Abstract
Background and Objectives
Non-high density lipoprotein-cholesterol (non-HDL-C) and apolipoprotein B (ApoB) are markers of atherosclerotic risk and predictors of cardiovascular events. The aim of this study was to evaluate clinical impact of non-HDL-C and ApoB on clinical outcomes in metabolic syndrome (MS) patients with acute myocardial infarction (AMI) undergoing percuatneous coronary intervetion.
Subjects and Methods
We analyzed 470 MS patients (64.4±12.0 years, 53.6% male) with AMI who were followed-up for 12-month after percutaneous coronary intervention (PCI) from December 2005 to January 2008 in a single center. These patients were divided into 2 groups based on median values of non-HDL-C and ApoB. We studied their baseline and follow-up relation with 12-month clinical outcomes, all-cause death and major adverse cardiac events (MACE).
Results
Mean values of baseline non-HDL-C and ApoB were 141.2±43.1 mg/dL and 99.3±29.0 mg/dL respectively. During 12-month follow-up 32 MACE (6.8%) and 12 deaths (2.5%) occurred. We observed significant correlation between non-HDL-C and ApoB. Twelve-month MACE and all-cause death after PCI showed no significant relation as non-HDL-C or ApoB levels increased. Follow-up patients (n=306, rate 65%) also did not show significant relation with clinical outcomes. Twelve-month MACE decreased as non-HDL-C and ApoB reduction rates increased.
Metabolic syndrome (MS) is characterized by the clustering of risk factors related to insulin resistance and is associated with an increased rate of cardiovascular disease and all-cause mortality.1-4) Several studies have established the significance of non-high density lipoprotein-cholesterol (non-HDL-C) and apolipoprotein B (ApoB) as predictive factors for coronary artery disease (CAD) and their association with excess cardiovascular morbidity and mortality.2)3) Non-HDL-C measurement (calculated as total cholesterol minus HDL-C) provides a single index of all the atherogenic ApoB containing lipoproteins - low density lipoprotein, very low density lipoprotein, intermediate-density lipoprotein and other remnant lipoproteins. In 2001, the National Cholesterol Education Program (NCEP) Adult Treatment Panel (ATP) III provided a new definition for MS and this is based on simple clinical criteria and is considered as a prognostic indicator of vascular risk in patients with no overt CAD.1-5) Most recently, in 2005, American Heart Association/National Heart Lung and Blood Institute (AHA/NHLBI) presented new criteria modified from NCEP-ATP III criteria.6)
Prevention of cardiovascular events in MS patients is the main theme of cardiology today. Therefore, the aim of this study was to investigate the association of non-HDL-C and ApoB with clinical outcomes in MS patients with acute myocardial infarction (AMI) after percuatneous coronary intervetion (PCI).
This retrospective study was carried out at The Heart Center of National University Hospital, Korea. The study was conducted according to the declaration of Helsinki. Informed written consent for the procedures was obtained from all patients and permission to carry out the study had been sought from the hospital authorities (institutional review board number 05-49 and I-2008-01-009).
The Korea Acute Myocardial Infarction Registry is a prospective, multicenter, observational registry designed to examine current epidemiology in hospital management and outcome of patients with AMI in Korea for the commemoration of the 50th anniversary of the Korean Circulation Society. The registry included 52 community and university hospitals for primary PCI. Data was collected at each site by a well-trained study coordinator based on standardized protocol.7)8)
Patients with AMI from December 2005 to January 2008 were assessed by the diagnostic criteria of MS and followed up for 12 months. ST-segment elevation myocardial infarction (STEMI) and non-STEMI patients who did not fulfill the criteria of MS were excluded from this study. As a result, a total number of 470 patients were selected for this study, mean age was 64.4±12.0 years and 53.6% patients were male (n=252).
