Abstract
Purpose
To report our initial clinical cases of robotic laparoendoscopic single-site (R-LESS) partial nephrectomy (PN) performed with the use of the novel Da Vinci R-LESS platform.
Materials and Methods
Three patients underwent R-LESS PN from November 2013 through February 2014. Perioperative and postoperative outcomes were collected and intraoperative difficulties were noted.
Results
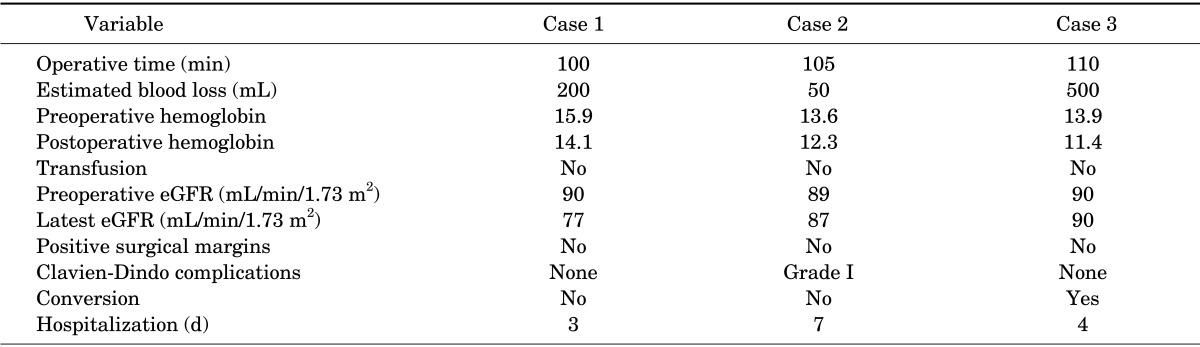
Operative time and estimated blood loss volume ranged between 100 and 110 minutes and between 50 and 500 mL, respectively. None of the patients was transfused. All cases were completed with the off-clamp technique, whereas one case required conversion to the conventional (multiport) approach because of difficulty in creating the appropriate scope for safe tumor resection. No major postoperative complications occurred, and all tumors were resected in safe margins. Length of hospital stay ranged between 3 and 7 days. The lack of EndoWrist movements, the external collisions, and the bed assistant's limited working space were noticed to be the main drawbacks of this surgical method.
Increasing experience in minimally invasive techniques has furthered an impetus in the urological community to reduce the invasiveness of laparoendoscopic renal surgery. Therefore, robotic laparoendoscopic single-site (R-LESS) partial nephrectomy (PN) has been introduced in an effort to achieve a cosmetic outcome superior to that of the conventional approach [1]. However, R-LESS PN is still more challenging and more complicated for surgeons than is conventional RPN, because the current Da Vinci robotic platform (Intuitive Surgical Inc., Sunnyvale, CA, USA) is not designed to be used in this kind of procedure [2].
In our practice, we have commonly used a homemade device adapted to an Alexis wound retractor to perform R-LESS PN [3]. However, we have experienced many difficulties during surgery, such as fragility of the device, significant gas leaks, and collision of the internal and external instruments [3]. Recently, Intuitive Surgical Inc. developed and commercialized the Da Vinci R-LESS device and instruments with a goal of decreasing the surgical limitations that occur during the utilization of the available single-port devices [4].
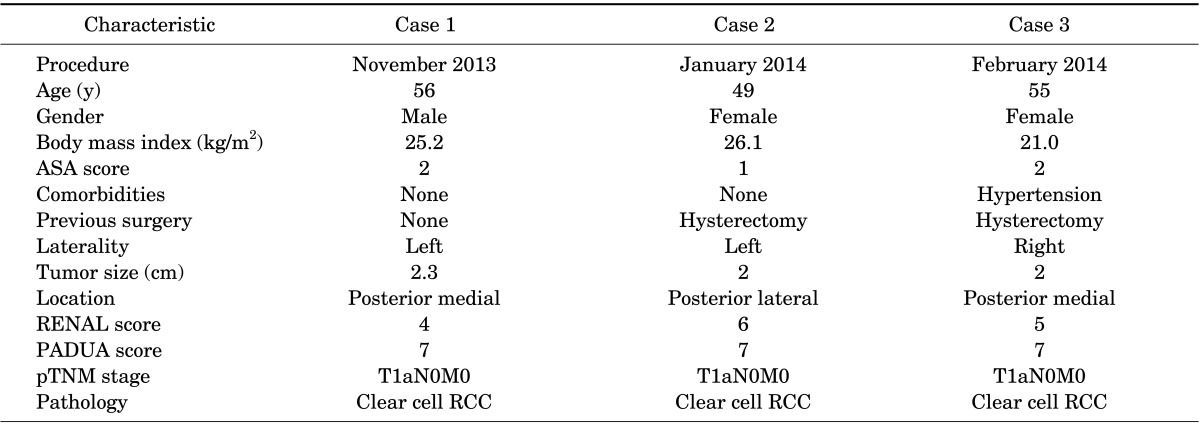
Since November 2013, a prospective analysis of the initial three patients who underwent R-LESS PN with use of the Da Vinci R-LESS platform was entered into an Institutional Review Board-approved database. Patient selection was based on the surgeon's clinical judgment. All tumors were identified on abdominal computed tomography scans. Perioperative and postoperative data were collected and analyzed. Both the PADUA and RENAL scoring systems were used to account for tumor complexity [8,9]. Each patient's estimated glomerular filtration rate (eGFR) was determined by using the Modification of Diet in Renal Disease formula [10]. Complications were recorded within 30 days postoperatively by using the modified Clavien-Dindo classification system [11]. Operative time was defined as the overall time that the surgeon needed to start and complete the operation, without including the docking process.
The Da Vinci R-LESS access device is a soft, silicon, reel-shaped port with four channels. Two channels accommodate curved cannulae for the flexible robotic instruments (VeSPA surgical instruments, Intuitive Surgical Inc.), and the third and fourth channels remain for the laparoscope and the assistant's instrument. The left robotic instrument is directed downward to the right, whereas the right one is directed downward to the left. Although the robotic instruments are crossed at the entrance site, the instruments are automatically reassigned by the system software, such that the left hand of the surgeon's control directs the left instrument and vice versa. The development of this "chopstick" surgical device hypothetically results in fewer collisions of the robotic arms [12].
