Abstract
Purpose
The purpose of this study was to develop and evaluate psychometric properties of the instrument, Resuscitation Self-Efficacy Scale for nurses.
Methods
This was a methodological study for instrument development and psychometric testing. The initial item pool derived from literature review and experts resulted in 30 items linked to resuscitation self-efficacy. A convenience sample of 509 Korean nurses from eleven academic teaching hospitals participated in a survey to examine psychometric properties of the scale. To examine construct validity, exploratory factor analysis and known-group comparison were used. Cronbach's coefficient alpha was used to determine the scale's internal consistency reliability.
Results
The final scale included 17 items with four-component structure termed 'Recognition', 'Debriefing and recording', 'Responding and rescuing', and 'Reporting'. These four factors accounted for 57.5% of the variance. Each subscale and the total scale demonstrated satisfactory internal consistency: .82; .88; .87; .83; and .91 respectively. Experienced nurses reported significantly higher self-efficacy mean scores in both total and subscales compared to new graduate nurses.
Effective and high-quality resuscitation performance is essential for nurses who are usually the first responders in in-hospital clinical emergencies. It requires a set of coordinated actions represented by the links in the Chain of Survival, and includes immediate recognition and activation, early cardiopulmonary resuscitation (CPR), rapid defibrillation, effective advanced life support and integrated post-cardiac arrest care (Travers et al., 2010). However, nurses are not delivering high-quality resuscitation skills in actual clinical settings (Abella et al., 2005) or simulated environment (Kim, Lee, Lee, & Kim, 2012). Under preparedness of nurses responding to a resuscitation event may result in an extended time to intervention and consequently a decrease in patients' chance of survival (Moretti et al., 2007). Therefore, effective resuscitation training is needed to ensure high-quality resuscitation performance.
According to Bandura (1997), self-efficacy refers to a person's sense of confidence in his or her ability to perform a particular behavior in a variety of circumstances, and self-efficacy beliefs are constructed from enactive mastery experiences, vicarious experiences, verbal persuasion, and physiological and affective states. Resuscitation self-efficacy is defined as a judgment of perceived capability to organize and execute the process of care during resuscitation (Maibach, Schieber, & Carroll, 1996). It is also believed to be an important factor in areas of education for health professions, including resuscitation training (Maibach et al.; Turner, Lukkassen, Bakker, Draaisma, & ten Cate, 2009). Turner et al. demonstrated that self-efficacy was moderately correlated with the quality of global performance of healthcare providers on a simulation, clinicians who are knowledgeable and skilled in resuscitation techniques may fail to apply them successfully unless they have an adequately strong self-efficacy (Maibach et al.).
One of the major effects of training is developing confidence in self-performance (Cant & Cooper, 2010). However, there has been relatively little research on the effect of resuscitation training on nurses' self-efficacy (Carlo et al., 2009; Gordon & Buckley, 2009; Roh, Lee, Chung, & Park, 2011; van Schaik, Plant, Diane, Tsang, & O'Sullivan, 2011), and a possible reason is the lack of a simple measurement instrument. Furthermore in the provision of healthcare, inaccurate calibration of self-efficacy may lead to adverse patient outcomes (Stump, Husman, & Brem, 2012). Therefore, it is important to evaluate resuscitation self-efficacy to foster assessment of current practice and promote the implementation of educational interventions through identification of areas of low characteristic values to be targeted by educational interventions.
Nurses who are often the first responders in the emergency situations require their sense of confidence to be measured in a reliable and valid way. Measuring self-efficacy requires the development of a situation- and population-specific instrument (May & Limandri, 2004) including either single-faceted resuscitation tasks (Carlo et al., 2009; Turner, van de Leemput, Draaisma, Oosterveld, & ten Cate, 2008) or multi-faceted tasks (Gordon & Buckley, 2009). But there are few published instruments that measure nurses' self-efficacy in resuscitation task (Gordon & Buckley; Turner et al.). However in a Gordon and Buckley's study, although questions were related to nurse-specific resuscitation tasks, items related to post-cardiac arrest care were lacking. Turner et al. who developed the 4-item Visual Analogue Scale to measure self-efficacy only had three pediatric resuscitation-specific tasks; cardiac massage, bag and mask ventilation, and insertion of an intraosseous device which are generally performed by doctors. In addition, Cronbach's alpha for the scale was .59 casting doubt on its reliability in use for hospital nurses. Another limitation is that self-efficacy scales have not been thoroughly validated before implementation (Carlo et al.) or have been adapted from the resident survey to account for nurse-specific resuscitation tasks and skills (van Schaik et al., 2011). Therefore, there is a need to develop an easy-to-use and clinically adequate resuscitation self-efficacy measure that includes all above multitude of nurse-specific resuscitation tasks in contrast to a physician focused one using a systematic way of scale development to support its reliability and validity.