Patients' medical documents were used to note the demographic data, clinical characteristics and relevant laboratory results. Diabetes mellitus (DM) was defined as use of oral hypoglycaemic agent or insulin to lower blood glucose levels. Hyperlipidemia was defined as total cholesterol >200 mg/dL or treatment with a lipid-lowering agent. CAD was defined as history of myocardial infarction (MI), revascularization procedure or obstructive CAD. A final diagnosis of AMI was made according to European Society of Cardiology/American College of Cardiology diagnostic criteria of AMI.9)
Peripheral blood samples were obtained on admission using direct venipuncture. Blood samples were centrifused and serum was removed and stored at -70℃ until the assay for sugar and proteins could be performed. Blood samples for high sensitivity-C-reactive protein (hs-CRP) were obtained on admission and were analyzed turbidimetrically with sheep antibodies against human CRP; this has been validated against the Dade Behring method. Absolute creatine kinase-MB levels were determined by radioimmunoassay (Dade Behring, Inc., Miami, FL, USA). Cardiac specific troponin I levels were measured by a paramagnetic particle, chemiluminescent immunoenzymatic assay (Beckham, Coulter, Inc. Fullerton, CA, USA). Twelve-hour fasting serum levels of total cholesterol, triglyceride, low and high density lipoprotein-cholesterol, and ApoB were measured by standard enzymatic methods. Non-HDL-C was calculated as total cholesterol minus high density lipoprotein-cholesterol (HDL-C). The selected patients were divided into two groups according to the median value of baseline non-HDL-C, group 1 ≤138 mg/dL, n=234 and group 2 >138 mg/dL, n=236. In another set, these patients were divided into two groups based on median value of baseline ApoB, group 1 ≤96.5 mg/dL, n=235 and group 2 >96.5 mg/dL, n=235.
Two-dimensional echocardiography was performed in all patients and left ventricular ejection fraction was assessed by Simpsons biplanar method. The morphology in coronary angiography was classified by criteria of American College of Cardiology/American Heart Association (ACC/AHA).10) The degree of coronary flow was classified by Thrombolysis in Myocardial Infarction score.11) Presence of left main coronary artery stenosis was defined as a luminal stenosis ≥50%. Multivessel disease was defined as the presence of a lesion with >50% stenosis in a non-infarct related coronary artery. All patients were administered loading doses of aspirin 325 mg and clopidogrel 300-600 mg before PCI. On admission anticoagulation was performed with un-fractionated heparin 5000 IU IV bolus followed by 24000 IU over 24 hours. During PCI 5000-7500 IU IV bolus is given followed by 1000 IU an hour later, then additional heparin to achieve an activated clotting time of 250-350 seconds. After the procedure, aspirin 100-200 mg (once daily) was prescribed indefinitely. Clopidogrel was prescribed continuously for 1 year.
The clinical outcomes studied were 1) 12-month major adverse cardiac events (MACE) and 2) 12-month all-cause death. MACE included all-cause death, non-fatal MI and target vessel revascularization. All data were recorded on a standardized, electronic, web based registry at http://www.kamir.or.kr.
For the diagnosis of MS at baseline we followed the NCEP-ATP III criteria. Central obesity was defined as waist circumference >90 cm in men or >80 cm in women by modified ATP III guideline that WHO-Western Pacific Region and International Association for the Study of Obesity presented for Asian populations in 2000. The presence of MS was analyzed considering the presence of the following criteria: 1) central obesity: waist circumference >90 cm (men), >80 cm (women), 2) a fasting triglyceride level ≥150 mg/dL, 3) reduced HDL-C: <40 mg/dL (men), <50 mg/dL (women), 4) hypertension: blood pressure ≥130/85 mm Hg or taking antihypertensive medication, 5) impaired fasting glucose (IFG): fasting glucose ≥110 mg/dL, or taking anti-diabetic medication or past history of type 2 DM. Patients were considered to have MS in the presence of ≥3 of the above criteria according to the definition proposed by AHA/NHLBI. Although AHA/NHLBI guideline recommended the definition of IFG at/above 100 mg/dL, our study adopted NCEP-ATP III guideline.6)
This set of MS patients were followed up for 10-15 months (n=306, follow-up rate 65.1%) with a mean follow-up at 12 months. They were also divided into two groups based on their non-HDL-C and ApoB follow-up levels and clinical outcomes were also studied. To evaluate the effect of after treatment reduction of non-HDL-C and ApoB on clinical outcomes we divided the same subset of patients into three groups based on their reduction percentage-group A (reference group) included reduction rate 0-10% (n=16 in non-HDL-C arm and n=23 in ApoB arm), group B included 10-30% reduction (n=30 in non-HDL-C arm and n=64 in ApoB arm) and group C included >30% (n=158 in non-HDL-C arm and n=117 in ApoB arm). We also studied patients who had higher follow-up levels of non-HDL-C and ApoB than the baseline levels (n=102) so that we could compare the impact of their reduction and increase on clinical outcomes.
