Abstract
Purpose
This study aimed to determine whether symptoms of urinary urgency increase according to the severity of stress urinary incontinence (SUI). For this purpose, we recruited women with symptoms of mixed as well as pure SUI and compared the clinical characteristics of each subgroup.
Materials and Methods
A total of 241 female patients who were diagnosed with SUI and mixed urinary incontinence (MUI) were analyzed retrospectively. Patients with only SUI were categorized as group 1. Patients with MUI were categorized as group 2. Clinical and urodynamic differences between the 2 groups were compared.
Results
The proportion of Stamey grade was significantly different between the 2 groups: grade 1 SUI was higher in group 1, but grades 2 and 3 SUI were higher in group 2. The incidence of urgency was proportional to the degree of Stamey grade (23.5% in grade 1, 36.9% in grade II, and 60.0% in grade III). In the urodynamic study, the presence of detrusor overactivity was significantly higher in group 2 than in group 1 (25.9% vs. 49.4%). Other clinical parameters were also significantly different between the 2 clinical groups: Q-tip angle (group 1: 42.1°, group 2: 28.6°, p<0.05), maximal urethral closure pressure (group 1: 54.7 cmH2O, group 2: 44.1 cmH2O, p<0.05), maximal bladder capacity (group 1: 356.3 ml, group 2: 282.0 ml, p<0.05), and bladder volume at first desire (group 1: 144.6 ml, group 2: 123.2 ml, p<0.05).
Mixed urinary incontinence (MUI) is a troublesome condition for patients and incontinence specialists because for treatment to be successful, both the stress and the urge components of the incontinence need to respond to therapy. The International Continence Society's standardized nomenclature defines mixed urinary incontinence as "the complaint of involuntary leakage associated with urgency and also with exertion, effort, sneezing or coughing." [1]. The most appropriate definition for mixed incontinence is not known. From a pragmatic standpoint, patients with MUI and their clinicians want information about the chance of a favorable outcome following their primary incontinence treatment. The clinical consequences of not understanding the role of the stress and urge components in MUI include the persistence of urge incontinence after stress urinary incontinence (SUI) surgery, which the patient then perceives as surgical failure [2-4]. The urgency component in MUI may consist of either detrusor instability, urethral relaxation, or an uninhibited premature micturition reflex [5]. Others have argued that the "urge incontinence" component of MUI appears to be different from that of urge urinary incontinence (UUI) and have suggested that urge incontinence may be overdiagnosed in patients with SUI who misinterpret their fear of leaking (because of SUI) for urge incontinence [6]. In our study, we tried to identify whether symptoms of urgency increase along with the severity of SUI symptoms. In an effort to define more precisely the specific pathophysiology of incontinence in women, we examined whether women suffering from MUI exhibit clinical and urodynamic characteristics that are distinct from those of patients with pure SUI.
Two hundred forty-one women with SUI and MUI from March 2005 to December 2008 were included in this study, and their medical records were retrospectively reviewed. Patients with diabetes mellitus, neurologic disease, prior urologic surgery, and urethral abnormalities were excluded. Of the total, 164 patients (68%) had SUI symptoms only, and 77 (32%) had MUI symptoms. Urgency was defined as an average of 1 episode per day on a 3-day voiding diary. Patients with SUI only were defined as group 1, and those with MUI were defined as group 2.
History taking, physical examination, urinalysis, quantitative urine culture, Q-tip test, frequency volume chart, uroflow study, postvoiding residual urine measurement, Valsalva leak point pressure (VLPP), and urodynamic study that included maximal urethral closure pressure (MUCP) were performed on all patients.
Level of incontinence symptoms were categorized into grade I, II, and III according to the Stamey grade. The degree of cystocele was categorized into grade I-V. Urethral hypermobility was defined as more than 30° by a Q-tip test. The cutoff value of VLPP, in which endogenous sphincter dysfunction is suggested by urodynamic study, was defined as less than 60 cmH2O. Detrusor overactivity (DO) was defined as involuntary detrusor contraction of more than 15 cmH2O during filling cystometry with a speed of saline infusion of 30 ml/min.
The Bristol Female Lower Urinary Tract Symptom (BFLUTS-F2) questionnaire was used to evaluate the symptoms of urinary urgency. The grade of urinary urgency symptoms was expressed from 0 to 4, and higher points represented more severe symptoms. In our study, urgency symptoms were not only urgency but also urge incontinence.
