Abstract
Purpose
We developed an inverse technique for tissue morcellation by modifying the conventional upward technique and then examined its safety and efficiency.
Materials and Methods
From July 2008 to December 2010, a total of 389 consecutive patients treated with holmium laser enucleation of the prostate (HoLEP) were enrolled in this study. For tissue morcellation, we used an upward technique for an initial series of 84 patients and an inverse technique for a consecutive series of 305 patients. We compared efficiency and safety between the inverse technique and the upward technique.
Results
There were no significant differences in mean age or prostate volume between the two groups. The mean morcellation efficiency was higher in the inverse technique group. The incidence of severe bladder injury was significantly higher in the upward technique group. Regarding the site of bladder injury, 7 and 4 cases of bladder injury occurred in the bladder dome and posterior wall, respectively, in the upward technique group. In the inverse technique group, however, the site of bladder injury was limited to the trigone. We divided our clinical series of patients into the upward technique group and three inverse technique groups on the basis of the timing. The mean morcellation efficiency was significantly higher in all three inverse technique groups than in the upward technique group. However, there was no significant difference in mean morcellation efficiency between the three inverse technique groups.
In patients with bladder outlet obstruction (BOO) due to benign prostatic hyperplasia (BPH), transurethral resection of the prostate (TURP) has long been considered a standard treatment regimen [1]. In 1995, Gilling first introduced holmium laser prostatectomy for the treatment of BPH. Since then, holmium laser enucleation of the prostate (HoLEP) has been increasingly performed [2]. HoLEP is advantageous in that it can be performed both effectively and safely with no respect to the size of prostate. As compared with open prostatectomy or TURP, HoLEP shows a lower morbidity and a shorter length of hospital stay [3-5]. It is composed a two-stage procedure: enucleation and morcellation. To date, however, most studies have focused on enucleation and its outcomes.
Given the above background, we developed an inverse technique for tissue morcellation by modifying the conventional upward technique and then examined its safety and efficiency.
The current study was conducted in 389 patients (n=389) with BPH who underwent HoLEP between July 2008 and December 2010. For tissue morcellation, we used an upward technique for an initial series of 84 patients during a period from July 2008 to June 2009 and an inverse technique for a consecutive series of the remaining 305 patients between July 2009 and December 2010. In the current study, the inclusion criteria were an International Prostate Symptom Score (IPSS) of ≥8, a peak urinary flow rate (Qmax) of ≤15 ml/sec, and significant postvoid residual (PVR) urine volume. In addition, the exclusion criteria were prostate cancer, neurogenic bladder, and urethral surgery. A prostate biopsy was done, if clinically applicable, to rule out the possibility of prostate cancer. All surgical procedures were done by a single surgeon (JBL). Before HoLEP, all patients underwent a digital rectal examination, serum prostate-specific antigen (PSA) measurement, transrectal ultrasonography, uroflowmetry, and residual urine measurement and IPSS and quality of life (QoL) scores were determined.
HoLEP was done preferably under spinal anesthesia and was composed of two maneuvers: enucleation of prostate adenoma and morcellation of adenoma tissue within the bladder. Our methods of enucleation followed previous reports [6-8]. The mechanical morcellator device is constructed of a handpiece and blades (the outer sheath and inner sheath). The inner sheath aspires the tissue, which is followed by the morcellation of the tissue by a sharp portion between the outer sheath and the inner one. The tissue morcellation is performed as follows. First, a resectoscope is replaced with a nephroscope following enucleation. When surgeons notice that the bladder is sufficiently filled and then remote from the bladder mucosa, they place a resectoscope central to the bladder. The morcellator contains a two-phase foot pedal. By sharp pressing of the pedal, surgeons capture the tissue through a suction function. This is followed by the morcellation of the captured tissue by the blades by full pressing of the pedal [7,8]. With the use of the currently commercially available form of the morcellator, the most important detail is the shape of the tip of the morcellator. Holes are created proximal to the tip of the outer sheath. Similarly, the inner sheath also has a semi-tubular shape. To prevent the aspiration of the bladder mucosa from the tip of the morcellator, the morcellator was designed to have a blind-ended tip of the inner sheath. When surgeons discontinue operation of the morcellator, they can adjust the location of the blades. Surgeons should be aware that there is a complete lack of aspiration if they halt the tip of the inner sheath before the holes made in the outer sheath. The conventional method of tissue morcellation, that is, the upward technique, is operated when the blades are directed upwards and the tissue is first aspirated from their superior part. Thus, the morcellation of tissue is accomplished [8]. In the current study, we used an inverse technique, a modified form of the conventional upward technique, for 305 patients excluding an initial series of 84 patients. In the inverse technique, the prostate tissue is aspirated and then captured superiorly by inversely placing the blades inferior to the bladder and superior to the prostate tissue (Fig. 1).
