Abstract
Determining of HER-2/neu oncogene amplification has become clinically important for managing breast cancer. Fluorescent in situ hybridization (FISH) and immunohistochemistry (IHC) are currently regarded as the standard methods. Chromogenic in situ hybridization (CISH) was investigated as a new modification with an accurate, sensitive technique. From 1998 to 2002, using CISH and IHC, the amplification and protein expression of the HER-2/neu oncogene were examined using paraffin sections in 130 breast carcinomas and to determine the prognostic role of HER-2/neu for outcome after a follow-up of 24-64 months. Amplifications by CISH and overexpression by IHC were observed in 28 (22%) and 27 cases (20.8%), respectively. Of the 104 patients, 20 patients (19.2%) with amplification had a shorter disease-free interval (34.9 months vs. 38.0 months in controls) (p=0.372). 15 patients (14.4%) had a disease recurrence, but there is no significant difference between 3 patients amplifying the oncogene and 12 patients without oncogene (20.6 months vs. 19.6 months) (p=0.862). 6 patients (5.8%) of these died. CISH is a useful alternative, particularly for confirming the IHC results. There is no relationship between the early recurrence and the HER-2/neu positive group, but lymph node status was statistically significant.
Slamon et al. (1) first described the association of an amplification of the HER-2/neu gene with an unfavorable outcome in breast cancer in 1987. The HER-2/neu oncogene, which is located on chromosome 17q21, is homologous with, but distinct from, the epidermal growth factor receptor and encodes for a 185-kDa transmembrane glycoprotein that possesses intracellular tyrosine kinase activity (1-6). This gene is amplified and overexpressed in approximately 20-40% of breast cancers (1-7). Amplification and overexpression of the HER-2/neu oncogene correlates with a more aggressive disease as shown by the association with a shorter disease-free and overall survival of women with this alteration (1, 2, 4-6). HER-2/neu amplification and overexpression has been correlated with the responsiveness to adriamycin chemotherapy in addition to a lack of a responsiveness to tamoxifen therapy (7-9). The clinical importance of the HER-2/neu diagnostics has risen even more with the increasing use of the new anti-cancer drug, trastuzumab (Herceptin, Roche Ltd. Basel, Switzerland), a humanized monoclonal antibody to the extracellular domain of HER-2/neu oncoprotein, to treat metastatic breast carcinoma (2, 10-12).
Because of the heightened interest in selecting patients for both adjuvant treatment and Herceptin treatment based on the alterations in the HER-2/neu oncogene, considerable attention has been focused on the accuracy of the clinical assays used to evaluate the level of HER-2/neu amplification and overexpression. Most studies of the HER-2/neu oncogene in breast cancer have used immunohistochemistry (IHC) to evaluate its overexpression. IHC is relatively inexpensive and easy to perform but has a number of shortcomings. The interpretation of IHC is subjective and has been found to vary among observers (13, 14). Fluorescent in situ hybridization (FISH) assays have been used to evaluate the level of gene amplification in paraffin-embedded specimens. These assays are more complicated to perform than IHC and require fluorescence microscopy (15, 16). Chronogenic in situ hytridigation (CISH) was investigated as a new modification and an extremely accurate and sensitive technique, in which a chromosomal DNA probe is detected using an immunohistochemical-like peroxidase reaction (17). CISH offers three important advantages; 1) the histological details of the paraffin section are generally better appreciated with a bright field, 2) the morphological details are readily apparent using low-power objectives, and 3) the probe signals are not subject to rapid fading (17-19). However, CISH analysis has not been extensively studied in breast cancer specimens in contrast to FISH analysis. Therefore, in this study, we analyzed the level of HER-2/neu gene amplification using CISH, and we correlated the findings with IHC in 130 breast cancers specimens obtained from operable patients. And also this study attempted to determine the predictive role of HER-2/neu for the disease-free interval after a follow-up of 24-64 months (mean=40.0 months) in 104 patients.
From 1998 to 2002, 130 consecutive patients with breast cancer were tested for the overexpression of the cell surface oncoprotein by IHC (Novocastra Laboratories, Newcastle, U.K.) and amplification of the HER-2/neu oncogene by CISH (SPOT-LIGHT, Zymed, South San Francisco, CA, U.S.A.). All patients had tissue samples that were initially tested for the HER-2/neu gene product by IHC, which were interpreted independently by three pathologists. The findings with scores of 2+ to 3+ by IHC were considered to be immunopositive (17, 20). If the results were positive, anthracycline-based therapy was given. Because of the possibility of false positive or negative results by IHC, CISH was performed on all samples.
In order to evaluate significant numbers of the tumors, low-density tissue microarrays (TMA) blocks were made at the hospital. The integration of the TMA blocks enabled a high-throughput determination of the level of HER-2/neu amplification with rapidity in large cohorts (21, 22). One block contained 20 cores (single core per tumor), each measuring 3 mm in diameter. Four µm sections were mounted onto the positively charged slides.