Statistical Package for the Social Sciences (SPSS) 17.0 for windows (SPSS Inc., Chicago, IL, USA) was used for all analysis. Continuous variables were presented as mean±SD. Comparisons were conducted by Student's t-test. Discrete variables were presented as percentages and frequencies; comparisons were conducted by chi-square/Fischer's exact statistics. All statistical tests were 2-tailed, with statistical significance defined as p<0.05. To estimate the degree of relationship between the two quantitative non-parametric variables we used Pearson's correlation test or Spearman's rank correlation test. We used linear-by-linear association to evaluate the relation between a parameter and 12-month clinical outcomes.
Cox proportional hazard analysis was performed to identify a model with independent predictive factors with a determination of hazard ratio and its 95% confidence interval for each variable in the model. A cut off p<0.2 in univariate analysis for end points and other variables that have been reported to be associated with prognosis of patients with AMI were entered into the Cox model. The variables included were age, gender, systolic blood pressure, hypertension, history of CAD, serum creatinine, total cholesterol, triglyceride, ApoB, clinical presentation with STEMI, hs-CRP, N-terminal pro-brain natrieuretic peptide, HDL-C, left main involvement, ACC/AHA lesion type C, in-hospital complications, and use of beta-blocker, calcium-channel blocker and statin for baseline non-HDL-C. The variables included in baseline ApoB Cox model were age, gender, systolic blood pressure, hypertension, clinical presentation with STEMI, serum creatinine, total cholesterol, triglyceride, hs-CRP, HDL-C, non-HDL-C, left main involvement, in-hospital complications, and statin use. The number of 12-month deaths was very small, n=12 (2.5%) so we limited our analysis to MACE.
A total number of 470 MS patients were selected for this study with mean age 64.4±12.0 years and 53.6% were men (n=252). The mean values of baseline non-HDL-C and ApoB were 141.2±43.1 mg/dL and 99.3±29.0 mg/dL respectively. These patients were followed up for 12-month (n=306, follow-up rate 65%).
As shown in Table 1, patients in group 2 i.e. with higher non-HDL-C (>138 mg/dL) tended to be younger. They showed increased systolic blood pressure, total cholesterol, triglyceride and ApoB whereas previous history of hypertension, serum creatinine, hs-CRP, left main involvement, and in-hospital complications decreased. Frequency of STEMI and use of calcium-channel blocker was lower and use of statin was higher in group 2. As shown in Table 2, patients in group 2, with higher ApoB (>96.5 mg/dL) levels were younger, and showed increased systolic blood pressure, total cholesterol, triglyceride and non-HDL-C whereas serum creatinine, hs-CRP, left main involvement and in-hospital complications decreased. The use of statin was more frequently observed in group 2.
During 12-month follow-up 32 MACE (6.8%) and 12 deaths (2.5%) occurred. Pearson's simple correlation analysis revealed a significant correlation between baseline non-HDL-C and ApoB (r=0.655, p<0.001) and Spearman's rank test also showed a significant correlation between them (r=0.655, p<0.001).
Twelve-month MACE and death after PCI showed no significance association between non-HDL-C baseline groups: 12-month MACE, 7.26% in group 1 vs. 6.35% in group 2 with unadjusted p=0.595, linear p=0.714 and adjusted p=0.516; and 12-month death, 2.56% in group 1 vs. 2.54% in group 2 with unadjusted p=0.486, linear p=0.99 and adjusted p=0.716 as shown in Table 3. Also, 12-month MACE and death after PCI showed no significance association between ApoB baseline groups: 12-month MACE, 6.8% in both groups with unadjusted p=0.698, linear p=0.958 and adjusted p=0.675; 12-month death, 2.5% in each group with unadjusted p=0.712, linear p=0.975 and adjusted p=0.919 as shown in Table 4.
