Chronic idiopathic thrombocytopenic purpura (ITP) is an autoimmune disease that is characterized by isolated thrombocytopenia resulting from degradation of autoantibody-coated platelets in the reticuloendothelial system. Diagnosis of this disease, which responds favorably to conventional therapy, is not challenging, and the disease usually has a benign clinical course. Bleeding-related symptoms consist of mild mucocutaneous bleeding such as purpura, gingival bleeding, and nosebleeds. Hematuria and gastrointestinal and intracranial bleeding are rarely seen hemorrhagic episodes that lead to more serious clinical manifestations [1-3]. Perirenal hematoma develops in association with spontaneous or traumatic vascular abnormalities and hemorrhagic diathesis and occasionally leads to a life-threatening clinical picture requiring urgent surgical intervention [2-7]. In this case report, we present for the first time the management of bilateral perirenal hematoma and distal ureteral stones that developed spontaneously in a patient undergoing treatment of ITP. We also evaluate the case in light of the literature.
CASE REPORT
A 57-year-old patient with a diagnosis of chronic ITP for 1 year was referred to our emergency department with complaints of left flank pain and diffuse petechial bleeding all over his body. A complete blood count revealed thrombocytopenia (4,000/mm3), which led to his admission into the clinics of internal medicine. On the third day of chronic ITP therapy, the patient developed macroscopic hematuria, and we consulted with the patient after the urinary system ultrasound revealed bilateral perirenal hematoma. We learned from his medical history that he had not previously had any complaints of gross hematuria. He had previously undergone extracorporeal shock wave lithotripsy (ESWL) because of a left ureteral distal stone. His general health state was good and his vital findings were stable. The physical examination revealed a relaxed abdominal region with left costovertebral angle tenderness in addition to diffuse petechiae all over his body. In his biochemical analysis, blood urea nitrogen (53 mg/dl), creatinine (3.2 mg/dl), and fasting blood sugar (167 mg/dl) levels were also measured. Escherichia coli was detected in the urine culture, and the urinalysis revealed microscopic hematuria and pyuria. The results of the complete blood count analysis were as follows: white blood cells 27,000/mm3, hemoglobin 12.2 g/dl, hematocrit 37.3%, platelet count 4,000/mm3, prothrombin time 16.6 seconds (9 to 14), and international normalized ratio 1.36 (0.8 to 1.19).
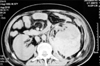
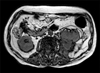
Owing to suddenly evolving macroscopic hematuria, the patient received prednisolone (80 mg/d) and intravenous immune globulin (0.5 g/kg/d) (KIOVIG 10 g/100 ml-Eczacıbaşı-Baxter), and an ultrasound examination of the urinary system demonstrated right and left perirenal hematoma and irregular renal contours. A non-contrast computed tomography (CT) scan was then performed. The CT scan revealed a right perirenal hematoma with dimensions of 21×20×42 mm, a 15-mm stone in the right distal ureter without any marked ectasia, a left perirenal hematoma with dimensions of 150×120×90 mm (Fig. 1), left distal ureteral ectasia, and a 20-mm distal ureteral stone (Fig. 2). The patient had an extremely low hematocrit (22%), hemoglobin (7.2 g/dl), and platelet counts (3,000/mm3) and received 6 IU erythrocytes and 3 IU platelets to improve his hematologic status. An operation was performed for his distal ureteral stones when his platelet counts reached 89,000/mm3. He was stone-free after bilateral ureterorenoscopy and pneumatic lithotripsy. There was no increase in the size of the hematoma, and regression was even shown on the postoperative control CT scan (Fig. 3). The patient was discharged under prednisolone therapy with necessary recommendations. His control magnetic resonance imaging study showed regression of the perirenal hematoma (Fig. 4), and his blood urea nitrogen was 25 mg/dl and his creatinine was 0.79 mg/dl after 1 year.
DISCUSSION
Chronic ITP is an acquired bleeding diathesis with an immune origin. The onset and clinical course of the disease show variations. Platelet counts and the severity of the disease are important predictors of potential symptoms. Mild and moderately severe forms of ITP are asymptomatic in the absence of trauma, whereas in severe cases of ITP, clinical manifestations consist mostly of mucocutaneous bleeding such as purpura, petechiae, nosebleeds, and gingival bleedings. Gastrointestinal bleeding, hematuria, and intracranial hemorrhages are relatively more severe conditions and occasionally fatal [1-3,6,7]. In a meta-analysis conducted by Cohen et al. [1] in 1,817 patients, the rate of age-adjusted fatal hemorrhage risk for patients who were younger than 40 years, between 40 and 60 years, and older than 60 years was 0.004, 0.012, and 0.130, respectively.
Spontaneous perirenal and subcapsular renal bleeding are rarely seen clinical manifestations that lead to serious problems. The most important etiologic factors are angiomyolipoma and renal cell carcinoma. Among other causes are chronic hemodialysis, vascular pathologies such as atherosclerosis and arteritis, anticoagulant therapy, and hemorrhagic diathesis [2,4-9]. Because the clinical course of the disease in patients with perirenal hematoma varies according to the severity of bleeding, the therapeutic approach is closely related to the clinical condition of the patient. In cases of persistent bleeding and a worsening general health state, surgical treatment predominates, whereas in patients with stable vital parameters, palliative treatment can be performed. None of the very rarely encountered cases of renal bleeding due to ITP reported mortality. In two cases we found during a literature search, bedrest, steroid therapy, and platelet suspensions were sufficient without the need for surgical management. According to the guidelines of the American Hematologic Association, hospitalization is required for patients with mucocutaneous bleeding and platelet counts less than 20.000/mm3; for candidates for surgery, the American Hematologic Association recommends increasing platelet counts to above 50.000/mm3.
Our case of bilateral perirenal hematoma secondary to ITP with a concurrent bilateral distal ureteral stone is the first such case report in the literature. In the management of distal ureteral stones, ESWL and ureteroscopic lithotripsy are effective and safe treatment modalities, but in patients with hemorrhagic diathesis, extreme care should be exercised for ESWL. In a case report presented in Japan, safe use of ESWL was mentioned in a ureteral stone patient with ITP [10]. In a study performed in patients with hemorrhagic diathesis, the frequency of severe perirenal bleeding secondary to ESWL was reported to be 4.1% and to be associated with patient age. In contrast to this study, Ruiz Marcellan et al. [9] did not report any cases of hematoma or bleeding in 17 patients with hemorrhagic diathesis following ESWL. However, in patients with hemorrhagic diathesis, coagulation tests should be done because of the risk of hematoma occurrence, and platelet counts should be increased above 50.000/mm3. As far as we know, our case had undergone a single session of ESWL nearly 2 months previously for a left ureteral stone. Even though the risk of development of perirenal hematoma secondary to ESWL increases in chronic ITP, the absence of any urinary system symptoms in our patient after ESWL and the application of ESWL targeted to the distal ureter suggest that the bleeding was not a complication of ESWL but rather originated from thrombocytopenia due to ITP. Still, stasis and compression resulting from hydronephrosis caused by bilateral distal ureteral stones might be influential in the development of perirenal hematoma.
In conclusion, urinary system diseases can be seen in patients with bleeding diathesis, such as chronic ITP, and related hematologic test results should be carefully evaluated in the following up and treatment of these patients. In these cases, therapeutic procedures targeting urinary system abnormalities can be optimally performed after normalizing hematologic test results while continuing ITP therapy without making any change in the current treatment modalities.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download