The VersaPulse Power Suite (Lumenis, Yokneam, Israel) holmium laser was used for enucleation of prostatic adenoma at a laser power of 80 to 100 W. In addition, a 26-Fr resectoscope (Karl Storz, El Segundo, CA, USA) with a laser bridge was used. The tissue morcellation was performed by using a percutaneous nephrolithotomy nephroscope and a VersaCut morcellator (Lumenis).
Between the upward technique group and the inverse technique group, we compared the mean morcellation time, the morcellation efficiency, the incidence and location of bladder injury occurring during the morcellation, and the catheter time. To rule out the possibility of a learning curve, we excluded an initial series of 20 patients. Then, we divided our clinical series of patients into the upward technique group and three inverse technique groups on the basis of the timing of the inverse technique: group 1 (early stage), group 2 (middle stage), and group 3 (late stage). This was followed by a comparison of the morcellation efficiency between the four groups. In addition, on the basis of a cutoff value of 50 g, we divided our clinical series of patients into two groups: a group with a prostate size of ≥50 g and a group with a prostate size of <50 g. Then, we compared the mean morcellation time, the morcellation efficiency, the incidence and location of bladder injury occurring during the morcellation, and the catheter time between the two groups.
The mean values of continuous variables were used in the analysis, for which ranges are presented in parentheses. Data are expressed as mean±standard deviation. The unpaired Student's t-test was used to analyze the differences in mean values between the four groups. In addition, the Mann-Whitney U test was used to analyze non-normally distributed continuous variables. A p-value of <0.05 was considered statistically significant.
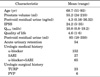
The baseline characteristics of the patients are presented in Table 1. There were no significant differences in mean age or prostate volume between the two groups. The mean morcellation time was 14.3±8.6 minutes in the upward technique group and 6.4±7.2 minutes in the inverse technique group. The morcellation efficiency was 1.93±1.14 g/min and 4.03±0.89 g/min in the two groups, respectively. Thus, the degree of morcellation efficiency was significantly higher in the inverse technique group (p<0.05). There were 11 cases (13.1%) and 4 cases (1.3%) of bladder injury during the morcellation, respectively. In particular, there were 5 cases (5.9%) and 1 case (0.3%) of severe bladder injury in the corresponding order, for which a urethral catheter was required for more than 3 days postoperatively. That is, the incidence of severe bladder injury was significantly higher in the upward technique group. Regarding the site of bladder injury, 7 cases (63.6%) and 4 cases (36.4%) of bladder injury occurred in the bladder dome and the posterior wall, respectively, in patients in the upward technique group. In the inverse technique group, however, the site of bladder injury was limited to the trigone (Table 2).
To rule out the possibility of a learning curve, we excluded an initial series of 20 patients. Then, we divided our clinical series of patients into the upward technique group and three inverse technique groups on the basis of the timing of the inverse technique. The mean morcellation efficiency was 2.15±0.82 g/min, 3.95±0.91 g/min, 3.71±1.56 g/min, and 3.83±1.35 g/min in the upward technique group and in groups 1, 2, and 3 of the inverse technique group, respectively. Thus, morcellation efficiency was significantly higher in all three inverse technique groups than in the upward technique group. There was no significant difference in the mean morcellation efficiency between the three inverse technique groups (Table 3). Using the cutoff value of 50 g, we divided our clinical series of patients into two groups: the group with a prostate size of ≥50 g and that with a prostate size of <50 g. Then, we compared the mean morcellation efficiency between the two groups. This comparison showed that morcellation efficiency was 2.8±0.97 g/min in the group with a prostate size of <50 g and 3.5±0.75 g/min in the group with a prostate size of ≥50 g. In addition, there were six cases and nine cases of bladder injury, respectively. Furthermore, the mean morcellation efficiency and the incidence of bladder injury were significantly higher in the group with a prostate size of <50 g than in the group with a prostate size of ≥50 g. However, this difference was not statistically significant (Table 4).