Cox regression analysis of baseline non-HDL-C and ApoB groups showed no significant association with 12-month MACE (p=0.516 and p=0.675 respectively). Left main involvement was the only independent factor for 12-month MACE in baseline ApoB arm {3.77 (1.015-14.014), p=0.047}. In-hospital complications included any of atrio-ventricular block, bradycardia, ventricular tachycardia, ventricular fibrillation, atrial fibrillation, cardiogenic shock, acute renal failure, metabolic acidosis/lactic acidosis, cerebrovascular event and/or infection/sepsis.
A total of 306 out of 470 MS patients were followed up for 12 months (follow-up rate 65.1%). They were also divided into 2 groups based on median values of non-HDL-C (104.7 mg/dL) and ApoB (76.05 mg/dL). Cox model showed no significant relation between 12-month MACE and follow-up non-HDL-C (p=0.205) or ApoB (p=0.831). N-terminal pro-brain natrieuretic peptide was the only independent predictor of 12-month MACE in non-HDL-C follow-up arm {2.628 (1.025-6.738), p=0.044}.
Fig. 1A and B show Cox adjusted survival curves for 12-month MACE of baseline and follow-up non-HDL-C respectively. Fig. 1C and D show Cox adjusted survival curves for 12-month MACE of baseline and follow-up ApoB respectively.
Reduction rate of non-HDL-C showed a decreasing trend of 12-month MACE, but it was not statistically significant {43.8% reduction in group A (0-10%) vs. 26.7% in group B (10-30%) vs. 19.0% in group C (>30%), p=0.069} as shown in Fig. 2. We noted that 12-month MACE also showed a decreasing trend as ApoB reduction rate increased {47.8% reduction in group A (0-10%) vs. 23.4% in group B (10-30%) vs. 16.2% in group C (>30%), p=0.004} as shown in Fig. 3. Prognostic value of the rates of ApoB reduction for 12-month MACE is presented in Table 5, when unadjusted showed significant relation with 12-month MACE (unadjusted p=0.012), 59% reduction in group B {0.417 (0.191-0.907), p=0.027} and 67% reduction in group C {0.331 (0.157-0.695), p=0.003}. It was also significant when adjusted with age and gender (Model 1), p=0.012, 57% reduction in group B {0.437 (0.199-0.958), p=0.039} and 68% reduction in group C {0.324 (0.153-0.683), p=0.003}. After adjustment with multiple covariates (Model 2), patients in group B had 57% reduction {0.431 (0.186-0.997), p=0.049} and patients in group C had 62% reduction {0.383 (0.171-0.855), p=0.019} for MACE at 12-month follow-up. The variables included in Model 2 were age, gender, creatinine, total cholesterol, triglyceride, Killip class, history of hyperlipidemia, clinical presentation with ST-elevation MI and ACC/AHA lesion type C.
We further analyzed the patients with increase in ApoB level during follow-up and found no significant association with 12-month MACE (unadjusted p=0.734 and adjusted p=0.43). Patients with increase in non-HDL-C were also found to have no significant association with 12-month MACE during follow-up (unadjusted p=0.283 and adjusted p=0.744). Statin use was insignificant in both the arms (p=0.558 in non-HDL-C arm and p=0.789 in ApoB arm) during follow-up.
The present study demonstrated that higher non-HDL-C and ApoB levels in MS patients with AMI who underwent PCI showed no significant association with 12-month MACE. There was positive correlation between non-HDL-C and ApoB. ApoB was found to be a better predictor of 12-month MACE than non-HDL-C based on their reduction rates.
The prevalence of MS has reached epidemic proportions.12) These patients are at three-fold greater risk of CAD and five-fold greater risk of cardiovascular mortality.13) Dyslipidemia is a hallmark of MS and is characterized by elevation of triglyceride and low HDL-C. Plasma low density lipoprotein-cholesterol (LDL-C) is often found to be normal in these patients.14) Non-HDL-C provides a measure of all ApoB-containing lipoproteins, all of which have the potential to deliver cholesterol into the arterial wall and contribute to atherosclerotic lesions. This measure thus reflects atherogenic risk not captured by LDL-C measurement alone, particularly in the context of elevated triglyceride. Total serum ApoB is a strong predictor for severity of coronary atherosclerosis and CAD events, and non-HDL-C is highly correlated with ApoB levels.3) In Table 1 and 2, patients in group 1 were found to have lower levels of triglyceride. This might be by the definition of MS itself or due to older age, chronic kidney disease or may be influenced by heparin injection. We used fasting lipid levels after PCI for this analysis. The potential effect of heparin use on lipid levels might have influenced this study's results. The fact that the incidence of in-hospital complications was higher in groups with lower non-HDL-C or ApoB. This could be attributed to older age, higher incidence of STEMI, let main artery disease, hypertension and also higher levels of serum creatinine and hs-CRP.
