Abstract
Background and Objectives
It is not well understood whether the left ventricular geometry is associated with such diastolic parameters as the left atrial volume and the left ventricular filling pressure, as assessed by the Doppler indices. Accordingly, this study aimed to evaluate the influence of the left ventricular geometry on the left atrial volume and the left ventricular filling pressure, as assessed by the Doppler indices.
Subjects and Methods
181 patients (mean age: 63±9 years old, 62 males) with hypertension were included for echocardiographic analysis. The hypertensive patients were classified into four groups according to the left ventricular mass index and the relative wall thickness: normal geometry, concentric remodeling, eccentric hypertrophy and concentric hypertrophy. We excluded all the individuals with established cardiovascular disease, atrial fibrillation, significant aortic and/or mitral valve disease, or an ejection fraction <50%.
Results
By definition, the left ventricular mass was increased in the patients with eccentric and concentric hypertrophy. Both the left ventricular end-systolic diameter and the left ventricular end-diastolic diameter were reduced in the concentric remodeling group, whereas the left ventricular end-systolic diameter and the left ventricular end-diastolic diameter were increased in the eccentric and concentric hypertrophy groups. Compared with the patients with normal geometry, the patients with eccentric and concentric hypertrophy demonstrated a significant higher value for the left atrial volume index. The ratio of the transmitral inflow velocity to the mitral annular velocity (E/E') showed a stepwise increase from the patients with normal geometry to the patients with concentric remodeling, and then to the patients with eccentric and concentric hypertrophy.
Conclusion
This study demonstrates that in a patient population with hypertension and who are without systolic dysfunction, the left atrial volume index and the E/E' demonstrated a progressive worsening of the left ventricular diastolic function from patients with normal geometry to the patients with concentric remodeling, and then to the patients with eccentric and concentric hypertrophy.
The cardiac adaptation of the left ventricle to hypertension may occur in four different geometric patterns, as based on the left ventricular mass index (LVMI) and the relative wall thickness (RWT). The left ventricular geometric patterns include the normal geometry with the normal LVMI and RWT, concentric remodeling with the normal LVMI and the increased RWT, eccentric hypertrophy with the increased LVMI and the normal RWT, and concentric hypertrophy with increases in both the LVMI and RWT.1)2) Studies that have grouped hypertensive patients by these geometric patterns have revealed distinctive profiles of the blood pressure,3) the hemodynamics4) and the prognosis.5) Simone et al.6) have also reported that the Doppler indices of abnormal relaxation were more impaired in the presence of concentric left ventricular geometry and this was assessed by using the diastolic filling pattern of the mitral flow. However, it is not well understood whether the left ventricular geometry is associated with the modern diastolic parameters, such as the left atrial volume and the left ventricular filling pressure, as assessed by the Doppler indices. Accordingly, this study aimed to evaluate the influence of the left ventricular geometry on the left atrial volume and the left ventricular filling pressure, as assessed by the Doppler indices.
Using our database of the patients who underwent transthoracic echocardiography between January 2004 and December 2007, we selected 181 patients, among all the hypertensive patients, for analysis and these 181 patients' clinical and echocardiographic data were readily available. Patients were defined as being hypertensive if they had a history of antihypertensive therapy, an office systolic blood pressure ≥140 mmHg or a diastolic blood pressure ≥90 mmHg. The prior medications consisted of calcium antagonists, diuretics, beta-blockers, angiotensin converting enzyme inhibitors and angiotensin receptor blocker. We excluded all the individuals with established cardiovascular diseases such as myocardial infarction, angina, coronary bypass grafting and congestive heart failure, atrial fibrillation, significant aortic and/or mitral valve disease, or an ejection fraction <50%. Based on the LVMI and the RWT, the patients were categorized into four groups: the normal geometry group, the concentric remodeling group, the eccentric hypertrophy group and the concentric hypertrophy group.