After induction of general endotracheal anesthesia, the patients were placed in a 45-degree flank position with the ipsilateral side elevated and were secured to the operating table after the pressure points were padded. The table was tilted to position the patient supine and a 2.5-cm midline periumbilical incision was made and dissected deep to the rectus fascia, down through the peritoneum. Access to the peritoneum was then obtained and the Da Vinci single-port device was inserted through the incision in the peritoneal cavity.
Pneumoperitoneum was established up to 15 mmHg and the camera port was inserted. A 30° camera viewing angle was used to minimize clashing between the robotic scope and instruments externally. The Da Vinci Si system was docked by using a 3-arm configuration and the curved cannulae ports were inserted and docked under vision. Robotically controlled instruments included a semirigid cautery hook, curved scissors, needle holders, and a Cadiere grasper. During the procedure, the bedside assistant had the ability to use a suction irrigator, a laparoscopic grasper, and a clip applier. The surgical steps included tumor identification, tumor excision, and renorrhaphy by using the sliding clip technique. Laparoscopic ultrasound with TilePro projection (Intuitive Surgical Inc.) onto the console screen was introduced through the assistant port to confirm the tumor margin and depth. Frozen biopsies of renal parenchyma from the base of the operative bed were always obtained. Our surgical technique is demonstrated in a supplementary video clip (Supplementary material).
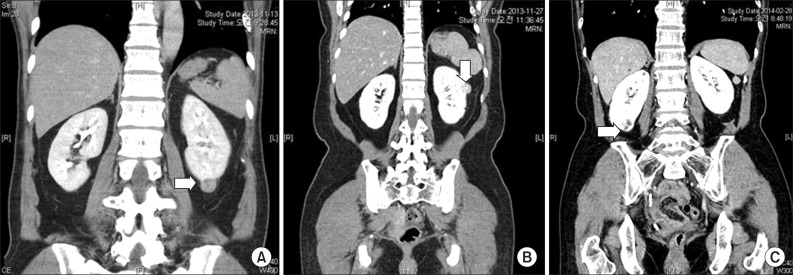
Case 1 had a 2.3-cm tumor located on the lower pole of the left kidney, case 2 a 2-cm mass located on the mid portion of the left kidney, and case 3 a 2-cm tumor on the lower pole of the right kidney (Fig. 1A-C).
The clinical and demographic characteristics of the three patients are summarized in Table 1. All the tumors were located on the posterior surface of the kidneys and the renal scores were 4, 6, and 5, respectively.
All the procedures were completed without clamping the renal vessels. No additional ports were used in any case. Operative time ranged from 100 to 110 minutes, and estimated blood loss volume ranged from 50 to 500 mL. None of the patients was transfused. We did not detect positive surgical margins in any of the cases. One patient (case 2) developed atelectasis, which resulted in prolonged hospitalization (a grade I complication according to the Clavien-Dindo classification system). One case (case 3) was converted to a multiport procedure owing to intraoperative difficulty of resecting the tumor. Table 2 shows the perioperative and postoperative outcomes of the subjects.
The Da Vinci R-LESS platform (Intuitive Surgical Inc.) has recently been used for pyeloplasty and radical nephrectomy procedures [5,6,7]. However, regarding R-LESS PN, only procedures performed in cadaver models have been described with the use of the novel Da Vinci platform [13]. RPN remains a challenging procedure even for the conventional approach; therefore, it is difficult to apply novel techniques in humans. To our knowledge, the current study is the first report of clinical experience with PN by use of this new technology.