Earlier studies demonstrated a 'paradoxical' decrease in mortality with a history of hypercholesterolemia.3)15)16) The explanation for why hypercholesterolemia, unlike other cardiac risk factors, is paradoxically associated with better clinical outcomes remains obscure. Rauchhaus et al.15) suggested that survival, in general, is a result of balance of risks. Circulating lipoproteins play a potentially beneficial role by neutralizing lipopolysaccharides, which is a possible source of the immunologic activation in chronic heart failure. Cho et al.17) studied the cholesterol paradox in AMI patients that showed higher LDL-C levels, except for patients with LDL-C ≥160 mg/dL, were related to better clinical outcome after PCI. Another reason suggested for this paradox in patients with AMI is the impact of statin treatment and the fact that previously diagnosed hypercholesterolemia is a marker for patients with more prior medical contact.15) It is also known that obesity is a serious independent risk factor for CAD. But multiple studies have shown that obese CAD patients have better survival rate and have fewer cardiovascular events than normal-weight or underweight patients after PCI.18-20) The reason of this obesity paradox is unclear. According to previous hypothesis normal and low body mass index (BMI) patients have small vessel size compared to obese. Consequently, they have smaller intravascular volume and poor compensation for a given amount of bleed.
Previous AMI studies have shown a higher incidence of morbidity and mortality in older patients regardless of treatment options.21)22) In our study, patients with higher non-HDL-C and ApoB levels were found to be younger. Younger age is most likely implicated in the confounded relation between higher BMI and AMI outcomes. This implies that AMI occurs at a younger age in the obese. It is this younger age that counterbalances the risks that DM, hypertension or dyslipidemia pose in the immediate course of care. As part of being younger, obese patients may have received more aggressive or attentive care.19) Follow-up analysis also suggested that non-HDL-C and ApoB had no relationship to clinical outcomes. However, this might be due to lower follow-up rates that may lead to false negative results.
Non-high density lipoprotein-cholesterol has been proposed to be an acceptable surrogate of ApoB in routine clinical practice on the basis of the fact that they are highly correlated.2)3) However, they do not measure the same thing: non-HDL-C is the mass of cholesterol in the ApoB-containing lipoproteins, whereas ApoB is the number of atherogenic particles. The atherogenic risk resulting from lipoproteins does not relate primarily to their cholesterol content but rather to their size and number. In this regard, it is clearly important to examine whether ApoB is superior to non-HDL-C in its prediction of the risk of cardiovascular disease.
The study by Pischon et al.23) demonstrated that ApoB is superior to non-HDL-C to identify the risk of cardiovascular events. If ApoB and non-HDL-C are metabolically equivalent, they should keep the same biological company. But it is not so, ApoB is more closely associated with increased BMI, abdominal obesity, hyperglycemia, insulin resistance, and pro-thrombogenic and pro-inflammatory markers than non-HDL-C.24)25) In other words, ApoB relates more closely to the other features of the MS than non-HDL-C. On these grounds, ApoB, and not non-HDL-C, should be the pro-atherogenic index of choice in these patients.26) Also, an earlier study in Korean population demonstrated that ApoB is a better marker than non-HDL-C for identifying MS.27)
Incidence of each of cardiovascular death, MI, and repeated revascularization were considered as components of MACE and not studied individually as it has long since been established that lipid profile and re-stenosis have no relationship. Cholesterol and obesity paradox may have some influence on the findings of our study and could explain the relation between higher non-HDL-C/ApoB and clinical outcomes. We suggest further randomized study with longer term follow-up of this finding to elucidate its role in MS patients with AMI after PCI.