A digoxigenin-labeled genomic probe for HER-2/neu was obtained from Zymed (South San Francisco, U.S.A.) and used in CISH, using reagent kits from the same manufacturer. In brief, the sections were deparaffinized and incubated in pretreatment buffer in a temperature-controlled microwave oven (92℃ for 15 min). Enzymatic digestion was carried out with pepsin (at room temperature for 10-30 min). The slides were washed with PBS and dehydrated in graded dilutions of ethanol. The HER-2/neu probe (5-10 µL/slide) was applied to the slides under coverslips. The slides were co-denatured on a hot plate (94℃ for 3 min), followed by overnight hybridization at 37℃. The slides were washed (0.5× SSC for 5 min), and the hybridized probe was detected using the CISH detection reagents (anti-digoxigenin-FITC, anti-FITC-peroxidase, and diaminobenzidine as chromogen), according to the manufacturer's instructions. The sections were counterstained with hematoxylin and mounted. The slides were analyzed by 3 of us using an ordinary transmitted light microscope under 20× objective. Generally, 1-4 copies were considered as no amplification, 5-8 as low-level amplification and >8 gene copies as high-level amplification (23). Amplification was defined when greater than 5-10 discrete copies per nucleus or large gene copy clusters in at least 50% of cancer cells were seen, as described by Tanner et al. (15).
Deparaffinized tissue sections were heat pretreated in sodium citrate buffer (pH 7.3, at 92℃ for 20 min in a temperature-controlled microwave oven) and immunostained with a labeled monoclonal antibody to the intracellular domain of HER-2/neu protein (CB-11; Novocastra Laboratories, Newcastle, U.K.). A standard avidin-biotin-peroxidase complex (ABC) technique was used for visualization, with diaminobenzidine as the chromogen (Histostain Plus-kit; Zymed). There are several methods of interpreting cells stained by IHC. The most common scoring system is recommended in the Hercep Test manufacturer's protocol (24), but this has practical difficulties and is opened to interpretation errors, particularly around the subjective IHC 2+/3+ cutoff point. DAKO (the manufacturer of the Hercep Test) have recently modified their recommendations and propose FISH testing of all IHC 2+ tumors (24). The Finnish and Swedish guidelines advocate retesting all IHC 2+ and 3+ samples by in situ hybridization, diminishing the need to make a distinction between these two groups (25). Because the concordance between IHC at the 2+ level and FISH can be as low as 25% and the concordance between IHC 3+ and FISH is around 90% (25-28), only an intense cell membrane immunoreaction present in >50% of cancer cells (IHC 3+) was considered as overexpression of HER-2 protein (25, 29) (Fig. 1).
Statistical analysis was performed using SPSS for Windows (Version 10.0; SPSS, Chicago, IL. U.S.A.). Test-retest reliability was assessed using Spearman correlation. Comparison of survival between two groups was made by independent-samples t test. Statistical significance for variables, age, tumor size, lymph node status and HER-2/neu amplification by CISH and survival was examined using the multivariate test. A p-value of <0.05 was considered significant.
Amplification was seen most often as large gene copy clusters in the majority of nuclei (Fig. 2). Of the 130 breast carcinomas, amplifications of the HER-2/neu oncogene by CISH were observed in 28 cases (22%), and the HER-2/neu protein overexpression was identified by IHC in 27 cases (20.8%) (concordance rate: 94.96%) (Table 1). The tumors from 15 (11.5%) patients showed both amplification and overexpression, while 12 (9.2%) tumors displayed overexpression without amplification and 3 (2.3%) tumors displayed amplification without overexpression. Non-amplified tumors showed 1 to 3 clearly defined dots in the nucleus (Fig. 3).
Twenty-six patients were excluded from outcome analysis because of a short follow-up time (less than 2 yr). The remaining 104 patients were analyzed for disease-free survival. The mean follow-up period was 40.0 months. Of the 104 patients, 20 patients (19.2%) with oncogene amplification had a shorter median disease-free survival (34.9 months) compared to the controls (38.0 months), but statistically insignificant (p=0.871) (Table 2). There is no relationship between the early recurrence (shortened disease-free interval) and patient's age and tumor size, but lymph node status was statistically significant (p=0.010). Of the 104 patients, 15 patients (14.4%) had a disease recurrence, and 6 patients (5.8%) of these died of multifocal metastases.
Clinicopthological characteristics of 15 recurred patients were shown in Table 3. The mean age at the time of initial diagnosis was 46.3 yr (range: 31-65 yr) and mean tumor size was 3.8 cm (range: 1.0-9.0 cm). All patients were diagnosed as infiltrating ductal carcinoma, and some of them were associated with apocrine carcinoma, micropapillary, papillary, ductal carcinoma in situ and Paget's disease. All cases except one were observed evidence of lymph node metastases. 6 cases (40%) metastasized to the bone, and also lung, subclavian lymph node, thyroid and brain metastases were found. A mean disease-free survival between 3 patients amplifying the oncogene (20.6 months) and 12 patients without oncogene (19.6 months) revealed insignificant difference (p=0.862).