In the hospital settings nurses are often the first responders in the emergency situations that require their sense of confidence in his or her ability to perform optimal resuscitation skills. Therefore, there is need to assess nurses' self-efficacy in a reliable and valid way. But no instrument was found that is applicable to the nurses involved in the situations that require resuscitation. Through accurate and regular appraisal of self-efficacy in multi-faceted resuscitation tasks, such a tool could serve as an instrument for assessment and evaluation. The purpose of this study was to develop and evaluate the psychometric properties of an instrument to appraise nurses' resuscitation self-efficacy.
This was a methodological study to determine the psychometric properties of the nurses' resuscitation self-efficacy and to provide evidence for its construct validity.
The authors reviewed the literature and questionnaires previously published regarding nurses' resuscitation self-efficacy. Thematic analysis of the literature review was performed to derive the construct for the instrument. In this study, consideration was given to the implications of Bandura's theoretical concept which states that self-efficacy instruments should measure a judgment of perceived capability ("I can do") for carrying out specific activities (Bandura, 1997). A few principal articles (Odell, Victor, & Oliver, 2009; Smith, 2010) and existing instruments (Gordon & Buckley, 2009; Hicks, Bandiera, & Denny, 2008; Turner et al., 2008) served as a matrix for the items on the questionnaire. The conceptual framework of nurses' resuscitation self-efficacy was developed based on the extensive literature review (Figure 1). It includes four dimensions corresponding to the three core attributes of nurses' resuscitation self-efficacy.
Initially, the English version of the Resuscitation Self-Efficacy Scale (RSES) with 33 items was developed based on empirical referents or indicators identified from the literature. To derive the initial items, three original instruments were carefully reviewed: 15-item Evaluation Form for Early Interventions in Acute Care Nursing Simulation Workshop (Gordon & Buckley, 2009), 16-item Team Training Needs Assessment Survey Tool (Hicks et al., 2008), and 4-item Visual Analogue Scale to measure self-efficacy (Turner et al., 2008). Among the 33-item preliminary scale, 18 items were derived from the above three instruments, and 15 items (patient monitoring, other nurse-specific technical skills, equipment preparation, post-resuscitation care, documentation, and debriefing) were newly added based on the extensive literature review to measure nurse-specific resuscitation self-efficacy.
The initial draft of the English version of the RSES was revised based on five experts' comments about the questionnaire length, item repetition, and clarity. A content validity index (CVI) was established with the assistance of two faculty members of nursing schools in the United States and one faculty member of a nursing school and two physicians in Korea who had expertise in critical or emergency care. Overall CVI scores for the scale ranged from .85 to .90. Finally, this process reduced the scale from 33 to 30 items. The English version of 30-item RSES was back-translated into Korean by the authors. In addition, content validity of the Korean version of the RSES was retested with seven volunteer practicing nurses. Three items were further clarified in terms of meaning based on the nurses' comments.
Demographic characteristics included gender, age, total work duration, workplace specialty, and highest education degree. Nurses' perceived resuscitation self-efficacy was measured using the Korean version of the initial instrument. It consists of 30 items and participants are asked to respond on a 5-point Likert-type scale ranging from 1 (least confident) to 5 (very confident).
