Abstract
Background and Objectives
To investigate the impact of age on arterial stiffness and blood pressure (BP) variables in newly diagnosed untreated hypertension (HT).
Subjects and Methods
A total of 144 patients with newly diagnosed untreated HT were divided into two groups: young group (age ≤50 years, n=71), and old group (age >50 years, n=73). BP variables were measured on office or 24 hours ambulatory BP monitoring (ABPM). Parameters of arterial stiffness were measured on pulse wave velocity (PWV). Pulse wave analysis (PWA) was compared.
Results
Although office BP and pulse pressure (PP) were significantly (p<0.05) higher in the young group than in the old group, BP and PP on ABPM were not significantly different. Central systolic BP and PP, augmentation pressure, augmentation index on PWA, and PWV were significantly higher or faster in the old group compared to that in the young group. Age showed significant positive correlation with both PWV and PWA variables in the young group with HT. However, age only showed significant positive correlation with PWV in the old group with HT. In the young group with HT, PWA variable showed better correlation with age than PWV.
Conclusion
Considering BP levels on ABPM, office BP is prone to be overestimated in young patients with HT. Parameters of arterial stiffness measured by PWV and PWA were more affected by age rather than by BP level in patients with HT. Therefore, PWA variable might be a more sensitive marker of arterial stiffness in young patients with HT. However, PWV might be a better marker for old patients with HT.
Hypertension (HT), defined as sustained elevation of brachial blood pressure (BP), is a well-known risk factor for all-cause mortality, cardiovascular morbidity, and mortality.1) Previous studies have shown that optimal treatment for HT can decrease cardiovascular events such as stroke and heart failure.2) However, many patients with HT on office BP measurements are not truly hypertensive. They are so called white coat HT (WCH). Therefore, recent guideline for the management of HT recommends 24 hours ambulatory BP monitoring (ABPM) or home BP monitoring to identify patients with true HT before initiating anti-hypertensive therapy.3) ABPM is also useful for the identification of non-dipper associated with stroke, target organ damage, and other cardiovascular events.4)5)6)7) Therefore, ABPM is an important tool not only for the diagnosis of true HT, but also for risk stratification or clinical decision making of therapeutic strategy for patients with HT.8)9)
Arterial stiffness is now an established risk factor and prognostic indicator of cardiovascular disease or events. It can be non-invasively evaluated by measuring pulse wave velocity (PWV) and pulse wave analysis (PWA).10) PWV is associated with future cardiovascular events in HT11) in the elderly12)13) or end-stage renal disease,14)15) even in the general population.16)17) Central aortic pressure and its related variables can be reliably measured by PWA to predict cardiovascular events more accurately than brachial pressures in hypertensive patients.18)19) Although both HT and age are associated with parameters of arterial stiffness, the impact of age on arterial stiffness in patients with newly diagnosed untreated HT has been poorly evaluated. Furthermore, the differences between office BP measurement and 24 ABPM according to age were poorly evaluated. Therefore, the aim of the present study was to investigate age related differences on parameters of arterial stiffness in patients with true HT on 24 hours ABPM who were suspected of HT on office BP measurements.
Among 176 patients who were suspected of HT on office BP measurements, a total of 147 patients had true HT on 24 hours ABPM. Of the 147 patients, 3 who did not have PWV or PWA measurements were excluded. Therefore, a total of 144 patients were included in this study. They were divided into two groups: young group (age ≤50 years, 71 patients, 42 males, mean age of 35.7±9.8 years), and old group (age >50 years, 73 patients, 34 males, mean age of 60.9±7.9 years). Vascular age is usually accelerated after menopause. The mean age of menopause in Korea is 49.7 years. Therefore, the age of 50 years was used as cut-off value for grouping in the present study. This study was a single center, prospective, and observational study. The study protocol was approved by the Institutional Review Board of our institution. Patients who agreed to participate in the present study and gave informed consent were enrolled. Exclusion criteria were: 1) prior history of coronary intervention or myocardial infarction, 2) significant arrhythmias including atrial fibrillation, 3) combined cardiac diseases including significant valvular heart diseases, cardiomyopathy, or heart failure, 4) known renal insufficiency, 5) medication history that might affect BP levels, 6) peripheral vascular disease with ankle-brachial index <0.9, 7) vasculitis disorders, and 8) major life threatening illness.
