoms and complications are related to the diverticulum. Esophagitis is the most frequent complication. Dysphagia and regurgitation are the most common symptoms, and bleeding ulceration may also occur. Spontaneous perforation is an extremely rare and serious complication of epiphrenic diverticulum, which has a high mortality and morbidity rate. In esophageal perforation, the gastric contents are expelled into the mediastinum and the pleural cavity as a resulting esophageal injury. The combination of gastric acid and digestive enzymes cause mediastinitis and sepsis, which is fatal in most untreated cases.
Esophageal perforation is not common and has a variety of symptoms, none of which are diagnostic, therefore, there is often a delay in diagnosis. When the esophageal perforation is more than 24 hr old, its treatment remains controversial. Diversion or resection of the esophagus has generally been recommended. Unfortunately, these methods have a high mortality and the disadvantage of needing further reconstructive surgery (9, 10). In 1975, however, Grillo and Wilkins (11) recommended that primary repair should be undertaken for esophageal perforation, regardless of the time interval between perforation and operation. However, postoperative morbidity, including postoperative leakage is a common occurrence after primary repair. These complications can be treated with aggressive and intensive nursing care, early nutritional support, and a proper antibiotic regimen. Therefore, the overall high morbidity rate does not correlate with a high morbidity rate and recently there is increasing evidence that primary repair affords the patient the best probability of survival, regardless of the time interval between esophageal perforation and repair (12, 13)
Most benign strictures or motility disorders may not contraindicate primary closure. However, delayed primary repair of the esophageal perforation is not advisable in all situations. In addition to malignant disease, an esophagus that is severely damaged from certain benign intrinsic conditions (scleroderma, previous caustic burn) or extrinsic trauma (acute lye ingestion, blast injury) may not be primarily repairable (13, 14).
A number autologous tissue flaps have been described to reinforce the repaired esophageal perforation, such as pleural flap, pericardium, diaphragm or muscle flaps (15, 16). It has been suggested that reinforced primary repair should be performed for most thoracic esophageal perforations.
In conclusion, a patient was treated successfully with delayed closure of perforated epiphrenic diverticulum.
Figures and Tables
Fig. 1
Preoperative radiography demonstrates a linear band of air (as shown by the arrow) paralleling to the trachea.

Fig. 2
Chest CT scan reveals periesophageal fluid collection in the lower esophagus, along with air collection around the esophagus.
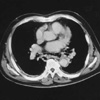
Fig. 3
Upright view from contrast study shows a 2.5 cm-wide diverticulum and leak on the diverticulum in the left distal esophagus.

Fig. 4
During the surgery, epiphrenic diverticulum is observed as a mucosal protrusion between the muscular fibers on the left side of the lower thoracic esophagus. The perforation (as shown by the arrow) is revealed in the borderline between mucosal protrusion and muscular fiber.

References
1. Bruggeman LL, Seaman WG. Epiphrenic diverticula: an analysis of 80 cases. Am J Roentgenol Radium Ther Nucl Med. 1973. 119:266–276.
2. Debas HT, Payne WS, Cameron AJ, Carlson HC. Physiopathology of lower esophageal diverticulum and its implications for treatment. Surg Gynecol Obstet. 1980. 151:593–600.
3. Benacci JC, Deschamps C, Trastek VF, Allen MS, Daly RC, Pairolero PC. Epiphrenic diverticulum: results of surgical treatment. Ann Thorac Surg. 1993. 55:1109–1114.

4. Abul-Khair MH, Khalil A, Mohsen A. Bleeding from an epiphrenic esophageal diverticulum. Eur J Surg. 1992. 158:377–378.
5. Hoxie DA, Dilon MC, Tuckson WB, DeSai RM. Profuse bleeding in epiphrenic diverticula: an unusual finding. J Natl Med Assoc. 1995. 87:373–375.
6. Jordan PH Jr, Kinner BM. New look at epiphrenic diverticula. World J Surg. 1999. 23:147–152.
7. Borri J, Wilson RL. Esophageal diverticula: principles of management and appraisal of classification. Thorax. 1980. 35:759–767.
8. Fasano NC, Levine MS, Rubesin SE, Redfern RO, Laufer I. Epiphrenic diverticulum: Clinical and radiographic findings in 27 patients. Dysphagia. 2003. 18:9–15.

9. Lee YC, Lee ST, Chu SH. New technique of esophageal exclusion for chronic esophageal perforation. Ann Thorac Surg. 1991. 51:1020–1022.

10. Bardini R, Bonavina L, Pavarello M, Asolati M, Peracchia A. Temporary double exclusion of the perforated esophagus using absorbable staples. Ann Thorac Surg. 1992. 54:1165–1167.

11. Grillo HC, Wilkins EW Jr. Esophageal repair following late diagnosis of intrathoracic perforation. Ann Thorac Surg. 1975. 20:387–399.

12. Kim KD, Chung KY, Kim CS, Park HK. Delayed primary repair of esophageal rupture. Korean J Thorac Cardiovasc Surg. 1998. 31:6–51.
13. Wang N, Razzouk AJ, Safavi A, Gan K, Van Arsdell GS, Burton PM, Fandrich BL, Wood MJ, Hill AC, Vyhmeister EE, Miranda R, Ahn C, Gundry SR. Delayed primary repair of intrathoracic esophageal perforation: is it safe? J Thorac Cardiovasc Surg. 1996. 111:114–122.

14. Orringer MB, Stirling MC. Esophagectomy for esophageal disruption. Ann Thorac Surg. 1990. 49:35–43.

15. Richardson JD, Martin LF, Borzotta AP, Polk HC Jr. Unifying concepts in the treatment of esophageal leaks. Am J Surg. 1985. 149:157–162.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download