Baseline clinical characteristics, such as age, body mass index (BMI), parity, duration of urinary incontinence symptoms, previous pelvic surgery, and Stamey symptom grade were compared between the 2 groups. Degree of urethral hypermobility and cystocele degree from physical examination, residual urine volume, maximal bladder capacity (MBC), bladder volume at first desire, VLPP, and MUCP, Pdetmax, and presence of DO from the urodynamic study were also compared. Statistical analysis used SPSS ver. 12.0 (SPSS, Inc., Chicago, IL, USA) and examined continuous variables by use of the independent t-test and non-continuous variables by use of the chi-square test in comparisons of the clinical characteristics and results of the 2 groups. A p-value of less than 0.05 was regarded as achieving statistical significance.
The mean age of the patients was 53.9 years (range, 35-81 years), the average parity was 2.5 (range, 0-8), average BMI was 24.7 kg/m2 (range, 17.2-34.3 kg/m2), and the average duration of symptoms was 71 months (range, 1-360 months).
Comparing baseline characteristics, age and a positive history of previous pelvic surgery were significantly higher in group 2 than in group 1 (56 vs. 53 years old for age, p<0.05; 57.1% vs. 44.5% for previous pelvic surgery, p<0.05). In our study, previous pelvic surgery included hysterectomy, myomectomy, oophorectomy, and cesarean section.
Severe degrees of cystocele (II-IV) were more frequently observed in group 2 than in group 1 (grade 0=69.5%, I=20.1%, II=7.9%, III=1.2%, IV=1.2% in group 1, vs. grade 0=57.1%, I=15.6%, II=11.7%, III=9.1%, IV=6.5% in group 2, p<0.05). The degree of urethral hypermobility was greater for group 1 than for group 2 (42.1° vs. 28.6°, p<0.001) (Table 1).
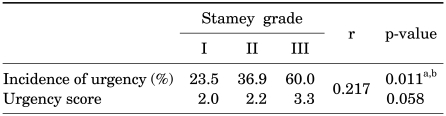
The proportion of Stamey grades differed between the 2 groups. Grade I symptoms were more frequently noted in group 1 than in group 2 (45.7% vs. 29.9%). However, grade II or III symptoms were seen more frequently in group 2 than in group 1 (53% vs. 66.2% for grade II; 1.2% vs. 3.9% for grade III) (p<0.05). Also, a positive linear association (6.440) was noted between Stamey grade and incidence of urgency in the linear by linear association test. That is, the incidence of urgency was proportional to the degree of Stamey grade (23.5% in grade 1, 36.9% in grade II, and 60.0% in grade III, p<0.05) (Table 2).
MUCP, MBC, and bladder volume at first desire were higher in group 1 than in group 2 (54.7 cmH2O vs. 44.1 cmH2O for MUCP, p<0.001; 356.3 ml vs. 282.0 ml for MBC, p<0.001; 144.6 ml vs. 123.2 ml for bladder volume at first desire, p<0.05, respectively). DO was more frequently observed in group 2 than in group 1 (49.4% vs. 25.9%, p<0.001) (Table 1).
Logistic regression analysis failed to identify any significant risk factors influencing the urgency symptoms accompanied by SUI among the clinical and urodynamic parameters.
The urgency score measured by the BFLUTS became higher as the Stamey symptom grade advanced (2.0 in I, 2.2 in II, and 3.3 in III), but not significantly so (r=0.217, p=0.058) (Table 2).
In this study, we compared 2 groups of SUI patients, those with and without urge incontinence, to determine whether any clinical or urodynamic data could identify differences between them. According to the argument suggested by Chou et al, the "urge incontinence" component of MUI appears to differ from that of UUI, and they suggested that urge incontinence may be overdiagnosed in patients with SUI who misinterpret their fear of leaking for their urge incontinence [6]. In our study, we also tried to identify whether the symptoms of urgency increased along with the severity of SUI symptoms. In other words, we suspected that the urgency symptoms accompanied by SUI may represent overexpression of the patient's premature voiding by her will to avoid stress-induced urine leakage, although not all. In an effort to define more precisely the specific pathophysiology of incontinence in women, we examined whether women suffering from MUI exhibited clinical or urodynamic characteristics that were distinct from those of patients with pure SUI.
Our study showed that the incidence of urgency was proportional to the degree of Stamey grade and that women with an MUI component had more severe SUI symptoms than did those with pure SUI. These results suggest that the urgency symptoms in SUI were not independent conditions. After reviewing epidemiologic and clinical evidence, Minassian et al also suggested that stress and urge urinary incontinence (UI) are pathophysiologically linked, consistent with the Integral Theory, which posits that bladder control problems, including stress and urge UI, are consequences of abnormal connective tissue resulting from an insult to the supportive pelvic floor support structures [7].
Resolution of urgency symptoms after surgery for SUI has been reported to be fair, with percentages of 60.2%, 54.2%, 54%, 63.6%, and 59% [8-12]. These results suggest that in patients with MUI, SUI may affect the development of urinary urgency symptoms as evidenced by the resolution of urgency following the surgery. Mahony et al reported two urethro-detrusor reflexes that increased the excitability of the micturition reflex as urine flowed across the urethral mucosa, modeling the clinical relationship between SUI and DO [13]. Hindmarsh et al proposed that urethral overactivity is often associated with unstable bladder contractions and suggested that bladder overactivity may originate from stimuli in the bladder outlet [14]. Also, Jung et al demonstrated that fluid passing through the urethra could promote detrusor activity [15].
