Abstract
Purpose
Little is known with respect to changes in the segmental thoracic and thoracolumbar kyphosis, which are major parameters influencing sagittal balance of the spine. The authors investigated the detailed segmental changes of those parameters by ageing.
Materials and Methods
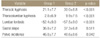
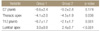
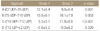
A total of 326 normal asymptomatic males were divided into 2 groups; group 1 (mean age, 21.2±1.7; n=175) and group 2 (mean age, 64.1±6.4; n=151). After taking a standing sagittal radiograph, the sagittal spinal and pelvic parameters were measured. Thoracic and thoracolumbar kyphosis were classified according to segments A, C7 UEP (upper end vertebra)–T5 UEP; B, T5 UEP–T10 UEP; C, T10 UEP–T12 LEP (lower end vertebra); and D, (T12 LEP–L2 LEP), and analyzed between 2 groups, respectively.
Results
Thoracic kyphosis (21.1°±7.7° vs. 30.0°±8.8°, p<0.001), segment B (15.8°±6.1° vs. 18.1°±7.9°, p=0.003), and segment C (5.3°±5.1° vs. 11.8°±6.5°, p<0.001) were increased in group 2. In group 2 segment A showed decreased kyphosis (12.1°±6.4° vs. 9.8°±6.4°, p=0.001). In segment D no significant difference was observed between groups.
Figures and Tables
Figure 1
The angular parameters showing thoracic kyphosis (TK, T5 UEP–T12 LEP), thoracolumbar kyphosis (TLK, T10 UEP–L2 LEP), and total lumbar lordosis (LL, T12 LEP–S1 UEP). Sacral slope (SS) and pelvic incidence (PI) are measured for the pelvic parameters. UEP, upper end plate; LEP, low end plate.

Figure 2
Four segments in thoracic kyphosis. Segment A, C7 UEP–T5 UEP; Segment B, T5 UEP–T10 UEP; Segment C, T10 UEP–T12 LEP; and Segment D, T12 LEP–L2 LEP. UEP, upper end plate; LEP, low end plate.

Figure 3
Chain of correlations. Group 1: young male group (range, 19–28 years), Group 2: old male group (range, 53–83 years).

References
1. Mehta VA, Amin A, Omeis I, Gokaslan ZL, Gottfried ON. Implications of spinopelvic alignment for the spine surgeon. Neurosurgery. 2015; 76:Suppl 1. S42–S56. discussion S56

2. Roussouly P, Nnadi C. Sagittal plane deformity: an overview of interpretation and management. Eur Spine J. 2010; 19:1824–1836.

3. Ahn YJ, Kim YB, Kang KB, Lee SW, Kim Y. Variations in sagittal spinopelvic parameters according to the lumbar spinal morphology in healthy Korean young men. J Korean Soc Spine Surg. 2010; 17:66–73.

4. Kang KB, Ahn YJ, Kim YJ, Kim YB, Park SC. Changes in sagittal spinopelvic parameters according to pelvic incidence in asymptomatic old Korean men. J Korean Soc Spine Surg. 2011; 18:223–229.

5. Kim YB, Kim YJ, Ahn YJ, et al. A comparative analysis of sagittal spinopelvic alignment between young and old men without localized disc degeneration. Eur Spine J. 2014; 23:1400–1406.

6. Kang KB, Kim YJ, Muzaffar N, Yang JH, Kim YB, Yeo ED. Changes of sagittal spinopelvic parameters in normal Koreans with age over 50. Asian Spine J. 2010; 4:96–101.

7. O'Brien MF, Kuklo TR, Blanke K, LG L. Spinal deformity study group radiographic measurement manual. Memphis (TN): Medtronic Sofamor Danek, Inc;2004.
8. Bartynski WS, Heller MT, Grahovac SZ, Rothfus WE, Kurs-Lasky M. Severe thoracic kyphosis in the older patient in the absence of vertebral fracture: association of extreme curve with age. AJNR Am J Neuroradiol. 2005; 26:2077–2085.
9. Manns RA, Haddaway MJ, McCall IW, Cassar Pullicino V, Davie MW. The relative contribution of disc and vertebral morphometry to the angle of kyphosis in asymptomatic subjects. Clin Radiol. 1996; 51:258–262.

10. Goh S, Price RI, Leedman PJ, Singer KP. The relative influence of vertebral body and intervertebral disc shape on thoracic kyphosis. Clin Biomech (Bristol, Avon). 1999; 14:439–448.

11. Boulay C, Tardieu C, Hecquet J, et al. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J. 2006; 15:415–422.

12. Legaye J, Duval-Beaupère G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998; 7:99–103.

13. Jean L. Influence of age and sagittal balance of the spine on the value of the pelvic incidence. Eur Spine J. 2014; 23:1394–1399.

14. Horton WC, Brown CW, Bridwell KH, Glassman SD, Suk SI, Cha CW. Is there an optimal patient stance for obtaining a lateral 36" radiograph? A critical comparison of three techniques. Spine (Phila Pa 1976). 2005; 30:427–433.
15. Toksoy A, Bektas F, Eken C, Ceken K, Cete Y. Value of the swimming position and arm traction in visualizing the cervicothoracic junction over the standard lateral cervical X-ray. Int J Emerg Med. 2010; 3:85–90.

16. Kim YJ, Lenke LG, Bridwell KH, et al. Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases. Spine (Phila Pa 1976). 2007; 32:2731–2738.
17. Kim YJ, Bridwell KH, Lenke LG, Glattes CR, Rhim S, Cheh G. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976). 2008; 33:2179–2184.
18. Watkins R 4th, Watkins R 3rd, Williams L, et al. Stability provided by the sternum and rib cage in the thoracic spine. Spine (Phila Pa 1976). 2005; 30:1283–1286.

19. Cho KJ, Kim YT, Shin SH, Suk SI. Surgical treatment of adult degenerative scoliosis. Asian Spine J. 2014; 8:371–381.

20. Cho KJ, Suk SI, Park SR, Kim JH, Jung JH. Selection of proximal fusion level for adult degenerative lumbar scoliosis. Eur Spine J. 2013; 22:394–401.

21. Shufflebarger H, Suk SI, Mardjetko S. Debate: determining the upper instrumented vertebra in the management of adult degenerative scoliosis: stopping at T10 versus L1. Spine (Phila Pa 1976). 2006; 31:S185–S194.
22. Kim YJ, Bridwell KH, Lenke LG, Rhim S, Kim YW. Is the T9, T11, or L1 the more reliable proximal level after adult lumbar or lumbosacral instrumented fusion to L5 or S1? Spine (Phila Pa 1976). 2007; 32:2653–2661.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download