Recently, it has been increasingly reported that HoLEP can be used as an alternative to the traditional BPH surgery [9]. The HoLEP technique consists of a two-stage procedure: enucleation for removal of adenoma along the surgical capsule and morcellation for the aspiration and removal of the adenoma tissue in the urinary bladder. With the development of a morcellator, it has become possible to perform surgery for patients with large-sized BPH [4,10,11]. Compared with the traditional treatment regimens for BPH, that is, TURP and open prostatectomy, HoLEP has been reported to cause lower morbidity and similar or better postoperative outcomes [4,12]. Despite these advantages, the HoLEP procedure has the disadvantage of a learning curve that is not easily overcome. Several studies have reported that time and experience are needed to overcome the learning curve [13-16]. According to many currently published articles about HoLEP, the upward technique is recommended to aspirate the adenoma superiorly to the blades of a morcellator before the morcellation of adenoma. This is commonly used in a clinical setting [7,8]. In this upward technique, it is not actually easy to put the large extracted tissue on the blades with the thin shape of the rod in a narrow visual field. It is therefore highly probable that this might lead to careless operation of the blades in a place remote from the endoscope in a poor visual field because the blades have a penetrating appearance on the tip of an endoscope. We have therefore used the inverse technique by inversely rotating both the nephroscope and the blades. This makes it possible to aspirate the tissue bladder mucosa inferiorly. In addition, there is a visual field of the endoscope between the blades and the tissue. This makes it easier not only to confirm the aspirated tissue but also to minimize unnecessary manipulation to put the tissue on the blades. Thus, the morcellation efficiency can be raised. This is also accompanied by decreased risks of damaging the bladder mucosa during the morcellation. In the current study, we compared the mean morcellation time, the incidence of bladder injury, and catheter time between the upward technique group and the inverse technique group. This showed that these values were significantly lower in the inverse technique group. In addition, the morcellation efficiency was also significantly higher with the inverse technique. Regarding the sites of occurrence of bladder injury, the tissue is aspirated when the blades are directed downward toward the urinary bladder. Therefore, all the injuries occurred in the bladder trigone. This indicates that the inverse technique is relatively safe and has a lower risk of bladder perforation than does the upward technique, which was associated with the occurrence of bladder injury in the bladder dome and the posterior wall (Table 2).
Unlike enucleation, it has been reported that the morcellation is not subject to a learning curve. Shah et al. compared the morcellation efficiency in 16 groups (10 patients assigned to the first 15 groups each and 12 assigned to the final 16th group). But these authors reported that morcellation efficiency showed no great changes and was not increased with experience [15]. Moreover, Seki et al. [16] also compared the morcellation efficiency in seven groups (10 patients assigned to seven groups each). These authors noted that the value of morcellation efficiency was increased but this was not statistically significant. Bae et al. [17] compared the morcellation efficiency between an initial series of 60 patients (20 patients assigned to three groups each). These authors reported that the value of morcellation efficiency was significantly increased by 0.61 g/min, 1.70 g/min, and 2.03 g/min in the corresponding order (p<0.001). They also noted that 20 cases were required for the adaptation to the morcellation procedure. In the current study, to rule out the possibility of a morcellation learning curve, we divided our clinical series of patients into four groups that excluded an initial series of 20 patients: the upward technique (n=64) group and three inverse technique groups that were based on the timing of the procedure. Then, we compared the morcellation efficiency between the four groups. This showed that there was a significant difference in the morcellation efficiency (p<0.05). This suggests that a significant difference in the morcellation efficiency between the upward technique group and the three inverse technique groups did not originate from the morcellation learning curve (Table 3). The morcellation efficiency was significantly higher in the inverse technique group than in the upward technique group. This was due to the following reasons:
1) The inverse technique can shorten the length of time for urologic surgeons to put the tissue on the blades during the morcellation.
2) The inverse technique can prevent the tissue from interfering with the visual field in the posterior wall of the bladder during the morcellation.
3) The inverse technique can maintain the distance between the blades and the bladder wall to a sufficient extent, thus continuing the morcellation with no interruptions. This can eventually shorten the morcellation time.
Ishikawa et al. [18], who first introduced the inverse technique, performed HoLEP surgery for 140 patients with BPH during a period ranging from January to December 2010. According to those authors, the mean morcellation time and mean morcellation efficiency were 9.9 minutes and 6.7 g/min, respectively. In addition, they also noted that there were no complications such as bladder injury during the morcellation. Furthermore, they also reported that there was a decreasing tendency in the morcellation efficiency in patients with a weight of enucleated tissue of >80 g. Furthermore, the morcellation efficiency was significantly poor in patients with a weight of enucleated tissue of >100 g. In the current study, we compared the morcellation efficiency and the incidence of bladder injury during the morcellation according to prostate size. This comparison showed that both values were higher in the group with a prostate size of ≥50 g than in the group with a prostate size of <50 g. However, this was not statistically significant (Table 4).
There are limitations of the current study as shown below:
1) The current study was conducted under a retrospective cross-sectional design. This limits an accurate comparison between the different subsets of patients.
2) A smaller number of patients underwent the upward technique as compared with the inverse technique. Moreover, the complications occurred at a lower incidence during the morcellation in both groups (the upward technique group and the inverse technique group). Therefore, this might produce a bias in the statistical significance.