Even with current bladder neck surgery or surgery that places tension on the central urethra, which were conducted before the introduction of the theory of tension-free surgery, not only the treatment of SUI but also urgency symptoms were reported to improve [16,17]. Also, fairly high numbers of patients have been reported to show improvement in both the treatment of SUI and urinary symptoms with the current tension-free surgery methods [18]. This illustrates the connection between the two diseases of urinary urgency and SUI, because such surgery stabilizes the urethra statically or dynamically, thus showing that the urethra is contributing in some part. Our study showed that the Q-tip test, which assesses the stability of the urethra, has significant meaning between the SUI group with no urinary urgency and the group with urinary urgency. Also, MUCP was verified as a factor with significant meaning between the 2 groups. Ku et al reported that MUCP is one of the independent prognostic factors that maintains the urinary urgency of urinary incontinence patients after the tension-free vaginal tape (TVT) procedure [19].
Reports on how duloxetine, which is being researched as a remedy for SUI, increases urethral resistance and bladder volume at the same time show that there is an association between urethral pressure and bladder volume [17,20]. Our study also confirmed that the MBC and bladder volume at first desire differed significantly between the 2 groups. Others also reported that urinary urgency symptoms and unstable bladder contractions occur as urethral pressure decreases [21,22].
In our study, age, previous pelvic surgery, and degree of cystocele were shown to be significant factors between the 2 groups. It could be supposed that with increasing age, previous pelvic surgery, or pelvic organ prolapse, some changes may occur in the bladder and pelvic tissue or detrusor, and that as a result, urinary urgency may have developed. In Nguyen and Bhatia's report, 56.7% of patients with pelvic organ prolapse symptoms complained of symptoms of urinary urgency, with pelvic organ prolapse being the factor having a connection with urinary urgency [23].
The presence of DO in MUI is controversial, because the presence of DO may affect the physician's decision for surgery as well as the surgical outcomes. Interestingly, many women with clinically defined MUI do not demonstrate DO during urodynamic studies [24]. Consequently, the relationship between DO and clinical symptoms is often conflicting and has not been fully delineated. If the rate of positive DO was higher in patients with MUI, then we can easily conclude that the cause of urgency symptoms in MUI was independent of SUI symptoms. However, in real practice, only about 50% at most of women with MUI exhibited DO during urodynamics, which suggests that the urgency symptoms in MUI were closely linked with each other. In a preoperative urodynamic study of women with MUI, Stoffel et al reported that 42% of MUI patients had preoperative DO [25]. In our study, it was observed that 49.4% of MUI patients exhibited DO, which is similar to the report of Stoffel et al, but lower than that of Lewis et al, who insisted that 56% of SUI patients showed DO [26]. On the other hand, Digesu et al reported 11% of MUI patients to have positive DO [27].
In a report by Chou et al, the rate of DO occurrence was less than in the patients with symptoms of urge incontinence in the MUI patient group, and he explained this finding as "over diagnosis," which shows urinary urgency to prevent it in the early stage because patients with severe SUI are more aware of urine flows [6]. Our results suggested that the urgency in MUI was correlated with the severity of SUI symptoms, but that the component of urgency may exist independently of the SUI symptoms.
In our study, it may be controvertible to use the Stamey symptom grade in MUI, because patients with severe MUI symptoms might misunderstand urge incontinence as SUI. However, we thought that the Stamey grade was a meaningful assessment scale from the point of view of the doctor more than the patient. A more detailed classification between SUI and urge incontinence should be considered in patients with severe MUI, and more systemic and objective consideration that could analyze SUI symptoms will be required.
In conclusion, the more serious the symptoms of SUI, the higher the incidence of accompanying urinary urgency. MUI may represent a more advanced state of SUI. According to the considerable rates of DO shown in our results, it is also possible that there may be a unique underlying cause that motivates symptoms of mixed UI that is distinct from the factors that stimulate urge UI induced by SUI.
References
1. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002; 21:167–178. PMID: 11857671.