According to the literature, LESS surgery is technically feasible and safe for various urologic diseases, results in better cosmetic outcome, has a lower postoperative analgesic requirement, and is associated with faster convalescence than is conventional laparoscopy [1,14]. However, the oncological and surgical safety of a procedure is more important. In a recently published article, we demonstrated that safety, estimated with Trifecta achievement, is inferior in R-LESS PN compared with the conventional approach [3]. Therefore, we concluded that R-LESS PN in the current fashion should be offered only to selected patients with low complexity and small tumors. These results were also reported by other studies, whereas European association guidelines recommend that LESS PNs should be performed only as part of a clinical study [15,16]. This is logical, because it is admitted worldwide that the current Da Vinci system (Intuitive Surgical Inc.) is not designed to be used in this kind of procedure.
Intuitive Surgical Inc. developed a novel set of single-site instruments and accessories specifically dedicated to LESS in an attempt to overcome the current limitations [4]. However, the drawbacks of the existing configuration of robotic arms and the use of a bulky robot in this kind of surgery remain. Therefore, although the current Da Vinci platform has been shown to be a valuable ally in LESS surgery, the ideal robotic platform for LESS is still lacking and more advanced equipment is requisite.
According to our experience, even though the procedures were performed safely, we encountered many difficulties during the surgery. First, the lack of EndoWrist technology at the instrument tips results in difficult tumor excision and renal bed reconstruction, while intracorporeal suturing is more challenging. Second, the availability of monopolar and bipolar instruments is limited. Moreover, the external collisions of the instruments and the restricted assistant's motions due to the narrow space make the hilum dissection and the specimen extraction more complicated. In addition, we observed a frequent loss of pneumoperitoneum, as a result of leakage from the device, and fragile material. Finally, the inability to use the fourth robotic arm makes the resection of posteriorly located tumors harder owing to the insufficient tissue retraction. As a result, we needed to convert one case into a conventional approach, although tumor complexity was not a deterrent for R-LESS surgery.
Gas leakage and tearing of the device were also reported by Kroh et al. [17], and almost all studies refer to the lack of EndoWrist movements, the bed assistant's limited working space, and the multiple collisions between the robotic arms as the main drawbacks [7,13]. In our opinion, improvement of the current R-LESS surgery to overcome these limitations can be achieved with the development of articulating instruments, a device with resistant material and a low external profile and wider internal rim, and repositioning of the assistant port below the camera port. The 30° laparoscope is also necessary to minimize internal conflicts between the surgical instruments and the optical system.
R-LESS PN in the current design can be effectively performed in centers with significant expertise, but careful patient selection appears to be a very important consideration. However, further significant improvements, along with more studies, are needed to develop the ideal R-LESS robotic platform. The development of novel platforms specific for R-LESS surgery is essential to overcome the current limitations and to promote the widespread use of this system.
References
1. Park SK, Olweny EO, Best SL, Tracy CR, Mir SA, Cadeddu JA. Patient-reported body image and cosmesis outcomes following kidney surgery: comparison of laparoendoscopic single-site, laparoscopic, and open surgery. Eur Urol. 2011; 60:1097–1104. PMID: 21856076.