Transthoracic echocardiography was performed using a commercially available imaging ultrasound system (Sonos 5500, Hewlett-Packard Co., Palo Alto, CA, USA) with harmonic imaging. The measurements were made according to the recommendations of the American Society of Echocardiography and using the leading edge to leading edge convention.6) The left ventricular internal dimension, the septal thickness and the left ventricular posterior wall thickness were measured at end-diastole as defined by the onset of the QRS complex. The RWT was calculated as follows: 2×left ventricular posterior wall thickness/left ventricular end-diastolic dimension. A value more than 0.44 was defined as abnormal. The left ventricular mass was calculated using the formula developed by Devereux et al.8): 0.80×1.04 {(left ventricular end-diastolic diameter+left ventricular septal thickness+posterior wall thickness)3-(left ventricular end-diastolic diameter)3}+0.6. The LVMI was indexed for the body surface area. Left ventricular hypertrophy was to be considered present when the LVMI was >125 g/m2 in men or >110 g/m2 in women.9) The combination of the LVMI and RWT defined the four left ventricular geometric patterns: normal geometry (a normal LVMI and a normal RWT), concentric remodeling (a normal LVMI and an increased RWT), concentric hypertrophy (an increased LVMI and an increased RWT) and eccentric hypertrophy (an increased LVMI and a normal RWT).1) The left atrial diameter was measured by the two-dimensional guided M-mode echocardiography obtained with the parasternal short-axis view at the base of the heart.7) The left atrial volume was calculated from the apical four-chamber and two-chamber views at ventricular end systole with using Simpson's biplane method.10)
The mitral inflow velocities were obtained by pulsedwave Doppler during quiet respiration in the apical fourchamber view with a 1-2 mm sample volume placed at the tips of the mitral valve leaflets. The mitral early (E) and late (A) inflow velocities and the deceleration time (DT) of the E velocity were measured (Fig. 1A). The isovolumic relaxation time was measured by continuouswave Doppler as the time from the closing click of the aortic valve to the onset of transmitral inflow. The pulsedwave Doppler tissue imaging velocities were obtained from the apical four-chamber view during quiet respiration by placing a sample volume in the septal mitral annulus. Images of the left ventricle in the apical four-chamber view were chosen to minimize the angle of incidence between the scan lines and the motion of the lateral mitral annulus. The peak early (E') and late (A') diastolic mitral annular velocities were measured from the time-myocardial velocity waveform, and we calculated the septal E/E' ratio, which is a measure of the left ventricular filling pressure (Fig. 1B). The patients were classified into four different stages of diastolic function: 1) normal filling was defined as a DT greater than or equal to 140 milliseconds and less than 240 milliseconds, an E/A ratio between 1.0 and 2.0 and an E'/A' ratio above 1.0; 2) abnormal relaxation was defined as a DT above 240 milliseconds, an E/A ratio less than 1.0 and an E'/A' ratio less than 1.0; 3) pseudonormal filling was defined as a DT greater than or equal to 140 milliseconds and less than 240 milliseconds, an E/A ratio between 1.0 and 2.0 and an E'/A' ratio less than 1.0; and finally 4) restrictive filling was defined as a DT less than 140 milliseconds.
The data was analyzed using Statistical Package for Social Science (SPSS) 14.0 software (SPSS, Chicago, IL, USA). The variables are expressed as means±standard deviations. The continuous variables were compared by one-way analysis of variance followed by the Tukey post hoc test for multiple comparisons. Proportions were compared among groups by chi-square analysis. Statistical significance was defined as p<0.05.
The demographic characteristics of the study population are shown in Table 1. The four groups of patients that were characterized by the different left ventricular geometric patterns had a similar gender distribution and prevalence of diabetes, although the patients with left ventricular hypertrophy had a lower mean age than did the patients with normal geometry. The body mass index was lower in the eccentric hypertrophy group as compared with all the other groups. The patients with concentric hypertrophy had substantially elevated systolic blood pressure.
The two-dimensional echocardiographic variables are shown in Table 2. By definition, the left ventricular mass was increased in the groups with eccentric and concentric hypertrophy. As compared with the normal geometry group, the left ventricular end-systolic diameter and the left ventricular end-diastolic diameter were significantly reduced in the concentric remodeling group, whereas the left ventricular end-systolic diameter and the left ventricular end-diastolic diameter were increased in the eccentric and concentric hypertrophy groups. The patients with both eccentric and concentric hypertrophy demonstrated significantly higher values for the left atrial diameter and the left atrial volume index (Fig. 2).
The Doppler indices are shown in Table 3. There were no significant differences among any of the four groups in terms of the A velocity, the isovolumic relaxation time and the E' velocity. The E velocity was increased and the A' velocity was decreased in the groups with eccentric and concentric hypertrophy, as compared with those values of the normal geometry group. The DT was lower in the eccentric hypertrophy group, as compared with that of the other groups.
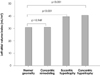
The E/E' showed a significant stepwise increase from the normal geometry group to the concentric remodeling group and then to the eccentric and concentric hypertrophy groups (Fig. 3). The differences of the diastolic filling pattern, as assessed by the mitral inflow, among the groups showed borderline significance (p=0.064).
