Abstract
The fat-forming variant of solitary fibrous tumors (SFTs) is a rare soft tissue neoplasm that was previously referred to as a lipomatous hemangiopericytoma (L-HPC). The most common affected site is deep soft tissue. Here, we present the first case, worldwide, of a fat-forming variant of SFT of the pleura. A 74-year-old man presented with left lower chest pain. Chest radiographs showed a mass-like lesion at the left lower lung field and chest computed tomography revealed a 12 cm fat-containing enhancing mass that was well-separated, lobulated and inhomogeneous. Radiology findings suggested a liposarcoma. Percutaneous needle biopsy was performed and pathological diagnosis of the mass was a fat-forming variant of SFT. Surgical resection was carried out and there has been no recurrence to date. So, a benign fat-forming variant of SFT must be considered as one of the differential diagnoses of lipomatous tumors of the pleura.
Fat-forming variant of solitary fibrous tumor (SFT) is a rare fibroblastic tumor that is composed of mature adipocytes and a hemangiopericytoma (HPC)-like area. The World Health Organization (WHO) has defined the lipomatous hemangiopericytoma (L-HPC) as a variant of a SFT in their 2002 report1.
Currently, only 41 cases of fat-forming variant of SFT or L-HPC have been reported in the English literature worldwide. In South Korea, only two cases of fat-forming variant of SFT or L-HPC have been reported. They were located in the nasal cavity and perineum2,3.
Unlike other variants of SFT, fat-forming variant of SFT occur predominantly in the deep soft tissue of the lower extremities rather than the pleura4. Fat-forming variant of SFT originating from the pleura has not been reported in the English literature to date. Therefore, the first case of fat-forming variant of SFT of the pleura is reported here2,3,5.
A 74-year-old man was presented to our department with a left lower chest pain with dyspnea. The dyspnea was intermittent over the past 10 years and the chest pain started 1 month ago. The patient was a 100 pack year ex-smoker. Auscultation of the lungs revealed an expiratory wheezing throughout both lungs, with a decreased lung sounds, tactile fremitus and vocal fremitus at the left lower lung field. The blood pressure was 130/80 mm Hg, pulse rate was 88 times per minute, respiratory rate was 22 per minute and the body temperature was 36.5℃.
Laboratory studies showed no leukocytosis (7,870/mm3); the cardiac enzyme levels were normal (CK 89 U/L, CK-MB 1.86 ng/mL, Trponin-T <0.01 ng/mL) in the peripheral blood; the blood gas studies were normal (pH 7.43 PaCO2 38 mm Hg, PaO2 92 mm Hg, HCO3 25.2 mEq/L, SaO2 97%) in the arterial blood on room air.
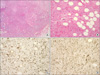
Chest radiographs showed a mass-like lesion with increased opacity at the left lower lung field (Figure 1). The chest computed tomography (CT) showed emphysematous lung parenchyma with a 12×10×5 cm fat-containing enhancing mass, which was well-seperated, lobulated and inhomogeneously enhanced (Figure 2). The radiology findings suggested a liposarcoma that originated from the pleura. The bone scan showed no bony metastatic lesions. The pulmonary function tests (PFT) showed an obstructive ventilatory disorder without reversibility. The forced expiratory volume at 1 second (FEV1) before a bronchodilator was 50% of the normal predictive value (1.2 L) and the FEV1 after a bronchodilator was 54% of the normal predictive value (1.3 L). forced expiratory volume in 1 second/forced vital capacity (FEV1/FVC) after a bronchodilator was 41%, which suggested an obstructive ventilatory disorder.
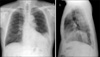
Because the radiology findings suggested a liposarcoma, a percutaneous needle biopsy was performed. Pathologic findings suggested a mesenchymal neoplasm that had spindle cells, mature fat components, and a collagenous stroma (Figure 3A, B). The immunohistochemistry staining was positive for CD34, CD99 and negative for S-100 and smooth muscle actin. The Ki-67 proliferative index was not increased, and this suggested a benign fat-forming variant of SFT rather than a malignant liposarcoma (Figure 3C, D).
The patient underwent surgical resection of the tumor. At the surgery, the tumor was found to originate from the pleura and was not attached to adjacent organs. The tumor was completely removed. The pathology confirmed that the tumor was a fat-forming variant of a SFT. After the surgery, the patient had regular follow up with chest X-ray and CT scans. There is no evidence of recurrence and the chest pain resolved. In addition, the patient was diagnosed with chronic obstructive pulmonary disease and is being treated with inhaled bronchodilators for the dyspnea which is now well controlled.
Fat-forming variant of SFT is a rare soft tissue tumor histologically characterized by a hemangiopericytomatous vasculature with mature adipocytes1. Nielsen et al. reported three tumors, composed of HPCs and adipose tissues in 1995 and referred to them as L-HPC for the first time. However, Guillou et al. reported that the L-HPC shared a similar clinical course, pathological features and immunohistochemical staining of the SFT except for the mature adipocytes. Therefore, the L-HPC was regarded as a subgroup of SFT6,7. In addition, the L-HPC was classified as a variant of the SFT by the newly established WHO classification of soft-tissue tumors (Table 1)1.
Only 41 cases of L-HPCs or fat-forming variants of SFTs have been reported in the English literature worldwide to date2,3,5-9. Among the 41 cases, the age of the patients ranged from 27 to 75 years (average 50 years). These lesions appear to occur mostly in middle-aged adult patients with no gender predilection. The fat-forming variant of SFTs has a wide anatomical distribution. However, the most common site affected has been the deep soft tissue (25 cases). Other sites have included the retroperitoneum (4 cases), mediastinum (3 cases), orbit (2 cases), nasal sinus (2 cases), larynx (1 case), thyroid (1 case), lungs (1 case), epicardium (1 case) and perineum (1 case)8,9.