The present study should be interpreted in the light of the following limitations. First, this is not a randomized trial, but a retrospective study. Second, patient population is relatively small but Cho et al.17) studied cholesterol paradox in a large population with 9571 AMI patients from the same registry and demonstrated similar results. Third, in the majority of cases blood samples for lipid profile were taken at least several hours ("overnight fasting blood") after the onset of infarction. Therefore the non-HDL-C levels may be influenced by infarction. Fourth, diurnal variations of ApoB and non-HDL-C were not taken into consideration in our study. Fifth, heparin which is an integral part of treatment strategy in AMI setup may influence serum levels of non-HDL-C and ApoB. Sixth, the diagnosis of MS should be made using data obtained at least 8 weeks after AMI or surgery, because in the early course of AMI, levels of cholesterols, glucose, and inflammatory markers are all altered, but we did not have exact 8 weeks data of all patients.
In conclusion, 1) There was positive correlation between non-HDL-C and ApoB. 2) There was no significant association between higher levels of either non-HDL-C or ApoB and 12-month MACE in MS patients with AMI undergoing PCI. 3) ApoB is a better predictor of MACE than non-HDL-C based on their reduction rates in this patient population.
We suggest fully randomized long-term follow-up evaluation of our findings to reach a concrete conclusion.
Figures and Tables
Fig. 1
Adjusted 12-month survival curves for MACEs. A: baseline non-HDL-C. B: follow-up non-HDL-C. C: baseline ApoB. D: follow-up ApoB. MACE: major adverse cardiac event, non-HCL-C: non-high density lipoprotein-cholesterol, AopB: apolipoprotein B.

Fig. 2
Non-HDL-C reduction rates vs. 12-month major adverse cardiac events. non-HCL-C: non-high density lipoprotein-cholesterol.
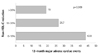
Table 1
Baseline clinical characteristics, coronary angiographic findings and procedural results according to the levels of non-high density lipoprotein-cholesterol

Table 2
Baseline characteristics, coronary angiographic findings and procedural results according to the levels of apolipoprotein B

Table 3
Clinical outcomes at 12 months after percutaneous coronary intervention according to the baseline levels of non-high density lipoprotein-cholesterol

Table 4
Clinical outcomes at 12 months after percutaneous coronary intervention according to the baseline levels of apolipoprotein B

Table 5
Prognostic value of the rates of ApoB reduction for 12-month MACE

*Reference group, †Adjusted for age and gender, ‡Adjusted for age, gender, creatinine, total cholesterol, triglyceride, Killip class, history of hyperlipidemia, clinical presentation with ST-elevation MI and ACC/AHA lesion type C. ACC/AHA: American College of Cardiology/American Heart Association, ApoB: apolipoprotein B, MI: myocardial infarction, MACE: major adverse cardiac events
Acknowledgments
This study was performed with the support of Korea Ministry of Health & Welfare (A084869). The authors thank Dr. Sumera K. Ahmed for her contribution to this study.
References
1. Ferrannini E, Haffner SM, Mitchell BD, Stern MP. Hyperinsulinaemia: the key feature of a cardiovascular and metabolic syndrome. Diabetologia. 1991. 34:416–422.
2. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002. 106:3143–3421.
3. Ballantyne CM, Andrews TC, Hsia JA, Kramer JH, Shear C. ACCESS Study Group. Correlation of non-high-density lipoprotein cholesterol with apolipoprotein B: effect of 5 hydroxymethylglutaryl coenzyme A reductase inhibitors on non-high-density lipoprotein cholesterol levels. Am J Cardiol. 2001. 88:265–269.
4. Lakka HM, Laaksonen DE, Lakka TA, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002. 288:2709–2716.
5. Sattar N, Gaw A, Scherbakova O, et al. Metabolic syndrome with and without C-reactive protein as a predictor of coronary heart disease and diabetes in the West of Scotland Coronary Prevention Study. Circulation. 2003. 108:414–419.
6. Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005. 112:2735–2752.
7. Lee KH, Jeong MH, Ahn YK, et al. Sex differences of the clinical characteristics and early management in the Korea acute myocardial infarction registry. Korean Circ J. 2007. 37:64–71.