The Doppler examination method has been used in recent years to evaluate the left ventricular diastolic function.11) Abnormalities in the left ventricular relaxation and/or increased filling pressures are indicators of left ventricular diastolic dysfunction. The E/E' ratio has been used as the initial measurement for estimating the left ventricular filling pressure, and particularly in those patients with a preserved systolic function. Patients with an E/E' >15 can be classified as having an elevated filling pressure and an E/E' <8 suggests a normal filling pressure.12) The left atrial volume can be viewed as a morphologic expression of the left ventricular diastolic dysfunction because exposure of the left atrium to an increased filling pressure results in its remodeling, which is reflected in the measurements of the left atrial volume.13) An increased E/E' ratio is associated with an increased left atrial volume, and this can readily be used to discriminate between normal individuals and the individuals with diastolic dysfunction.12)13) For the hypertensive patients who are without a discrete cause for their left atrial enlargement, an increased left atrial size may represent a very early sign of the impact of high pressure on the hypertensive heart.14)
Previous studies have reported a relationship between impaired left ventricular filling and left ventricular hypertrophy, which raised the possibility that the left ventricular geometric pattern could influence the characteristics of left ventricular filling.15-17) Furthermore, it has been reported that the indices of abnormal relaxation were more impaired in the presence of concentric left ventricular geometry and that there was an association between the concentric left ventricular geometry and abnormal relaxation.6)18)
This current study compared the left ventricular structure, the left atrial size, the mitral inflow indices and the Doppler tissue image velocities in hypertensive patients who had different geometries. All the participants had a normal left ventricular ejection fraction. The results demonstrated that patients with concentric remodeling, eccentric hypertrophy and concentric hypertrophy had an increased left ventricular filling pressure, as compared with the patients with normal geometry, and this most likely reflects the early left ventricular remodeling. Furthermore, the patients with eccentric and concentric hypertrophy had an increased left atrial volume index that reflected a more chronically impaired diastolic function, although these patient groups had a lower mean age and body mass index. The patients with eccentric and concentric hypertrophy also showed more advanced diastolic dysfunction according to the mitral inflow indices, so that there were more patients with a pseudonormal filling pattern and a shorter DT in this population, as compared with the patients who had normal geometry.
An interesting finding in the present study was that hypertensive patients with concentric remodeling had a significantly higher value for the E/E' than did the hypertensive patients with normal geometry, and this occurred despite the similarities between the groups for age, the gender distribution and the body size. This fact might explain a previous report that patients with left ventricular concentric remodeling had a worse prognosis than those with normal left ventricular geometry.19)20) However, the left atrial size, which is the parameter of the chronicity of the diastolic dysfunction, did not differ between the two groups (the patients with left ventricular concentric remodeling and the patients with normal left ventricular geometry), and this result means that patients with concentric remodeling revealed only very early changes that were indicative of diastolic dysfunction. As increased left ventricular filling pressures will inevitably lead to left atrial dilation, the patients with concentric remodeling might be on the way to left ventricular hypertrophy that's accompanied by an enlarged left atrium and a more elevated left ventricular filling pressure.
The results of this study suggest that diastolic dysfunction is an important indicator of abnormality for the progressive changes of the left ventricular geometry, and these changes from normal to concentric remodeling and then to eccentric and concentric hypertrophy are accompanied by further increases of the left ventricular filling pressure, which finally lead to the enlargement of the left atrial volume. Therefore, the left ventricular diastolic function progressively worsens from patients with normal geometry to the patients with concentric remodeling, and then to the patients with eccentric and concentric hypertrophy. Strict blood pressure control may be required for hypertensive patients who show an elevated left ventricular filling pressure and/or an enlarged left atrial volume to avoid further progression of the left ventricular geometric changes.
The major limitation of the current investigation is that it was a cross-sectional study and the data was obtained retrospectively by a review of the patients' records and echocardiograms rather than gathering the data prospectively, although the echocardiograms were reviewed without the reviewer having any knowledge of the clinical and hemodynamic data. The duration of hypertension and antihypertensive medication was not certain for some patients. Yet most of the patients were taking more than two types of drugs, so the effect of any specific drug on cardiac remodeling and the diastolic function could be minimized. The patients with concentric hypertrophy had elevated systolic blood pressure, as compared with the patients who had normal geometry, and this fact might have influenced the results. The differences in the left atrial volume index and the E/E' between the group of patients with concentric hypertrophy and the group of patients with eccentric hypertrophy were not statistically significant, so further studies with larger patient groups are needed to compare these two groups.
This study demonstrates that in a patient population with hypertension and without systolic dysfunction, both the left atrial volume index and the E/E' demonstrate progressive worsening of the left ventricular diastolic function in the order of the patients with normal geometry to the patients with concentric remodeling and to the patients with eccentric and concentric hypertrophy.
Figures and Tables
Fig. 1
Measurement of the mitral inflow velocities by pulsed-wave Doppler (A) and measurement of the mitral annular velocity by pulsed-wave Doppler tissue imaging (B). E: early diastolic mitral inflow velocity, A: late diastolic mitral inflow velocity, DT: deceleration time, E': early diastolic mitral annular tissue velocity, A': late diastolic mitral annular tissue velocity.