Theoretically, morcellation is a simple procedure for HoLEP. In practice, however, it is one of the complicated procedures of this surgical modality and requires special attention. This is because the tissue morcellation is accomplished by using mechanical devices. Urologic surgeons should therefore be careful not to cause complications such as bladder mucosal injury or perforation. As described in the current study, the inverse technique might be a more effective, safer, and more excellent method of morcellation as compared with the conventional upward technique.
Figures and Tables
FIG. 1
(A) Upward technique: adenoma is aspirated superiorly after the blades are placed superior to the urinary bladder, which is followed by the morcellation. (B) Inverse technique: adenoma is aspirated inferiorly after the blades are placed inferior to the urinary bladder, which is followed by the morcellation.

TABLE 2
Comparison of operative data of the morcellation between the upward and inverse (downward) techniques

References
1. AUA Practice Guidelines Committee. AUA guideline on management of benign prostatic hyperplasia (2003). Chapter 1: Diagnosis and treatment recommendations. J Urol. 2003. 170(2 Pt 1):530–547.
2. Gilling PJ, Cass CB, Malcolm AR, Fraundorfer MR. Combination holmium and Nd:YAG laser ablation of the prostate: initial clinical experience. J Endourol. 1995. 9:151–153.
3. Montorsi F, Naspro R, Salonia A, Suardi N, Briganti A, Zanoni M, et al. Holmium laser enucleation versus transurethral resection of the prostate: results from a 2-center, prospective, randomized trial in patients with obstructive benign prostatic hyperplasia. J Urol. 2004. 172(5 Pt 1):1926–1929.
4. Kuntz RM, Lehrich K. Transurethral holmium laser enucleation versus transvesical open enucleation for prostate adenoma greater than 100 gm.:: a randomized prospective trial of 120 patients. J Urol. 2002. 168(4 Pt 1):1465–1469.
5. Elzayat EA, Elhilali MM. Holmium laser enucleation of the prostate (HoLEP): the endourologic alternative to open prostatectomy. Eur Urol. 2006. 49:87–91.
6. Gilling PJ, Kennett K, Das AK, Thompson D, Fraundorfer MR. Holmium laser enucleation of the prostate (HoLEP) combined with transurethral tissue morcellation: an update on the early clinical experience. J Endourol. 1998. 12:457–459.
7. Kuo RL, Paterson RF, Kim SC, Siqueira TM Jr, Elhilali MM, Lingeman JE. Holmium laser enucleation of the prostate (HoLEP): a technical update. World J Surg Oncol. 2003. 1:6.
8. Kelly DC, Das A. Holmium laser enucleation of the prostate technique for benign prostatic hyperplasia. Can J Urol. 2012. 19:6131–6134.
9. Reich O, Gratzke C, Stief CG. Techniques and long-term results of surgical procedures for BPH. Eur Urol. 2006. 49:970–978.
10. Gilling PJ, Kennett KM, Fraundorfer MR. Holmium laser enucleation of the prostate for glands larger than 100 g: an endourologic alternative to open prostatectomy. J Endourol. 2000. 14:529–531.
11. Moody JA, Lingeman JE. Holmium laser enucleation for prostate adenoma greater than 100 gm.: comparison to open prostatectomy. J Urol. 2001. 165:459–462.
12. Ahyai SA, Lehrich K, Kuntz RM. Holmium laser enucleation versus transurethral resection of the prostate: 3-year follow-up results of a randomized clinical trial. Eur Urol. 2007. 52:1456–1463.
13. Placer J, Gelabert-Mas A, Vallmanya F, Manresa JM, Menendez V, Cortadellas R, et al. Holmium laser enucleation of prostate: outcome and complications of self-taught learning curve. Urology. 2009. 73:1042–1048.
14. Elzayat EA, Elhilali MM. Holmium laser enucleation of the prostate (HoLEP): long-term results, reoperation rate, and possible impact of the learning curve. Eur Urol. 2007. 52:1465–1471.
15. Shah HN, Mahajan AP, Sodha HS, Hegde S, Mohile PD, Bansal MB. Prospective evaluation of the learning curve for holmium laser enucleation of the prostate. J Urol. 2007. 177:1468–1474.
16. Seki N, Mochida O, Kinukawa N, Sagiyama K, Naito S. Holmium laser enucleation for prostatic adenoma: analysis of learning curve over the course of 70 consecutive cases. J Urol. 2003. 170:1847–1850.
17. Bae J, Oh SJ, Paick JS. The learning curve for holmium laser enucleation of the prostate: a single-center experience. Korean J Urol. 2010. 51:688–693.
18. Ishikawa R, Shitara T, Wakatabe Y, Kubo S, Hirayama T, Fujita T, et al. Relationship between morcellation efficiency and enucleated tissue weight in holmium laser enucleation of the prostate (HoLEP) for patients with benign prostatic hyperplasia. Nihon Hinyokika Gakkai Zasshi. 2011. 102:675–678.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download