The total sample size was estimated based on the suggestion that there be at least 10 to 15 subjects per initial item for factor analysis, preferably aiming for a sample size that fits Comrey and Lee's very good (N=500) category to assess the adequacy of the total sample size (Pett, Lackey, & Sullivan, 2003). The sample was 540 hospital nurses who agreed to participate in this research and who worked in non critical care areas of the hospitals. The distribution of 540 structured questionnaires to the 11 hospitals resulted in 531 returned surveys, accounting for a response rate of 98.3%. For the final analysis, 509 questionnaires were used after excluding 22 due to incomplete data.
The study was approved by the Institutional Review Board (IRB) of the College of Nursing, Yonsei University. Informed consent was obtained from each participant who volunteered. Respondent anonymity was maintained throughout the data collection and analysis.
The authors contacted and requested the nursing department/division in each of the 25 University affiliated academic teaching hospitals in Seoul, Korea to participate in the research. Eleven of the 25 university affiliated academic teaching hospitals agreed to participate in the study (44%). A self-administered questionnaire consisting of the 30-item RSES and a set of demographic questions was sent via mail to the 11 hospitals with a letter describing the study. Using a convenience sampling method, eligible participants were approached by a staff nurse in the nursing departments of the 11 hospitals, who distributed and collected the questionnaires as a research assistant. The data collection period lasted from April 11 to May 20, 2011.
Data were analyzed using SPSS version 18.0 program (SPSS Inc, Chicago, IL) and included descriptive statistics for demographic characteristics, CVI, exploratory factor analysis to assess validity, and Cronbach's alpha coefficients to assess reliability.
An exploratory factor analysis with principal axis factoring (PAF) approach and Direct Oblimin rotation was used to explore the underlying structure and investigate the construct validity of the RSES. The reason for using Oblimin rotation was that the factors were conceptualized as interrelated aspects of self-efficacy. In the PAF solution, factors were extracted with eigen values greater than 1.0. In the extraction phase, items were used, if they had a factor loading of at least .40 (Pett et al., 2003).
For known-group analysis, comparison of the mean of RSES and its subscale scores between new graduate and experienced nurses was performed using t-test. In this study, new graduate nurses were defined as nurses with less than 12 months of clinical experience.
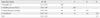
A demographic profile of the nurses is presented in Table 1. Of the nurses, 504 (99%) were women, and their ages ranged from 22 to 52 years, with a mean age of 28.8 years (SD=4.96). Experienced nurses with work duration of more than 12 months made up 84.1% of the sample. The majority of the participants either worked in a medical ward or a surgical ward (45.8%, 43.4% respectively).
The item means, standard deviations, inter-item correlation matrix, and item-total correlations were computed and examined. The item-to-total scale correlations of preliminary 30-item scale ranged from .44 to .78. After serial calculation of corrected item-total correlation coefficients, 13 items were eliminated because of redundancy or lack of homogeneity with the construct by the acceptable corrected item-total correlations ranged from .20 to .70. The remaining 17 items had corrected item-total correlation coefficients between .44 and .67.
Prior to performing the analysis, the suitability of the data for factor analysis was assessed. First, the range of inter-item correlations was from .04 to .73. Examination of the correlation matrix indicated that all items correlated ≥.30 with at least three other items in the matrix. We concluded that the correlation matrix was factorable and we could continue with the initial extraction process. Secondly, Bartlett's test of sphericity was significant (χ2 = 5825.54, p<.001), which indicated that the correlation matrix was not an identity matrix. The Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy which is an index that compares the magnitude of the observed correlations with the magnitude of the partial correlation coefficients (Pett et al., 2003) was appropriate (.93). These results suggest that a factor analysis was appropriate and could be expected to yield common factors.
The factor loadings for the rotated four-factor solution from responses to items on the RSES are presented in Table 2. Factors were interpreted and labeled based on the four main themes of nurses' role in detecting deteriorating patients (Odell et al., 2009): 'Recognition' (factor 1); 'Debriefing and recording' (factor 2); 'Responding and rescuing' (factor 3); 'Reporting' (factor 4). These four factors explained 57.5% of the total variance.
The mean resuscitation self-efficacy scores between new graduate and experienced nurses are presented in Table 3. Experienced nurses, compared to new graduate nurses, reported a significant higher mean scores for total RSES (t= -6.61, p= <.001), and for the Recognition subscale (t= -5.92, p= <.001), Debriefing and recording subscale (t= -5.53, p= <.001), Responding and rescuing subscale (t= -5.35, p= <.001), and Reporting subscale (t= -4.37, p= <.001).