Thirty-six patients (27.7%) and 94 patients (72.3%) were treated by lumpectomy with axillary node dissection and modified radical mastectomy, respectively. The patients also received adjuvant therapy depending on the type of surgery and nodal status. Breast irradiation was systematically performed in 44 patients, but the chest wall irradiation was performed only on 2 patients with positive axillary nodes that were treated with a mastectomy. One hundred and five of the 130 patients (80.7%) received adjuvant chemotherapy after surgery. Twenty patients were given tamoxifen alone (18 negative for HER-2/neu and 2 positive by CISH) and 85 patients were given systemic chemotherapy (65 negative for HER-2/neu and 20 positive by CISH), consisting either of CMF (cyclophosphamide, methotrexate, 5-fluorouracil) or FAC (5-fluorouracil, adriamycin, cyclophosphamide). Sixty patients received doxorubicin-based regimens, of whom 46 tested negative for the HER-2/neu oncogene, and 14 tested positive by CISH. If the results were positive (2+ or 3+) by IHC, anthracycline-based adjuvant chemotherapy was performed in our patients. Because IHC 3+ was considered as overexpression of HER-2 protein, some differences between the number of doxorubicin-treated patients and case number of overexpression (IHC 3+).
HER-2/neu amplification must occur very early in the genetic cascade, at least before the dissemination of the cancerous cells (3, 7, 30). The patients with HER-2/neu positivity have a poor prognosis, including a shortened disease-free survival and overall survival, in contrast to HER-2/neu negative patients (6, 12). Previous studies have shown that HER-2/neu overexpression is significantly associated with an increased risk of an earlier relapse and death (6, 31, 32). However, other studies have not demonstrated this relationship (14). There is no consensus in the literature concerning the clinical significance of the amplification of this oncogene. In this study, patients with an oncogene amplification had a shorter median disease-free interval (34.9 months) compared to the controls (38.0 months), but statistically insignificant (p=0.871). Of the 15 recurred patients, a mean disease-free survival between 3 patients amplifying the oncogene (20.6 months) and 12 patients without oncogene (19.6 months) revealed insignificant difference (p=0.862). This study suggests there is no relationship between the early recurrence (shortened diseasefree interval) and the HER-2/neu positive group. No association was found between the gene amplification and the tumor grade, the ER/PR status, or the lymph node status (6). But, this study revealed that correlation between survival rate and lymph node status was statistically significant. HER-2/neu status should not be used to determine whether or not a woman should receive adjuvant systemic therapy and whether or not a patient should receive endocrine therapy (3, 33). Riou et al. (4) showed that HER-2/neu amplification had a similar prognostic value on patients regardless of whether they received these treatments or not. If a specific patient's tumor overexpresses HER-2/neu and adjuvant chemotherapy is recommended, an anthracycline-containing regimen may be preferable. In contrast, for women whose tumors do not overexpress HER-2/neu, adjuvant therapy with either a CMF-like or anthracycline-containing regimen appears to be similar (5). Herceptin therapy is effective only in the HER-2/neu positive patients and produces a significant survival benefit in patients with HER-2/neu positive metastatic breast cancer (2, 3, 12, 33).
There are several methods for determining the HER-2/neu status. IHC is widely available and most laboratories have experience using this technique. Furthermore, this technique is quite reliable when performed by experienced laboratories following established protocols (20). However, previous reports, and U.S. Food and Drug Administration-approved IHC assay have shown that the method and reproducibility of IHC for determining the HER-2/neu gene product was inaccurate in identifying women who are likely to respond to treatment with Herceptin (6, 24, 34). A deterioration of the antigenicity over time is causative (4, 20). The factors that can lead to inaccuracies in the HER-2/neu testing results include preparation, fixation, and storage of the tissue sections; the antibody or probe used to detect the HER-2/neu oncogene; the scoring or result interpretation; the lack of validated methodologies; the experience of the personnel; and the inter-observer variability (20, 25, 35). FISH has also been shown to provide reliable and accurate information (15, 16, 36). DAKO recommended the use of FISH testing to determine HER-2/neu status in equivocal circumferences, particularly in all IHC 2+ tumors (24). Although not all laboratories currently have the equipment necessary to conduct and quantify FISH assays, their use is becoming more widespread. CISH also has the advantage of revealing the tissue histopathology, which was found to be particularly useful when analyzing the metastatic tumor lesions (3). Metastases often contain only small foci of cancer cells, which are difficult to find using FISH with dark-field fluorescence microscopy. Gene amplification detected by CISH is 91.0% concordant with the results obtained using FISH (37). In the present study, a poor correlation in IHC 2+ and 3+ tumors has been found compared to the negative groups (IHC 0 and 1+). Controversy still exists as to whether cases that show 1+ or 2+ staining. The overall standardization for determining and interpreting HER-2/neu by IHC is still a critical issue with many investigators and clinicians.
Although CISH is more difficult to apply in routine practice than IHC, we recommended for clinical application as a complementary test for confirming the IHC results and selecting the patients for Herceptin treatment. In present study, there is no relationship between the early recurrence and the HER-2/neu positive group, but lymph node status was statistically significant.
Figures and Tables
Fig. 1
Immunohistochemical staining for HER-2/neu oncogene shows strong, complete membrane staining (score 3+), ×200.
Fig. 2
A typical high-level HER-2/neu amplification appears multiple large clusters of gene copies by chromogenic in situ hybridization. Counterstained with hematoxylin, ×200.