The definition of HT was complied with the current guideline.3) Systolic BP ≥140 mm Hg and/or diastolic BP ≥90 mm Hg was defined as HT on office BP measurement and 24 hours average systolic BP ≥130 mm Hg and/or diastolic BP ≥80 mm Hg was defined as HT on ABPM in the present study.
Office BP was measured in triplicates at brachial artery of the non-dominant arm by using optimal cuff and mercury sphygmomanometer after at least 10 minutes of resting in seated position. ABPM was recorded using a validated oscillometric device (TONOPORT V, firmware Version 1.4, GE Medical systems, Berlin, Germany). The device allowed automatic measurement of BP every 15 minutes from 7 a.m. to 10 p.m. and every 30 minutes from 10 p.m. to 7 a.m.
Pulse wave velocity was measured non-invasively by using commercially available VP-2000 (Colins, Kyoto, Japan). PWV measurements were performed by a single well-trained clinical technician at supine position in a quiet and temperature controlled room after at least 10 minutes of rest. Heart-femoral PWV (hfPWV) and brachial-ankle PWV (baPWV) were measured and used for analysis. Arterial waveforms and central BPs were obtained by using SphygmoCor PWA device (AtCor Medical, Sydney, Australia). After obtaining radial arterial waveform by using applanation tonometry, the central aortic pressure parameters including central aortic systolic and diastolic BP, augmentation pressure (AP), and augmentation index (AI) were obtained by using computerized transfer function. AP was defined by the difference between aortic systolic pressure and inflection pressure. AI was calculated as {AP/aortic pulse pressure (PP)}×100.
The differences of categorical variables were evaluated by chi-square test. Continuous variables were compared using independent t-test. Pearson's correlation coefficients were used to explore bivariate association between examined variables. Statistical Package for the Social Sciences (SPSS) for Windows, version 18.0 (SPSS Inc., Chicago, IL, USA) was used for all analyses. Data are presented as percents or mean±standard deviation. Statistical significance was considered when p was less than 0.05.
The baseline characteristics were summarized in Table 1. Office systolic and diastolic BP and PP were significantly (p<0.05) elevated in the young group than in the old group. The level of cholesterol was significantly (p<0.05) elevated in the old group than in the young group.
The differences of BP measurements between the two groups were summarized in Table 2. Office systolic and diastolic BP and PP were significantly (p<0.05) higher in the young group than in the old group. However, BP measurements on 24 hours ABPM were not significantly different between the groups. Overall, the difference of systolic BP between office and 24 hours ABPM (office systolic BP-systolic BP on 24 ABPM) showed significant negative correlation with age (r=-0.320, p<0.001) (Fig. 1).
The differences of parameters of arterial stiffness between the two groups were summarized in Table 3. Central systolic BP, PP, AP, and AI on PWA were significantly (p<0.05) higher in the old group than in the young group. However, central diastolic BP was not significantly different between the two groups. HfPWV and baPWV were significantly (p<0.05) faster in the old group than in the young group (Table 3).
Overall, age showed significant positive correlation with hfPWV (r=0.617, p<0.001) and baPWV (r=0.598, p<0.001) (Fig. 2). Age also showed significant positive correlation with central systolic BP (r=0.287, p=0.009) and PP (r=0.414, p<0.001). AP and AI also showed significant positive correlation with age (r=0.549, r=0.544, p<0.001, respectively) (Fig. 3). However, central diastolic BP did not show correlation with age (r=-0.030, p>0.05).
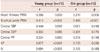
The correlation of parameters of arterial stiffness with age between the two groups were summarized in Table 4. In the young HT group, age showed significantly positive correlation with hfPWV, baPWV, AP, AI, and central systolic BP. However, central diastolic BP and PP did not show correlation with age. In the old HT group, age showed significant positive correlation with hfPWV and baPWV. However, PWA variables did not show any correlation with age.
The present study evaluated the impacts of age on parameters of arterial stiffness and BP in patients with newly diagnosed untreated HT. The results of the present study demonstrated several important findings. Firstly, office BP measurement considering BP levels on 24 hours ABPM is prone to be overestimated in young HT patients than in old HT patients. Secondly, peripheral BP measurements cannot reflect central BP indices appropriately, especially in young HT patients. Thirdly, in HT patients, parameters of arterial stiffness are more significantly affected by age rather than the levels of BP. Fourthly, AP and AI showed better correlation with age than PWV in the young HT group. However, age showed significant positive correlation only with PWV in the old HT group.