8. Sim DS, Kim JH, Jeong MH. Differences in clinical outcomes between patients with ST-elevation versus non-ST-elevation acute myocardial infarction in Korea. Korean Circ J. 2009. 39:297–303.
9. Apple FS, Wu AH, Jaffe AS. European Society of Cardiology and American College of Cardiology guidelines for redefinition of myocardial infarction: how to use existing assays clinically and for clinical trials. Am Heart J. 2002. 144:981–986.
10. Kini AS. Coronary angiography, lesion classification and severity assessment. Cardiol Clin. 2006. 24:153–162.
11. Manginas A, Gatzov P, Chasikidis C, Voudris V, Pavlides G, Cokkinos DV. Estimation of coronary flow reserve using the Thrombolysis In Myocardial Infarction (TIMI) frame count method. Am J Cardiol. 1999. 83:1562–1565.
12. Kereiakes DJ, Willerson JT. Metabolic syndrome epidemic. Circulation. 2003. 108:1552–1553.
13. Isomaa B, Almgren P, Tuomi T, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001. 24:683–689.
14. Reilly MP, Rader DJ. The metabolic syndrome: more than the sum of its parts? Circulation. 2003. 108:1546–1551.
15. Rauchhaus M, Clark AL, Doehner W, et al. The relationship between cholesterol and survival in patients with chronic heart failure. J Am Coll Cardiol. 2003. 42:1933–1940.
16. Wang TY, Newby LK, Chen AY, et al. Hypercholesterolemia paradox in relation to mortality in acute coronary syndrome. Clin Cardiol. 2009. 32:E22–E28.
17. Cho KH, Jeong MH, Ahn Y, et al. Low-density lipoprotein cholesterol level in patients with acute myocardial infarction having percutaneous coronary intervention (the cholesterol paradox). Am J Cardiol. 2010. 106:1061–1068.
18. Gruberg L, Weissman NJ, Waksman R, et al. The impact of obesity on the short-term and long-term outcomes after percutaneous coronary intervention: the obesity paradox? J Am Coll Cardiol. 2002. 39:578–584.
19. Gurm HS, Brennan DM, Booth J, Tcheng JE, Lincoff AM, Topol EJ. Impact of body mass index on outcome after percutaneous coronary intervention (the obesity paradox). Am J Cardiol. 2002. 90:42–45.
20. Mehta L, Devlin W, McCullough PA, et al. Impact of body mass index on outcomes after percutaneous coronary intervention in patients with acute myocardial infarction. Am J Cardiol. 2007. 99:906–910.
21. Prasad A, Stone GW, Aymong E, et al. Impact of ST-segment resolution after primary angioplasty on outcomes after myocardial infarction in elderly patients: an analysis from the CADILLAC trial. Am Heart J. 2004. 147:669–675.
22. Tespili M, Guagliumi G, Valsecchi O, et al. In-hospital clinical outcome in elderly patients with acute myocardial infarction treated with primary angioplasty. Ital Heart J. 2003. 4:193–198.
23. Pischon T, Girman CJ, Sacks FM, Rifai N, Stampfer MJ, Rimm EB. Non-high-density lipoprotein cholesterol and apolipoprotein B in the prediction of coronary heart disease in men. Circulation. 2005. 112:3375–3383.
24. Sniderman AD, St-Pierre AC, Cantin B, Dagenais GR, Després JP, Lamarche B. Concordance/discordance between plasma apolipoprotein B levels and the cholesterol indexes of atherosclerotic risk. Am J Cardiol. 2003. 91:1173–1177.
25. Sattar N, Williams K, Sniderman AD, D'Agostino R Jr, Haffner SM. Comparison of the associations of apolipoprotein B and non-high-density lipoprotein cholesterol with other cardiovascular risk factors in patients with the metabolic syndrome in the Insulin Resistance Atherosclerosis Study. Circulation. 2004. 110:2687–2693.
26. Sniderman AD. Apolipoprotein B versus non-high-density lipoprotein cholesterol: and the winner is. Circulation. 2005. 112:3366–3367.
27. Han JH, Park HS, Kim JA, Kim SM. Apolipoprotein B is a better marker than non-HDL-cholesterol for the metabolic syndrome in Koreans. Atherosclerosis. 2008. 197:333–338.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download