Table 4 presents the descriptive statistics, between-factor correlations, and alpha coefficients for the four generated subscales of the RSES. On a 5-point scale, the mean score for total self-efficacy was 3.53±0.48. The correlations between the subscales ranged from .13 to .65. The reliability estimates presented in parentheses on the diagonal of Table 4 ranged from .82 to .88. The RSES in this study demonstrated high internal consistency with an alpha value of .91.
Resuscitation self-efficacy is defined as a judgment of perceived capability to organize and execute the process of care during resuscitation. The purpose of this RSES is to evaluate a judgment of perceived capability in resuscitation including change over time, discriminate self-efficacy level by demographic background, resuscitation training, or real code experience, and identify areas of low characteristic values to be targeted by educational intervention. The final version of the RSES consisted of 17 items on a self-administered 5-point Likert-type scale, ranging from 1 (least confident) to 5 (very confident). It has four factors, 'Recognition', 'Debriefing and recording', 'Responding and rescuing', and 'Reporting'. All items were phrased positively. Higher mean scores denote higher degrees of resuscitation self-efficacy.
In this study, a measure of nurses' resuscitation self-efficacy, the 17-item Resuscitation Self-efficacy Scale (RSES) was developed, tested and refined. The RSES has four factors, 'Recognition', 'Debriefing and recording', 'Responding and rescuing', and 'Reporting', and these four factors accounted for 57.5% of the variance. Each subscale and the total scale demonstrated satisfactory internal consistency. The RSES appears to be a scale that can provide researchers with easy-to-use assessment of nurse-specific multidimensional resuscitation self-efficacy and that yields reliable data enabling valid judgments.
The data from this study support the multidimensional conceptualization of nurse-specific resuscitation self-efficacy. Exploratory factor analysis of the 17-item scale resulted in a four-factor solution termed Recognition, Debriefing and recording, Responding and rescuing, and Reporting. The results of testing the RSES using common factor analysis support the four main themes of nurses' role in detecting deterioration in ward patients (Odell et al., 2009). In addition, these factors are similar to the scale regarding the technical and non-technical aspects of emergency response used in Gordon and Buckley (2009)'s study except for 'Debriefing and recording'. In contrast, the Visual Analogue Scale (Turner et al., 2008) was not a valid tool to discriminate the nurse-specific self-efficacy because it has mainly physician specific resuscitation tasks. Nurses play a pivotal role in performing multi-faceted tasks throughout the resuscitation process between recognition and post-cardiac arrest care. Bandura's self-efficacy theory continues to represent the predominant paradigm for measurement based on the breadth of studies reporting findings about specific self-efficacy (May & Limandri, 2004). Therefore, the RSES can be considered a valid instrument to measure nurse-specific self-efficacy with respect to either well defined resuscitation tasks or multi-faceted tasks in resuscitation.
The study results suggest that 'Recognition', 'Debriefing and recording', 'Responding and rescuing', and 'Reporting' were the important factors, and 'Recognition' was the strongest factor and explained the highest percentage of variance. Effective resuscitation requires a combination of competencies in knowledge, technical and non-technical skills (Hicks et al., 2008). Nurses' awareness of deteriorating patients on general wards has been reported as suboptimal (Fuhrmann, Lippert, Perner, Østergaard, 2008), and a systematic review demonstrated that changes in deteriorating signs are often missed or misinterpreted by nurses (Pothitakis, Ekmektzoglou, Piagkou, Karatzas, & Xanthos, 2011). Wayne et al. (2008) demonstrated that debriefing as a technique to reflect on the performance improved adherence to resuscitation guidelines in clinical settings. However, in terms of responding and rescuing, the quality of CPR technical skills frequently did not meet established guidelines during an in-hospital cardiac arrest (Abella et al., 2005), and there was also a strong consensus regarding the importance of non-technical skills in resuscitation (Hicks et al.). Self-efficacy beliefs are strong determinants and predictors of the level of accomplishment that individuals finally attain (Bandura, 1997), and clinicians who are knowledgeable and skilled may fail to apply them successfully unless they have an adequate level of self-efficacy in cognitive, affective, psychomotor and social proficiency in resuscitation tasks (Maibach et al., 1996). Therefore, when tailoring educational interventions, attention should be paid to the early recognition and management of a deteriorating patient that can lead nurses to maximize their level of self-efficacy.
