Abstract
Background
Although the prevalence of pulmonary tuberculosis has progressively decreased all over the world, drug-resistant tuberculosis is major obstacle in treating tuberculosis. This study was performed to examine the current prevalence and risk factors of drug resistant tuberculosis in a single tertiary hospital in Busan, Korea.
Methods
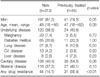
We enrolled 367 patients with active pulmonary tuberculosis on a retrospective basis who had undergone mycobacterium culture and drug sensitivity tests between January 2005 and December 2009. We analyzed all clinical and radiographic parameters to find predictors related to drug resistant tuberculosis.
Results
At least one incident of drug resistance was found in 75 (20.4%) patients. Isoniazid (18.8%) was the most frequent resistant drug, followed by rifampin (10.9%), ethambutol (7.1%), streptomycin (4.9%), and fluoroquinolone (2.7%). Resistance to second-line drugs was found in 37 (10.1%) patients. Multidrug resistance and extensively drug resistance was evident in 39 (10.6%) and 4 (1.1%) patients, respectively. Using multiple logistic regression analysis, history of previous treatment including relapse (odd ratio [OR], 11.3; 95% confidence interval [CI], 4.92~26.08; p<0.01), treatment failure (OR, 24.1; 95% CI, 5.65~102.79; p<0.01) and an age of below 46 years-old (OR, 3.8; 95% CI, 1.62~8.65; p<0.01) were found to be independent predictors of multidrug resistant tuberculosis.
Figures and Tables
Figure 1
The distribution of patients with multidrug-resistant tuberculosis according to the age group. MDR: multidrug-resistance.

References
1. World Health Organization (WHO). Global tuberculosis control: surveillance, planning, financing. WHO report 2007. 2007. Geneva, Switzerland: WHO.
2. Caminero JA, Sotgiu G, Zumla A, Migliori GB. Best drug treatment for multidrug-resistant and extensively drug-resistant tuberculosis. Lancet Infect Dis. 2010. 10:621–629.
3. Metcalfe JZ, Kim EY, Lin SY, Cattamanchi A, Oh P, Flood J, et al. Determinants of multidrug-resistant tuberculosis clusters, California, USA, 2004-2007. Emerg Infect Dis. 2010. 16:1403–1409.
4. Lougheed KE, Taylor DL, Osborne SA, Bryans JS, Buxton RS. New anti-tuberculosis agents amongst known drugs. Tuberculosis (Edinb). 2009. 89:364–370.
5. Gandhi NR, Nunn P, Dheda K, Schaaf HS, Zignol M, van Soolingen D, et al. Multidrug-resistant and extensively drug-resistant tuberculosis: a threat to global control of tuberculosis. Lancet. 2010. 375:1830–1843.
6. Velayati AA, Masjedi MR, Farnia P, Tabarsi P, Ghanavi J, Ziazarifi AH, et al. Emergence of new forms of totally drug-resistant tuberculosis bacilli: super extensively drug-resistant tuberculosis or totally drug-resistant strains in iran. Chest. 2009. 136:420–425.
7. Kim SY, Kim HJ, Kim CK, Yoon HR, Bae HG, Lee SH, et al. The recent status of multidrug- and extensively drug-resistant tuberculosis in Korea. Tuberc Respir Dis. 2010. 68:146–154.
8. Bai GH, Park YK, Choi YW, Bai JI, Kim HJ, Chang CL, et al. Trend of anti-tuberculosis drug resistance in Korea, 1994-2004. Int J Tuberc Lung Dis. 2007. 11:571–576.
9. Kim BJ, Lee IH, Lee DH, Bai GH, Kong SJ, Lee SH, et al. The current status of multidrug-resistant tuberculosis in Korea. Tuberc Respir Dis. 2006. 60:404–411.
10. Kim DW, Yoo CG, Lee CT, Kim YW, Han SK, Yoon YB, et al. Trend of prevalence of pulmonary tuberculosis among Seoul National University freshmen. Tuberc Respir Dis. 1998. 45:495–502.
11. Son CH, Yang DK, Rho MS, Jeong JS, Lee H, Lee KN, et al. Prevalence of drug-resistances in patients with pulmonary tuberculosis and its association with clinical characteristics at one tertiary rcferral hospital in Pusan, Korea. Tuberc Respir Dis. 2001. 51:416–425.
12. Kim SY, Jeong SS, Kim KW, Shin KS, Park SG, Kim AK, et al. Drug-resistant pulmonary tuberculosis in a tertiary referral hospital in Korea. Korean J Intern Med. 1999. 14:27–31.
13. Lee JH, Chang JH. Drug-resistant tuberculosis in a tertiary referral teaching hospital of Korea. Korean J Intern Med. 2001. 16:173–179.
14. Kim DK, Kim MO, Kim TH, Sohn JW, Yoon HJ, Shin DH, et al. The prevalence and risk factors of drug resistant pulmonary tuberculosis investigated at one university hospital in Seoul. Tuberc Respir Dis. 2005. 58:243–247.
15. Choi JC, Lim SY, Suh GY, Chung MP, Kim H, Kwon OJ, et al. Drug resistance rates of mycobacterium tuberculosis at a private referral center in Korea. J Korean Med Sci. 2007. 22:677–681.
16. Park YK, Park YS, Bai JY, Kim HJ, Lew WJ, Chang CH, et al. Drug resistance rate of new pulmonary tuberculosis patients treated from the private sector in 2003~2005. Tuberc Respir Dis. 2008. 64:87–94.
17. Jeon D, Shin DS, Kang HS, Sung KM, Kweon KS, Shin E, et al. Trend of multidrug and extensively drug resistant tuberculosis in a tuberculosis referral hospital, 2001~2005. Tuberc Respir Dis. 2008. 64:187–193.
18. Faustini A, Hall AJ, Perucci CA. Risk factors for multidrug resistant tuberculosis in Europe: a systematic review. Thorax. 2006. 61:158–163.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download