As in WCH, office BP is usually greater than home BP or ambulatory BP in most HT patients. This phenomenon of difference between office BP and average daytime ambulatory BP or home BP in patients with HT is called white-coat effect (WCE).20) WCH or WCE is a relatively common finding in patients with elevated BP. Previous studies have shown that WCH were more prevalent among non-smokers, females, and older age.21)22) In contrary to these studies, young age was found to be an independent predictor of WCH in a study of Pickering et al.23) and Pickering.24) Results of the present study were consistent with the study of Pickering et al.23) and Pickering24) except that the present study was conducted only in patients with HT. Although BP levels on 24 ABPM were not different between the two groups in the present study, office BP was significantly greater in young HT patients than in old HT patients, suggesting that WCE in young HT patients has a higher prevalence. Park et al.25) using Korean subjects found that age was not a predictor of WCH. To clarify the issue regarding the impact of age on WCE among HT patients, further controlled study with a larger population is merited.
Central BP is defined as the BP of the aorta and carotid artery. Aortic pressure reflects afterload of the heart. Diastolic aortic pressure is a major determinant of coronary perfusion. Theoretically, central BP would be a better predictor of future cardiovascular events than brachial BP. The results of Strong Heart Study26) support this hypothesis by demonstrating that central aortic PP and arterial stiffness are more strongly related to vascular hypertrophy and the extent of carotid atherosclerosis than brachial pressure. Furthermore, central PP was a better predictor of future cardiovascular outcome than brachial PP in the Strong Heart Study.26) In the present study the relationship between peripheral BP and central BP according to the age group of HT patients was evaluated. Although central systolic BP was lower in the young HT group than in the old HT group, peripheral systolic BP was significantly higher in the young group than in the old group in the present study. This observation might be explained by the phenomenon called "pressure wave amplification." As the pulse wave propagated from the central aorta to the peripheral arterial tree, diastolic and mean BP did not change significantly across the arterial tree. However, systolic BP could be significantly amplified, the so called "pressure wave amplification".27) Because this phenomenon is more common and marked in young people than in old people, the peripheral systolic BP might be significantly higher in the young HT group than in the old HT group in the present study. Results of the present study suggested that peripheral BP was prone to be overestimated in young HT patients than in old HT patients. Our results also suggested that the measurement of peripheral BP might not reflect central hemodynamics that is more closely associated with actual cardiovascular risk in young HT patients. Therefore, to evaluate actual cardiovascular risk, it would be advisable to measure central hemodynamics before initiating antihypertensive therapy, especially for young HT patients.
Arterial stiffness, an established risk factor of cardiovascular disease, is one of the best prognostic indicators of future cardiovascular events in HT patients.10)11)12)13)14)15)16)17) Both age and BP levels are well known major determinants of arterial stiffness. However, the impact of age on parameters of arterial stiffness among HT patients has been poorly studied. Although the level of peripheral BP was higher in the young HT group than in the old HT group, PWV was significantly faster and AI or AP was significantly higher in the old HT group. The results of the present study suggested that parameters of arterial stiffness were more significantly affected by age rather than the level of BP in patients with untreated HT. The correlation of parameters of arterial stiffness with age were different between the two groups in the present study. In the young HT group, both PWV and PWA variables showed significant positive correlation with age. In addition, PWA variables such as AI and AP showed better correlation with age than PWV variables. However, in the old HT group, age only showed significant positive correlation with PWV in the present study. These findings are quite similar to the results of Anglo-Cardiff Collaborative Trial (ACCT) except that the study population of the ACCT was healthy and normotensive individuals.28) The results of ACCT suggested that AI might be a more sensitive marker for arterial stiffening and risk in young individuals, but aortic PWV might be a better measure for old individuals.26) The results of the present study suggested that PWA variables might be a more sensitive marker of arterial stiffness and risk in young HT patients, but PWV would be a better marker of arterial stiffness in old HT patients.
