Abstract
Urological involvement of hepatocellular carcinoma (HCC) is rare; HCC arising in an orthotopic liver transplant (OLT) is exceptionally rare. Here we report the case of a 70-year-old man who was incidentally found to have metastatic HCC in the right kidney arising from his OLT undertaken for cryptogenic cirrhosis 10 years previously. Adding to the complexity of this case was the lack of an obvious liver primary HCC at the time of the radical nephrectomy, thus making the final diagnosis all but impossible. We believe this report represents the first report of HCC metastasizing to the kidney after OLT and adds to the few reports in the literature of HCC arising in transplanted livers.
Hepatocellular carcinoma (HCC) is one of the most common malignancies globally and accounts for nearly 1 million new cases per year [1]. The most frequent metastatic sites for HCC include the lung, lymph nodes, bones, and adrenal glands. Primary tumors that commonly metastasize to the kidney are lung (19.8%), breast (12.3%), stomach (11.1%), and contralateral kidney (8.6%) tumors [2]. Metastatic HCC to the kidney is very rare. The incidence of de novo HCC after an orthotopic liver transplant (OLT) is extremely rare, with an estimated incidence of 25 per 100,000 person-years [3]. Thus, two rare events occurred in the same patient in the present case report, with a further anomaly being the lack of an obvious primary liver HCC at the time of the radical nephrectomy. Here we report this case of renal metastasis of HCC arising in the recipient's transplanted liver 10 years after transplantation for cryptogenic cirrhosis.
A 70-year-old man presented with an incidental right renal mass after magnetic resonance cholangiopancreatography (MRCP) for investigation of abnormal results of liver function tests (LFTs), which suggested an obstructed biliary tree. The patient had undergone OLT in 2000 after extensive preoperative investigations for cryptogenic liver cirrhosis including serology and radiology. Post-OLT histopathology showed that the native liver had nodules of varying sizes consistent with cirrhosis with no evidence of carcinoma. The patient was started on immunosuppressive therapy with tacrolimus, which was subsequently changed to sirolimus in 2005, and he was followed up quarterly by the liver transplant service at our center.
On routine follow-up, the patient was found to have obstructive (cholestatic) LFT results in late 2009. An MRCP was performed and a diagnosis of choledocholithiasis was made, but incidentally a right renal mass was also found. No biliary tree obstruction or liver lesions were noted on this scan. A triple-phase computed tomographic (CT) scan of his abdomen and pelvis further confirmed the presence of a lobulated enhancing mass (55 mm×45 mm in diameter) in the right upper pole extending into the perinephric fat and abutting the right hemidiaphragm (Fig. 1A, B) but with a clear plane between the liver and the mass. Again, the hepatobiliary system had no lesions present. He was otherwise asymptomatic with all staging negative for metastatic disease. His case was reviewed at a multidisciplinary meeting where consensus dictated that the mass was likely to represent a primary renal tumor that should be resected. Partial nephrectomy was offered but declined by the patient.
The patient underwent a right open radical nephrectomy via a flank approach and resection of part of the hemidiaphragm requiring repair with a synthetic mesh (Gore-Tex patch). There were no obvious liver lesions on careful inspection and palpation. The procedure resulted in 500 mL of blood loss and no perioperative complications. Histology of the specimen revealed a tumor with hepatoid morphology (Fig. 2) invading the upper pole of the kidney, perinephric fat, and diaphragm. Immunohistochemical staining (positive for HepPar 1 and polyclonal carcinoembryonic antigen) was also suggestive of HCC. The patient was discharged but 5 months later it was noted that his serum alpha-fetoprotein levels were significantly elevated and abnormal serum baseline liver function was declining. An ultrasound demonstrated six previously undetected focal liver lesions. A CT scan further confirmed the liver lesions, which continued to enlarge (Fig. 1C). At restaging, new pulmonary lesions were also noted (Fig. 1D). After a multidisciplinary meeting, the patient was commenced on the tyrosine kinase inhibitor sorafenib in a bid to control his overt metastatic disease, which at 3 months has stabilized.
Most renal metastases are clinically silent as was observed in this report. Primary tumors of the lung, breast, and gastrointestinal tract are the most common sources of renal metastases [4]. Other sources include the cervix, prostate, gall bladder, thyroid, ovary, testis, urinary bladder, contralateral kidney, and bone [4]. Renal metastasis, however, is an uncommon site for HCC. In a search of the literature using MEDLINE, Embase, and Google scholar with cascading from returned manuscripts, we found fewer than 15 reported cases of HCC with renal metastasis in a living patient.
Increased risk of de novo malignancies is a serious long-term complication following liver transplantation. Nonmelanoma skin malignancies are the most frequent types of cancer occurring in the post-OLT setting, with age, cumulative years after OLT, and use of immunosuppression as independent risk factors [5]. We report the first case of renal metastasis of HCC after OLT.
What was interesting about our case was that our patient underwent liver transplant for cryptogenic cirrhosis after an extensive preoperative workup to exclude HCC. Histological examination of the native liver was also confirmed to show only cirrhosis without any evidence of carcinoma.