Fig. 3
No amplification by chromogenic in situ hybridization shows one to two clearly identifiable copies of HER-2/neu gene. Counterstained with hematoxylin, ×200.
Table 1
Correlation between amplification by CISH and overexpression by IHC for HER-2/neu in 130 breast carcinomas
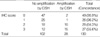
Table 2
Multivariate analysis of age, tumor size, lymph nodes and HER-2/neu oncogene amplification by CISH for survival rate in 104 follow-up cases

Table 3
Clinicopatholigical characteristics and follow-up of 15 recurred patients

*IHC, HER-2/neu overexpression by immunohistochemistry; CISH, HER-2/neu amplification by chromogenic in situ hybridization; Size, Tumor size; LN, Lymph node metastases (number of metastatic node/number of dissected node); FU, Follow-ups; DFS ms., Disease-free survival months; IFD 1, 2 & 3, Infiltrating ductal carcinoma, grade 1, 2 & 3; Apoca, Apocrine carcinoma; mp, micropapillary type; pp, papillary type; DCIS, Ductal carcinoma in situ; Paget's d, Paget's disease; SCL, Subclavian lymph node; meta, metastasis; D, Died.
ACKNOWLEDGMENT
The authors wish to acknowledge the technical assistance of Heechul Lee at Our Lady Mercy Hospital.
References
1. Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL. Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science. 1987. 235:177–182.

2. Vogel CL, Cobleigh MA, Tripathy D, Gutheil JC, Harris LN, Fehrenbacher L, Slamon DJ, Murphy M, Novotny WF, Burchmore M, Shak S, Stewart SJ, Press M. Efficacy and safety of trastuzumab as a single agent in first-line treatment of HER2-overexpressing metastatic breast cancer. J Clin Oncol. 2002. 20:719–726.