For further construct validity testing, known-group comparison of participants was used, considering that nurses with experience are expected to have higher levels of self-efficacy. The known-group analysis showed that self-efficacy measured on the RSES was higher in groups of experienced nurses compared to new graduate nurses. This is a similar result where both doctors and nurses showed significantly higher self-efficacy for bag and mask ventilation and cardiac massage than medical students (Turner et al., 2008). Nurses who have real code experience reported higher self-efficacy score compared to nurses with no experience (van Schaik et al., 2011). Theoretically, this would be an expected outcome. These findings support the construct validity of the RSES.
This study had several limitations. First, participants in this study were mainly from non-critical care units of academic teaching hospitals in a metropolitan area and that can impede generalization to other nurses in other clinical areas or different type of hospitals. Therefore, further testing of the RSES is needed with nurses from various work places and hospital types to enhance the reliability. Secondly, although the researchers tried their best to fully include all possible nurse-specific resuscitation tasks from resuscitation related literature, some items that would be required in different resuscitation circumstances may have been missed. In addition, psychometric testing was limited only to Korean nurses, therefore may need further validity testing and refinement study based on cultural or systematic differences in nurses' role during resuscitation attempts across countries.
The RSES with four factors demonstrated strong psychometric properties and high internal consistency. The study results indicate that the 17-item Resuscitation Self-Efficacy Scale is a tool that yields reliable data and enables one to make valid judgments of nurses' self-efficacy in multi-faceted resuscitation tasks. Assessment of self-efficacy allows educators and hospital administrators to describe nurses' self-efficacy level in resuscitation, explore correlates or determinants of resuscitation self-efficacy, and measure changes in self-efficacy as a result of educational interventions. The RSES can foster assessment of current practice, promote the implementation of educational interventions that improve self-efficacy for nurses, and eventually contribute to the improvement of patient care. Further studies that test psychometric properties of the scale are warranted to identify additional cultural or systematic differences of nurses' role during resuscitation attempts in other countries and hospital work places.
Figures and Tables
Table 2
Factor Loadings and Total Variance Explained from the Rotated Factor Structure Matrix for the Resuscitation Self-efficacy Scale (N=509)

References
1. Abella BS, Alvarado JP, Myklebust H, Edelson DP, Barry A, O'Hearn N, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA. 2005. 293(3):305–310. http://dx.doi.org/10.1001/jama.293.3.305.
2. Bandura A. Self-efficacy: The exercise of control. 1997. New York: Freeman.
3. Cant RP, Cooper SJ. Simulation-based learning in nurse education: Systematic review. J Adv Nurs. 2010. 66(1):3–15. http://dx/doi.org/10.1111/j.1365-2648.2009.05240.x.
4. Carlo WA, Wright LL, Chomba E, McClure EM, Carlo ME, Bann CM, et al. Educational impact of the neonatal resuscitation program in low-risk delivery centers in a developing country. J Pediatr. 2009. 154:504–508. http://dx/doi.org/10.1016/j.jpeds.2008.10.005.
5. Fuhrmann L, Lippert A, Perner A, Østergaard D. Incidence, staff awareness and mortality of patients at risk on general wards. Resuscitation. 2008. 77:325–330. http://dx/doi.org/10.1016/j.resuscitation.2008.01.009.
6. Gordon CJ, Buckley T. The effect of high-fidelity simulation training on medical-surgical graduate nurses perceived ability to respond to patient clinical emergencies. J Contin Educ Nurs. 2009. 40:491–498. http://dx/doi.org/10.1016/j.resuscitation.2008.01.009.
7. Hicks CM, Bandiera GW, Denny CJ. Building a simulation-based crisis resource management course for emergency medicine, phase 1: Results from an interdisciplinary needs assessment survey. Acad Emerg Med. 2008. 15:1136–1143. http://dx/doi.org/10.1111/j.1553-2712.2008.00185.x.