Fig. 3
The relationship of the left ventricular geometric pattern to the E/E'. E/E: the ratio of the transmitral inflow velocity to the mitral annular velocity.

Table 3
Doppler indices of the left ventricular diastolic function of the patient groups

The data is presented as the mean±SD. *p<0.001 versus normal geometry, †p<0.05 versus normal geometry. E: early diastolic mitral inflow velocity, A: late diastolic mitral inflow velocity, DT: deceleration time, IVRT: isovolumic relaxation time, E': early diastolic mitral annular tissue velocity, A': late diastolic mitral annular tissue velocity
References
1. Ganau A, Devereux RB, Roman MJ, et al. Patterns of left ventricular hypertrophy and geometric remodeling in essential hypertension. J Am Coll Cardiol. 1992. 19:1550–1558.
2. Balci B, Yilmaz O. Influence of left ventricular geometry on regional systolic and diastolic function in patients with essential hypertension. Scand Cardiovasc J. 2002. 36:292–296.
3. Devereux RB, James GD, Pickering TG. What is normal blood pressure?: comparison of ambulatory pressure level and variability in patients with normal or abnormal left ventricular geometry. Am J Hypertens. 1993. 6:211S–215S.
4. Im SA, Jung HK, Park SH, Shin GJ, Lee WH. Patterns of left ventricular hypertrophy and geometric remodeling in essential hypertension. Korean Circ J. 1995. 25:423–433.
5. Verdecchia P, Schillaci G, Borgioni C, et al. Adverse prognostic significance of concentric remodeling of the left ventricle in hypertensive subjects with normal left ventricular mass. J Am Coll Cardiol. 1995. 25:871–878.
6. de Simone G, Kitzman DW, Chinali M, et al. Left ventricular concentric geometry is associated with impaired relaxation in hypertension. Eur Heart J. 2005. 26:1039–1045.
7. Sahn DJ, Demaria A, Kisslo J, Weyman A. Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation. 1978. 58:1072–1083.
8. Devereux RB, Alonso DR, Lutas EM, et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986. 57:450–458.
9. Hammond LW, Devereux RB, Alderman MH, et al. The prevalence and correlates of echocardiographic left ventricular hypertrophy among employed patients with uncomplicated hypertension. J Am Coll Cardiol. 1986. 7:639–650.
10. Pritchett AM, Jacobsen SJ, Mahoney DW, Rodeheffer RJ, Bailey KR, Redfield MM. Left atrial volume as an index of left atrial size: a population-based study. J Am Coll Cardiol. 2003. 41:1036–1043.
11. Kim KS. The usefulness of Doppler tissue image in evaluation of left ventricular systolic and diastolic dysfunction. Korean Circ J. 2002. 32:99–105.
12. Ommen SR, Nishimura RA, Appleton CP, et al. Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: a comparative simultaneous Doppler-catheterization study. Circulation. 2000. 102:1788–1794.
13. Lester SJ, Tajik AJ, Nishimura RA, Oh JK, Khandheria BK, Seward JB. Unlocking the mysteries of diastolic function: deciphering the Rosetta Stone 10 years later. J Am Coll Cardiol. 2008. 51:679–689.
14. Miller JT, O'Rourke RA, Crawford MH. Left atrial enlargement: an early sign of hypertensive heart disease. Am Heart J. 1988. 116:1048–1051.
15. Fouad FM, Slominsk JM, Tarazi RC. Left ventricular diastolic function in hypertension: relation to left ventricular mass and systolic function. J Am Coll Cardiol. 1984. 3:1500–1506.
16. Douglas PS, Berko B, Lesh M, Reichk N. Alterations in diastolic function in response to progressive left ventricular hypertrophy. J Am Coll Cardiol. 1989. 13:461–467.
17. Galderisi M, Caso P, Severino S, et al. Myocardial diastolic impairment caused by left ventricular hypertrophy involves basal septum more than other walls: analysis by pulsed Doppler tissue imaging. J Hypertens. 1999. 17:685–693.
18. Marabotti C, Genovesi-Ebert A, Ghione S, Giaconi S, Palombo C. Diastolic function in the different patterns of left ventricular adaptation to essential hypertension. Int J Cardiol. 1994. 44:73–78.
19. Verdecchia P, Schillaci G, Borgioni C, et al. Adverse prognostic significance of concentric remodeling of the left ventricle in hypertensive patients with normal left ventricular mass. J Am Coll Cardiol. 1995. 25:871–878.
20. Pierdomenico SD, Lapenna D, Bucci A, Manente BM, Cuccurullo F, Mezzetti A. Prognostic value of left ventricular concentric remodeling in uncomplicated mild hypertension. Am J Hypertens. 2004. 17:1035–1039.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download