The patient was also on tacrolimus after OLT for 5 years and then switched to sirolimus. Although the role of systemic immunosuppression in promoting posttransplant tumors is not clearly defined, clinical evidence supports the effect of cyclosporine and tacrolimus in impairing cellular immunity and tumor cell surveillance at the time of liver transplantation [6]. An elevation in tumor incidence was also observed in liver transplant patients on either tacrolimus- or cyclosporine-based regimens [7].
Needle biopsies performed under CT guidance appear to be safe (with a minimal risk of bleeding or of seeding of the needle tract with malignant cells), and they have a sensitivity for the detection of cancer of 80% to 92% and a specificity of 83% to 100% [8]. We do not routinely biopsy lesions that will definitely undergo surgery as in this case, and although it may have been useful to know, his staging and in particular liver imaging was negative and he had no prior history of malignancy. Thus, we do not believe biopsy would have changed his management.
Flemming et al. [9] reported a case of HCC originating from the donor liver that was identified by an allelic pattern of the donor and the recipient. Saxena et al. [10] also confirmed the de novo origin of HCC by the difference in the donor's sex chromosome from that of the recipient. Although we did not perform such genetic analysis, the clinical course of the patient is highly suggestive of HCC that arose in the donor allograft.
In conclusion, a differential diagnosis of metastatic HCC should be kept in mind in a patient presenting with a renal mass with history of liver transplantation and immunosuppression. However, in reality, this is rare and perhaps if any lesions in the liver are present, including small ones, a biopsy should be considered. If nephrectomy is considered, the surgery may be more extensive in the case of metastatic disease but is certainly possible with the involvement of hepatobiliary surgeons, particularly where liver involvement is suspected.
Figures and Tables
FIG. 1
(A) Computed tomography arterial phase coronal view showing the isolated right renal mass (arrow) measuring 55 mm×45 mm in the upper pole abutting the hemidiaphragm. (B) Computed tomography venous phase axial view. The liver appears separate from the renal mass. (C) Computed tomography demonstrating ill-defined low-attenuation lesions (arrows) in the liver consistent with hepatocellular carcinoma, 5 months after the nephrectomy. (D) Computed tomography of the chest demonstrating multiple new pulmonary metastases 5 months after nephrectomy.
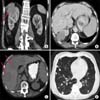
FIG. 2
Histopathology. (A) Hepatoid cells with large nuclei (×40); (B) section showing positive cytoplasmic staining for Hep-Par 1 (×100); (C) positive staining for polyclonal carcinoembryonic antigen (pCEA) (×100). Hep-Par 1 is a hepatocyte-specific antibody with an 82% sensitivity and 90% specificity for diagnosis of hepatocellular tumors. The usefulness of Hep-Par 1 is enhanced when it is combined with pCEA.

References
1. Cormier JN, Thomas KT, Chari RS, Pinson CW. Management of hepatocellular carcinoma. J Gastrointest Surg. 2006; 10:761–780.
2. Wagle DG, Moore RH, Murphy GP. Secondary carcinomas of the kidney. J Urol. 1975; 114:30–32.
3. Hoffmann CJ, Subramanian AK, Cameron AM, Engels EA. Incidence and risk factors for hepatocellular carcinoma after solid organ transplantation. Transplantation. 2008; 86:784–790.
4. Mayer RJ. Infiltrative and metastatic disease of the kidney. In : Rieselbach RE, Garnick MB, editors. Cancer and the kidney. Philadelphia: Lea & Febiger;1982. p. 707.
5. Saigal S, Norris S, Muiesan P, Rela M, Heaton N, O'Grady J. Evidence of differential risk for posttransplantation malignancy based on pretransplantation cause in patients undergoing liver transplantation. Liver Transpl. 2002; 8:482–487.
6. Yokoyama I, Takagi H. Liver transplantation and hepatocellular carcinoma. Semin Surg Oncol. 1996; 12:212–216.
7. Jonas S, Rayes N, Neumann U, Neuhaus R, Bechstein WO, Guckelberger O, et al. De novo malignancies after liver transplantation using tacrolimus-based protocols or cyclosporinebased quadruple immunosuppression with an interleukin-2 receptor antibody or antithymocyte globulin. Cancer. 1997; 80:1141–1150.
8. Volpe A, Kachura JR, Geddie WR, Evans AJ, Gharajeh A, Saravanan A, et al. Techniques, safety and accuracy of sampling of renal tumors by fine needle aspiration and core biopsy. J Urol. 2007; 178:379–386.
9. Flemming P, Tillmann HL, Barg-Hock H, Kleeberger W, Manns MP, Klempnauer J, et al. Donor origin of de novo hepatocellular carcinoma in hepatic allografts. Transplantation. 2003; 76:871–873.
10. Saxena R, Ye MQ, Emre S, Klion F, Nalesnik MA, Thung SN. De novo hepatocellular carcinoma in a hepatic allograft with recurrent hepatitis C cirrhosis. Liver Transpl Surg. 1999; 5:81–82.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download