8. Kim EJ, Lee KR, Lee MH, Kim JY. Nurses' cardiopulmonary resuscitation performance during the first 5 minutes in in-situ simulated cardiac arrest. J Korean Acad Nurs. 2012. 42(3):361–368. http://dx.doi.org/10.4040/jkan.2012.42.3.361.
9. Maibach EW, Schieber RA, Carroll MF. Self-efficacy in pediatric resuscitation: Implications for education and performance. Pediatrics. 1996. 97:94–99.
10. May BA, Limandri BJ. Instrument development of the Self-Efficacy Scale for abused women. Res Nurs Health. 2004. 27:208–214. http://dx/doi.org/10.1002/nur.20018.
11. Moretti MA, Cesar LA, Nusbacher A, Kern KB, Timerman S, Ramires JA. Advanced cardiac life support training improves long-term survival from in-hospital cardiac arrest. Resuscitation. 2007. 72(3):458–465. http://dx.doi.org/10.1016/j.resuscitation.2006.06.039.
12. Odell M, Victor C, Oliver D. Nurses' role in detecting deterioration in ward patients: Systematic literature review. J Adv Nurs. 2009. 65:1992–2006. http://dx/doi.org/10.1111/j.1365-2648.2009.05109.x.
13. Pett MA, Lackey NR, Sullivan JJ. Making sense of factor analysis: The use of factor analysis for instrument development in health care research. 2003. London: Sage Publications.
14. Pothitakis C, Ekmektzoglou KA, Piagkou M, Karatzas T, Xanthos T. Nursing role in monitoring during cardiopulmonary resuscitation and in the peri-arrest period: A review. Heart Lung. 2011. 40:530–544. http://dx/doi.org/10.1016/j.hrtlng.2010.11.006.
15. Roh YS, Lee WS, Chung HS, Park YM. The effects of simulation-based resuscitation training on nurses' self-efficacy and satisfaction. Nurse Educ Today. 2011. http://dx/doi.org/10.1016/j.nedt.2011.11.008.
16. Smith GB. In-hospital cardiac arrest: Is it time for an in-hospital 'chain of prevention'? Resuscitation. 2010. 81:1209–1211. http://dx/doi.org/10.1016/j.resuscitation.2010.04.017.
17. Stump GS, Husman J, Brem SK. The Nursing Student Self-Efficacy Scale: Development using item response theory. Nurs Res. 2012. 61(3):149–158. http://dx/doi.org/10.1097/NNR.0b013e318253a750.
18. Travers AH, Rea TD, Bobrow BJ, Edelson DP, Berg RA, Sayre MR, et al. Part 4: CPR overview: 2010 American Heart Association Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010. 122:18 Suppl 3. S676–S684. http://dx/doi.org/10.1161/CIRCULATIONAHA.110.970913.
19. Turner NM, Lukkassen I, Bakker N, Draaisma J, ten Cate OT. The effect of the APLS-course on self-efficacy and its relationship to behavioural decisions in paediatric resuscitation. Resuscitation. 2009. 80:913–918. http://dx/doi.org/10.1016/j.resuscitation. 2009.03.028.
20. Turner NM, van de Leemput AJ, Draaisma JM, Oosterveld P, ten Cate OT. Validity of the visual analogue scale as an instrument to measure self-efficacy in resuscitation skills. Med Educ. 2008. 42:503–511. http://dx/doi.org/doi:10.1111/j.1365-2923.2007.02950.x.
21. van Schaik SM, Plant JL, Diane S, Tsang L, O'Sullivan P. Interprofessional team training in pediatric resuscitation: A low-cost, in situ simulation program that enhances self-efficacy among participants. Clin Pediatr (Phila). 2011. 50:807–815. http://dx/doi.org/10.1177/0009922811405518.
22. Wayne DB, Didwania A, Feinglass J, Fudala MJ, Barsuk JH, McGaghie WC. Simulation-based education improves quality of care during cardiac arrest team responses at an academic teaching hospital: A case-control study. Chest. 2008. 133(1):56–61. http://dx/doi.org/10.1378/chest.07-0131.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download