3. Tanner M, Jarvinen P, Isola J. Amplification of HER-2/neu and Topoisomerase IIα in primary and metastatic breast cancer. Cancer Res. 2001. 61:5345–5348.
4. Riou G, Mathieu MC, Barrois M, Le Bihan ML, Ahomadegbe JC, Benard J, Le MG. c-erbB-2 (HER-2/neu) gene amplification is a better indicator of poor prognosis than protein over-expression in operable breast cancer patients. Int J Cancer. 2001. 95:266–270.
5. Yamauchi H, Stearns V, Hayes DF. When is a tumor marker ready for prime time? A case study of c-erbB-2 as a predictive factor in breast cancer. J Clin Oncol. 2001. 19:2334–2356.

6. Carr JA, Havstad S, Zarbo RJ, Divine G, Mackowiak P, Velanovich V. The association of HER-2/neu amplification with breast cancer recurrence. Arch Surg. 2000. 135:1469–1474.

7. Ross JS, Fletcher JA. HER-2/neu (c-erbB-2) gene and protein in breast cancer. Am J Clin Pathol. 1999. 112:Suppl 1. S53–S67.
8. Gupta D, Middleton LP, Whitaker MJ, Abrams J. Comparison of fluorescence and chromogenic in situ hybridization for detection of HER-2/neu oncogene in breast cancer. Am J Clin Pathol. 2003. 119:381–387.

9. Baselga J. Herceptin alone or in combination with chemotherapy in the treatment of HER2-positive metastatic breast cancer: pivot trials. Oncology. 2001. 61:Suppl 2. 14–21.
10. Pegram MD, Konecny G, Slamon DJ. The molecular and cellular biology of HER-2/gene amplification/overexpression and the clinical development of Herceptin (trastuzumab) therapy for breast cancer. Cancer Treat Res. 2000. 103:57–75.
11. Ross JS, Gray K, Gray GS, Worland PJ, Rolfe M. Anticancer antibodies. Am J Clin Pathol. 2003. 119:472–485.

12. Slamon D, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, Fleming T, Eiermann W, Wolter J, Pegram M, Baselga J, Norton L. Use of chemotherapy plus a monoclonal antibody against HER-2 for metastatic breast cancer that overexpresses HER-2. N Engl J Med. 2001. 344:783–792.

13. Rhodes A, Jasani B, Anderson E, Dodson AR, Balaton AJ. Evaluation of HER-2/neu immunohistochemical assay sensitivity and scoring on formalin-fixed and paraffin-processed cell lines and breast tumors. A comparative study involving results from laboratories in 21 countries. Am J Clin Pathol. 2002. 118:408–417.
14. Barnes DM, Lammie GA, Millis RR, Gullick WL, Allen DS, Altman DG. An immunohistochemical evaluation of c-erbB-2 expression in human breast carcinoma. Br J Cancer. 1988. 58:448–452.

15. Tanner M, Gancberg D, Di Leo A, Larsimont D, Rouas G, Piccart MJ, Isola J. Chromogenic in situ hybridization. A practical alternative for fluorescence in situ hybridization to detect HER-2/neu oncogene amplification in archival breast cancer samples. Am J Pathol. 2000. 157:1467–1472.
16. Tubbs R, Skacel M, Pettay J, Powell R, Myles J, Hicks D, Sreenan J, Roche P, Stoler MH, Hainfeld J. Interobserver interpretative reproducibility of GOLDFISH, a first generation gold-facilitated autometallographic bright field in situ hybridization assay for HER-2/neu amplification in invasive mammary carcinoma. Am J Surg Pathol. 2002. 26:908–913.

17. Kumamoto H, Sasano H, Taniguchi T, Suzuki T, Moriya T, Ichinohasama R. Chromogenic in situ hybridization analysis of HER-2/neu status in breast carcinoma: application in screening of patients for trastuzumab (Herceptin) therapy. Pathol Int. 2001. 51:579–584.
18. Dandachi N, Dietze O, Hauser-Kronberger C. Chromogenic in situ hybridization: a novel approach to a practical and sensitive method for the detection of HER-2 oncogene in archival human breast carcinoma. Lab Invest. 2002. 82:1007–1014.