The present study has potential limitations. Firstly, the number of study population was relatively small. Thus, it may result in selection bias that might affect statistical analysis. Secondly, although the present study enrolled patients with newly diagnosed untreated HT without known major cardiovascular diseases, the presence of atherosclerotic cardio-cerebro-vascular disease associated with arterial stiffness cannot be completely excluded. Thirdly, the results of BP measurement, especially in 24 ABPM, might be affected by different degree of physical activity or other factors. Fourthly, TONOPORT V was used for 24 ABPM measurements in the present study because this device was the only available device in our institution during the study period. However, the accuracy of this device is not well validated. Thus, the device used might be a limitation of the present study. Fifthly, male was predominant in the young group and female was predominant in the old group, even though the gender distribution was not different statistically. Because PWV or PWA data can be affected by body habitus, the gender difference between the two groups is another limitation of the present study. Sixthly, the prevalence of left ventricular hypertrophy on electrocardiography was higher in the young group than in the old group, even though it was not statistically different. To clarify this discrepancy, other surrogate markers of target organ damage such as the degree of microalbuminuria should be addressed. However, other surrogate markers of target organ damage were not evaluated in the present study. Therefore, it is another major limitation of the present study.
In conclusion, the results of the present study suggested that office BP, considering BP levels on 24 ABPM, is prone to be overestimated in young HT patients than in old HT patients, suggesting that WCE has a higher prevalence in young HT patients. The parameters of arterial stiffness measured by PWV and PWA were more affected by age rather than BP level among HT patients. PWA variables might be a more sensitive marker for arterial stiffness in young HT patients, but PWV might be a better marker for old HT patients.
Figures and Tables
Fig. 1
Correlation of the difference of systolic blood pressure (ΔSBP) on office or 24 hours ambulatory blood pressure measurements with age in patients with hypertension. Age showed significant negative correlation with ΔSBP.
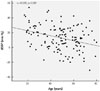
Fig. 2
Correlation of heart-femoral (hfPWV) (A) and brachial-ankle pulse wave velocity (baPWV) (B) with age in patients with hypertension. Age showed significant positive correlation with both hfPWV and baPWV in patients with hypertension.

Fig. 3
Correlation of augmentation pressure (AP) (A) and augmentation index (AI) (B) with age in patients with hypertension. Age showed significant positive correlation with both AP and AI in patients with hypertension.

Table 1
Baseline clinical characteristics between the young and old group

Young group: age ≤50 years, Old group: age >50 years. SBP: systolic blood pressure, DBP: diastolic blood pressure, PP: pulse pressure, LDL-C: low density lipoprotein-cholesterol, HDL-C: high density lipoprotein-cholesterol, hs-CRP: high sensitivity C-reactive protein, LVH: left ventricular hypertrophy, ECG: electrocardiography
Table 2
Differences of blood pressure variables between the young and old group
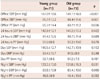
Table 3
Differences of parameters of arterial stiffness between the young and old group
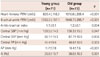
Table 4
Correlation of parameters of arterial stiffness with age in each group
References
1. Rutan GH, Kuller LH, Neaton JD, Wentworth DN, McDonald RH, Smith WM. Mortality associated with diastolic hypertension and isolated systolic hypertension among men screened for the Multiple Risk Factor Intervention Trial. Circulation. 1988; 77:504–514.
2. Turnbull F. Blood Pressure Lowering Treatment Trialists' Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003; 362:1527–1535.
3. McManus RJ, Caulfield M, Williams B. National Institute for Health and Clinical Excellence. NICE hypertension guideline 2011: evidence based evolution. BMJ. 2012; 344:e181.
4. Staessen JA, Bieniaszewski L, O'Brien E, et al. Nocturnal blood pressure fall on ambulatory monitoring in a large international database. The "Ad Hoc' Working Group. Hypertension. 1997; 29(1 Pt 1):30–39.
5. Phillips RA, Butkevich A, Sheinart KF, Tuhrim S. Dipping is superior to cusums analysis in assessment of the risk of stroke in a case-control study. Am J Hypertens. 2001; 14(7 Pt 1):649–652.
6. Verdecchia P, Schillaci G, Borgioni C, Ciucci A, Pede S, Porcellati C. Ambulatory pulse pressure: a potent predictor of total cardiovascular risk in hypertension. Hypertension. 1998; 32:983–988.