2. Minervini A, Siena G, Serni S, Carini M. Robotic laparoendoscopic single-site partial nephrectomy: almost like driving with the steering lock engaged. Eur Urol. 2013; 12. 11. [Epub]. http://dx.doi.org/10.1016/j.eururo.2013.11.048.
3. Komninos C, Shin TY, Tuliao P, Yoon YE, Koo KC, Chang CH, et al. R-LESS partial nephrectomy trifecta outcome is inferior to multiport robotic partial nephrectomy: comparative analysis. Eur Urol. 2013; 11. 11. [Epub]. http://dx.doi.org/10.1016/j.eururo.2013.10.058.

4. Haber GP, White MA, Autorino R, Escobar PF, Kroh MD, Chalikonda S, et al. Novel robotic da Vinci instruments for laparoendoscopic single-site surgery. Urology. 2010; 76:1279–1282. PMID: 20980046.

5. Cestari A, Buffi NM, Lista G, Lughezzani G, Larcher A, Lazzeri M, et al. Feasibility and preliminary clinical outcomes of robotic laparoendoscopic single-site (R-LESS) pyeloplasty using a new single-port platform. Eur Urol. 2012; 62:175–179. PMID: 22469392.

6. Buffi NM, Lughezzani G, Fossati N, Lazzeri M, Guazzoni G, Lista G, et al. Robot-assisted, single-site, dismembered pyeloplasty for ureteropelvic junction obstruction with the new da Vinci platform: a stage 2a study. Eur Urol. 2014; 3. 13. [Epub]. http://dx.doi.org/10.1016/j.eururo.2014.03.001.

7. Mathieu R, Verhoest G, Vincendeau S, Manunta A, Bensalah K. Robotic-assisted laparoendoscopic single-site radical nephrectomy: first experience with the novel Da Vinci single-site platform. World J Urol. 2014; 32:273–276. PMID: 24022235.

8. Ficarra V, Novara G, Secco S, Macchi V, Porzionato A, De Caro R, et al. Preoperative aspects and dimensions used for an anatomical (PADUA) classification of renal tumours in patients who are candidates for nephron-sparing surgery. Eur Urol. 2009; 56:786–793. PMID: 19665284.

9. Kutikov A, Uzzo RG. The R.E.N.A.L. nephrometry score: a comprehensive standardized system for quantitating renal tumor size, location and depth. J Urol. 2009; 182:844–853. PMID: 19616235.

10. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. Modification of Diet in Renal Disease Study Group. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med. 1999; 130:461–470. PMID: 10075613.

11. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213. PMID: 15273542.
12. Joseph RA, Goh AC, Cuevas SP, Donovan MA, Kauffman MG, Salas NA, et al. "Chopstick" surgery: a novel technique improves surgeon performance and eliminates arm collision in robotic single-incision laparoscopic surgery. Surg Endosc. 2010; 24:1331–1335. PMID: 20033723.

13. Kaouk JH, Autorino R, Laydner H, Hillyer S, Yakoubi R, Isac W, et al. Robotic single-site kidney surgery: evaluation of second-generation instruments in a cadaver model. Urology. 2012; 79:975–979. PMID: 22446346.

14. Choi KH, Ham WS, Rha KH, Lee JW, Jeon HG, Arkoncel FR, et al. Laparoendoscopic single-site surgeries: a single-center experience of 171 consecutive cases. Korean J Urol. 2011; 52:31–38. PMID: 21344028.

15. Autorino R, Kaouk JH, Yakoubi R, Rha KH, Stein RJ, White WM, et al. Urological laparoendoscopic single site surgery: multi-institutional analysis of risk factors for conversion and postoperative complications. J Urol. 2012; 187:1989–1994. PMID: 22498207.
16. Merseburger AS, Herrmann TR, Shariat SF, Kyriazis I, Nagele U, Traxer O, et al. EAU guidelines on robotic and single-site surgery in urology. Eur Urol. 2013; 64:277–291. PMID: 23764016.

17. Kroh M, El-Hayek K, Rosenblatt S, Chand B, Escobar P, Kaouk J, et al. First human surgery with a novel single-port robotic system: cholecystectomy using the da Vinci Single-Site platform. Surg Endosc. 2011; 25:3566–3573. PMID: 21638179.

SUPPLEMENTARY MATERIALS
Accompanying video clip can be found in the 'Urology in Motion' section of the journal homepage (www.kjurology.org). The supplementary video clip can also be accessed by scanning a QR code located on the title page of this article, or be available on YouTube (http://youtu.be/XdlmCuw3Er8).




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download