2. Elkadry EA, Kenton KS, FitzGerald MP, Shott S, Brubaker L. Patient-selected goals: a new perspective on surgical outcome. Am J Obstet Gynecol. 2003; 189:1551–1557. PMID: 14710061.

3. Hullfish KL, Bovbjerg VE, Gibson J, Steers WD. Patient-centered goals for pelvic floor dysfunction surgery: what is success, and is it achieved? Am J Obstet Gynecol. 2002; 187:88–92. PMID: 12114893.

4. Mahajan ST, Elkadry EA, Kenton KS, Shott S, Brubaker L. Patient-centered surgical outcomes: the impact of goal achievement and urge incontinence on patient satisfaction one year after surgery. Am J Obstet Gynecol. 2006; 194:722–728. PMID: 16522404.

5. Rezapour M, Ulmsten U. Tension-free vaginal tape (TVT) in women with mixed urinary incontinence--a long-term follow-up. Int Urogynecol J Pelvic Floor Dysfunct. 2001; 12(Suppl 2):S15–S18. PMID: 11450974.
6. Chou EC, Blaivas JG, Chou LW, Flisser AJ, Panagopoulos G. Urodynamic characteristics of mixed urinary incontinence and idiopathic urge urinary incontinence. Neurourol Urodyn. 2008; 27:376–378. PMID: 18314874.

7. Minassian VA, Stewart WF, Hirsch AG. Why do stress and urge incontinence co-occur much more often than expected? Int Urogynecol J Pelvic Floor Dysfunct. 2008; 19:1429–1440. PMID: 18528608.

8. Matteo B, Shahar M, Rodney AA. Resolution of urge symptoms following sling procedure. J Urol. 2002; 167:78A. abstract 311.
9. Fulford SC, Flynn R, Barrington J, Appanna T, Stephenson TP. An assessment of the surgical outcome and urodynamic effects of the pubovaginal sling for stress incontinence and the associated urge syndrome. J Urol. 1999; 162:135–137. PMID: 10379756.

10. DeMarco E, Heritz DM, Blaivas JG. Can we predict which patients will have urge incontinence following pubovaginal sling? J Urol. 1994; 151(Suppl):420A. abstract 770. PMID: 8283542.
11. Fulford SC, Bedwani J, Stephenson TP, Cardiff W. An investigation into the relationship of the urge syndrome and genuine stress urinary incontinence. J Urol. 1997; 157(Suppl):458A. abstract 1792.
12. Meyhoff HH, Walter S, Gerstenberg TC, Olesen KP, Nordling J, Pedersen PH, et al. Incontinence surgery in female motor urge incontinence. Acta Obstet Gynecol Scand. 1983; 62:365–368. PMID: 6637411.

13. Mahony DT, Laferte RO, Blais DJ. Integral storage and voiding reflexes. Neurophysiologic concept of continence and micturition. Urology. 1977; 9:95–106. PMID: 556658.
14. Hindmarsh JR, Gosling PT, Deane AM. Bladder instability. Is the primary defect in the urethra? Br J Urol. 1983; 55:648–651. PMID: 6652433.