19. Zhao J, Wu R, Au A, Marquez A, Yu Y, Shi Z. Determination of HER-2/neu gene amplification by chromogenic in situ hybridization (CISH) in archival breast carcinoma. Mod Pathol. 2002. 15:657–665.
20. Bast RC, Ravdin P, Hayes DF, Bates S, Fritsche H Jr, Jessup JM. 2000 update of recommendations for the use of tumor markers in breast and colorectal cancer: clinical practice guidelines of the American Society of Clinical Oncology. J Clin Oncol. 2001. 19:1865–1878.

21. Hsu FD, Nielsen TO, Alkushi A, Dupuis B, Huntsman D, Liu CL, van de Rijn M, Gilks CB. Tissue microarrays are an effective quality assurance tool for diagnostic immunohistochemistry. Mod Pathol. 2002. 15:1374–1380.

22. Zhang D, Salto-Tellez M, Putti TC, Do E, Koay ES. Reliability of tissue microarrays in detecting protein expression and gene amplification in breast cancer. Mod Pathol. 2003. 16:79–84.

23. van de Vijver M. Emerging technologies for HER 2 testing. Oncology. 2002. 63:Suppl 1. 33–38.
24. Jacobs TW, Bown AM, Yaziji H, Barnes MJ, Shinitt SJ. Specificity of Hercep Test in determining HER-2/neu status of breast cancers using the United States Food and Drug Administration-approved scoring system. J Clin Oncol. 1999. 17:1983–1987.
25. Bilous M, Dowsett M, Hanna W, Isola J, Lebeau A, Moreno A, Penault-Llorca F, Ruschoff J, Tomasic G, van de Vijver M. Current perspectives on HER 2 testing: A review of national testing guidelines. Mod Pathol. 2003. 16:173–182.
26. Jimenez RE, Wallis T, Tabasczka P, Visscher DW. Determination of HER-2/neu status in breast carcinoma: comparative analysis of immunohistochemistry and fluorescent in situ hybridization. Mod Pathol. 2000. 13:37–45.

27. Ridolfi RL, Jamehdor MR, Arber JM. HER-2/neu testing in breast carcinoma : a combined immunohistochemical and fluorescence in situ hybridization approach. Mod Pathol. 2000. 13:866–873.
28. Wang S, Saboorian MH, Frenkel E, Hynan L, Gokaslan ST, Ashfaq R. Laboratory assessment of the status of HER-2/neu protein and oncogene in breast cancer specimens: comparison of immunohistochemistry assay with fluorescence in situ hybridization assays. J Clin Pathol. 2000. 53:374–381.
29. Lee TJ, Oh HG, Kwon GY, Kim MK, Park ES, Yoo JH. HER-2/neu oncogene amplification by chromogenic in situ hybridization and immunohistochemical expression of Topoisomerase II-α in the breast cancer. Korean J Pathol. 2003. 37:26–34.
30. Latta EK, Tjan S, Parkes RK, O'Malley FP. The role of HER2/neu overexpression/amplification in the progression of ductal carcinoma in situ to invasive carcinoma of the breast. Mod Pathol. 2002. 15:1318–1325.

31. Dolan J, Curran B, Henry K, Lindley R, Leader M. C-erbB-2 protein expression and survival in breast carcinoma [abstract]. J Pathol. 1989. 158:354A.
32. Sjogren S, Inganas M, Lindgren A, Holmberg L, Bergh J. Prognostic and predictive value of c-erbB-2 overexpression in primary breast cancer, alone and in combination with other prognostic markers. J Clin Oncol. 1998. 16:462–469.
33. Burstein HJ, Harris LN, Gelman R, Lester SC, Nunes RA, Kaelin CM, Parker LM, Ellisen LW, Kuter I, Gadd MA, Christian RL, Kennedy PR, Borges VF, Bunnell CA, Younger J, Smith BL, Winer EP. Preoperative therapy with trastuzumab and paclitaxel followed by sequential adjuvant doxorubicin/cyclophosphamide for HER2 overexpressing stage II or III breast cancer: a pilot study. J Clin Oncol. 2003. 21:46–53.

34. Roche PC, Ingle JN. Increased HER-2 with U.S. Food and Drug Administration-approved antibody. J Clin Oncol. 1999. 17:434.

35. Cell Markers and Cytogenetics Committees College of American Pathologists. Clinical laboratory assays for HER-2/neu amplification and overexpression: quality assurance, standardization, and proficiency testing. Arch Pathol Lab Med. 2002. 126:803–808.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download