7. Zweiker R, Eber B, Schumacher M, Toplak H, Klein W. "Non-dipping" related to cardiovascular events in essential hypertensive patients. Acta Med Austriaca. 1994; 21:86–89.
8. Khattar RS, Senior R, Swales JD, Lahiri A. Value of ambulatory intraarterial blood pressure monitoring in the long-term prediction of left ventricular hypertrophy and carotid atherosclerosis in essential hypertension. J Hum Hypertens. 1999; 13:111–116.
9. Sega R, Facchetti R, Bombelli M, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005; 111:1777–1783.
10. Lee SJ, Park SH. Arterial ageing. Korean Circ J. 2013; 43:73–79.
11. Boutouyrie P, Tropeano AI, Asmar R, et al. Aortic stiffness is an independent predictor of primary coronary events in hypertensive patients: a longitudinal study. Hypertension. 2002; 39:10–15.
12. Meaume S, Benetos A, Henry OF, Rudnichi A, Safar ME. Aortic pulse wave velocity predicts cardiovascular mortality in subjects >70 years of age. Arterioscler Thromb Vasc Biol. 2001; 21:2046–2050.
13. Sutton-Tyrrell K, Najjar SS, Boudreau RM, et al. Elevated aortic pulse wave velocity, a marker of arterial stiffness, predicts cardiovascular events in well-functioning older adults. Circulation. 2005; 111:3384–3390.
14. Blacher J, Guerin AP, Pannier B, Marchais SJ, Safar ME, London GM. Impact of aortic stiffness on survival in end-stage renal disease. Circulation. 1999; 99:2434–2439.
15. Pannier B, Guérin AP, Marchais SJ, Safar ME, London GM. Stiffness of capacitive and conduit arteries: prognostic significance for end-stage renal disease patients. Hypertension. 2005; 45:592–596.
16. Willum-Hansen T, Staessen JA, Torp-Pedersen C, et al. Prognostic value of aortic pulse wave velocity as index of arterial stiffness in the general population. Circulation. 2006; 113:664–670.
17. Mattace-Raso FU, van der Cammen TJ, Hofman A, et al. Arterial stiffness and risk of coronary heart disease and stroke: the Rotterdam Study. Circulation. 2006; 113:657–663.
18. Pauca AL, O'Rourke MF, Kon ND. Prospective evaluation of a method for estimating ascending aortic pressure from the radial artery pressure waveform. Hypertension. 2001; 38:932–937.
19. Williams B, Lacy PS, Thom SM, et al. Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study. Circulation. 2006; 113:1213–1225.
20. Tsai PS. Determinants of the white-coat effect in normotensives and never-treated mild hypertensives. Clin Exp Hypertens. 2003; 25:443–454.
21. Dolan E, Stanton A, Atkins N, et al. Determinants of white-coat hypertension. Blood Press Monit. 2004; 9:307–309.
22. Staessen JA, O'Brien ET, Atkins N, Amery AK. Short report: ambulatory blood pressure in normotensive compared with hypertensive subjects. The Ad-Hoc Working Group. J Hypertens. 1993; 11:1289–1297.
23. Pickering TG, James GD, Boddie C, Harshfield GA, Blank S, Laragh JH. How common is white coat hypertension? JAMA. 1988; 259:225–228.
24. Pickering T. Ambulatory blood pressure monitoring: an historical perspective. Clin Cardiol. 1992; 15:5 Suppl 2. II3–II5.
25. Park SH, Bang DW, Seo J, et al. Comparison of the ambulatory blood pressure with the clinical blood pressure and electrocardiographic left ventricular hypertrophy. Korean J Med. 2007; 72:181–190.
26. Roman MJ, Devereux RB, Kizer JR, et al. Central pressure more strongly relates to vascular disease and outcome than does brachial pressure: the Strong Heart Study. Hypertension. 2007; 50:197–203.
27. Agabiti-Rosei E, Mancia G, O'Rourke MF, et al. Central blood pressure measurements and antihypertensive therapy: a consensus document. Hypertension. 2007; 50:154–160.
28. McEniery CM, Yasmin , Hall IR, et al. Normal vascular aging: differential effects on wave reflection and aortic pulse wave velocity: the Anglo-Cardiff Collaborative Trial (ACCT). J Am Coll Cardiol. 2005; 46:1753–1760.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download