15. Jung SY, Fraser MO, Ozawa H, Yokoyama O, Yoshiyama M, De Groat WC, et al. Urethral afferent nerve activity affects the micturition reflex: implication for the relationship between stress incontinence and detrusor instability. J Urol. 1999; 162:204–212. PMID: 10379788.

16. Kobashi KC, Govier F. The completely dry rate: a critical re-evaluation of the outcomes of slings. Neurourol Urodyn. 2005; 24:602–605. PMID: 16177999.

17. Ryu BS, Chung H, Lee JB. The change of urgency and effect on patient satisfaction after sling operations for stress urinary incontinence. Korean J Urol. 2004; 45:433–437.
18. Bourrat M, Armand C, Seffert P, Tostain J. Complications and medium-term functional results of TVT in stress urinary incontinence. Prog Urol. 2003; 13:1358–1364. PMID: 15000314.
19. Ku JH, Shin JW, Son H, Oh SJ, Kim SW, Paick JS. Predictive factors for persistent urgency or urge incontinence after tension-free vaginal tape procedure in mixed urinary incontinence. Korean J Urol. 2004; 45:330–336.
20. Theofrastous JP, Cundiff GW, Harris RL, Bump RC. The effect of vesical volume on Valsalva leak-point pressures in women with genuine stress urinary incontinence. Obstet Gynecol. 1996; 87:711–714. PMID: 8677072.

21. Petros PE, Ulmsten U. Bladder instability in women: a premature activation of the micturition reflex. Neurourol Urodyn. 1993; 12:235–239. PMID: 8330046.
22. Webster GD, Sihelnik SA, Stone AR. Female urinary incontinence: the incidence, identification, and characteristics of detrusor instability. Neurourol Urodyn. 1984; 3:235–242.
23. Nguyen JK, Bhatia NN. Resolution of motor urge incontinence after surgical repair of pelvic organ prolapse. J Urol. 2001; 166:2263–2266. PMID: 11696748.

25. Stoffel JT, Smith JJ, Crivellaro S, Bresette JF. Mixed incontinence: does preoperative urodynamic detrusor overactivity affect postoperative quality of life after pubovaginal sling? Int Braz J Urol. 2008; 34:765–771. PMID: 19111082.

26. Lewis JB, Ng AV, O'Connor RC, Guralnick ML. Are there differences between women with urge predominant and stress predominant mixed urinary incontinence? Neurourol Urodyn. 2007; 26:204–207. PMID: 17078089.

27. Digesu GA, Salvatore S, Fernando R, Khullar V. Mixed urinary symptoms: what are the urodynamic findings? Neurourol Urodyn. 2008; 27:372–375. PMID: 17943988.

TABLE 1
Characteristics of the SUI and MUI groups
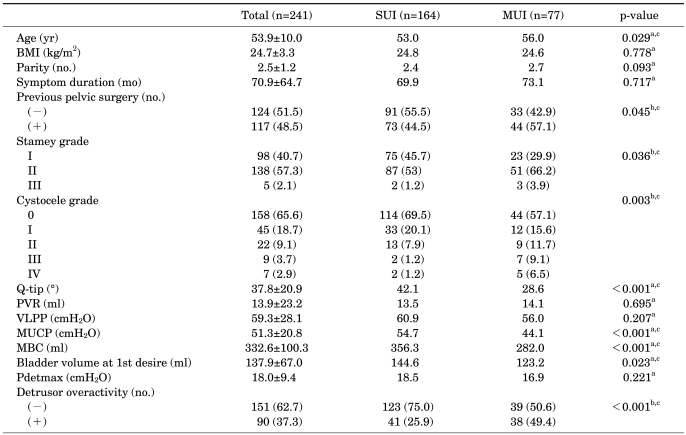
SUI: stress urinary incontinence, MUI: mixed urinary incontinence, BMI: body mass index, PVR: postvoid residual, VLPP: Valsalva leak point pressure, MUCP: maximal urethral closing pressure, MBC: maximum bladder capacity, a: independent t-test, b: chi-square test, c: statistically significant (p<0.05)




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download