In South Korea, one case of L-HPC and one case of a fat-forming variant of a SFT have been reported2,3. The first case was reported in 2001 as a L-HPC of the nasal cavity2. The second case was reported in 2009 as a fat-forming variant of a SFT of the perineum3. This is the third report of a fat-forming variant of a SFT and the first report of pleural involvement, worldwide.
SFTs originate from submesothelial mesenchymal tissue. Most SFTs grow slowly and become apparent during the fourth to sixth decades of life. They have a benign course unlike mesotheliomas and have no reported associations with genetics, smoking, exposure to asbestosis or other environmental factors. There is no gender predilection for these lesion9,10. Most SFTs develop at the pleura and a few SFTs occur at other sites such as peritoneum, lungs, mediastinum, epicardium and nasal sinuses. SFTs of the pleura are rare and reported at a rate of 2.8 persons per 100,000 hospitalized patients and account for fewer than 5% of all pleural tumors. About 800 cases of SFTs have been reported in the literature'. Malignant SFTs develop clinical symptoms in more than 75% of cases; however benign SFTs develop symptoms only in 54% to 67% of cases. The symptoms are mostly nonspecific such as cough, chest pain, and dyspnea. Some of the patients complained paraneoplastic symptoms such as arthralgia, clubbing of the fingers and hypoglycemia10.
SFTs are diagnosed when HPC-like lesions are noted with typical immunohistochemical staining. HPC-like lesions are nonspecific multiple branching anastamosing small and large vascular channels characterized by a stag-horn appearance with fibroblast-like cells and connective tissue. In addition, the fat-forming variant of a SFT is characterized by a HPC-like lesion with scattered mature adipose tissue8. The fat-forming variant of a SFT is negative for keratin, S-100 and positive for vimentin, CD34. However, most liposarcomas differ in that they are negative for CD34 and positive for S-100. CD34 is a marker for normal epithelium and vascular neoplasm. CD34 is positive for primitive mesenchymal stromal tumors and other mesenchymal tumors11.
The case reported here had pathology findings that suggested a mesenchymal tumor with spindle cells, collagenous stroma and mature adipocytes, which were positive for CD34, CD99 and negative for S-100 and smooth muscle actin. The patient was diagnosed with a fat-forming variant of a SFT. The treatment for a fat-forming variant of a SFT is a surgical resection; most cases have a benign course. Only one patient out of 41 cases was reported to have a malignant tumor with recurrence12.
Figures and Tables
Figure 2
Chest CT scans reveal large inhomogeneous fat-containing mass in the left lower hemithorax with a mild enhancing soft tissue density portion. CT: computed tomography.
Figure 3
Percutaneous needle aspiration biopsy shows a mesenchymal neoplasm with spindle cells, a mature fat component and collagenous stroma suggestive of a solitary fibrous tumor, fat-containing variant (hematoxylin-eosin, original magnification ×100 (A), ×200 (B)). Immunostains show positive results for vimentin (C) and CD34 (D) (all original magnification, ×200).
References
1. Fletcher CD. The evolving classification of soft tissue tumours: an update based on the new WHO classification. Histopathology. 2006. 48:3–12.
2. Lee JR, Kim JS, Lee CH, Sohn KR. A case of lipomatous hemangiopericytoma of the nasal cavity. Korean J Otolaryngol-Head Neck Surg. 2001. 44:893–896.
3. Kim MY, Rha SE, Oh SN, Lee YJ, Byun JY, Jung CK, et al. Case report. Lipomatous haemangiopericytoma (fat-forming solitary fibrous tumour) involving the perineum: CT and MRI findings and pathological correlation. Br J Radiol. 2009. 82:e23–e26.
4. Nielsen GP, Dickersin GR, Provenzal JM, Rosenberg AE. Lipomatous hemangiopericytoma. A histologic, ultrastructural and immunohistochemical study of a unique variant of hemangiopericytoma. Am J Surg Pathol. 1995. 19:748–756.
5. Liu X, Zhang HY, Bu H, Meng GZ, Zhang Z, Ke Q. Fat-forming variant of solitary fibrous tumor of the mediastinum. Chin Med J (Engl). 2007. 120:1029–1032.
6. Guillou L, Gebhard S, Coindre JM. Lipomatous hemangiopericytoma: a fat-containing variant of solitary fibrous tumor? Clinicopathologic, immunohistochemical, and ultrastructural analysis of a series in favor of a unifying concept. Hum Pathol. 2000. 31:1108–1115.
7. Gengler C, Guillou L. Solitary fibrous tumour and haemangiopericytoma: evolution of a concept. Histopathology. 2006. 48:63–74.
8. Cameselle-Teijeiro J, Manuel Lopes J, Villanueva JP, Gil-Gil P, Sobrinho-Simões M. Lipomatous haemangiopericytoma (adipocytic variant of solitary fibrous tumour) of the thyroid. Histopathology. 2003. 43:406–408.
9. Pitchamuthu H, Gonzalez P, Kyle P, Roberts F. Fat-forming variant of solitary fibrous tumour of the orbit: the entity previously known as lipomatous haemangiopericytoma. Eye (Lond). 2009. 23:1479–1481.
10. Robinson LA. Solitary fibrous tumor of the pleura. Cancer Control. 2006. 13:264–269.
11. van de Rijn M, Lombard CM, Rouse RV. Expression of CD34 by solitary fibrous tumors of the pleura, mediastinum, and lung. Am J Surg Pathol. 1994. 18:814–820.
12. Theunissen PH, Ariëns AT, Pannebakker MA, Blaauw G. Late recurrence of a hemangiopericytoma with lipomatous components. Pathologe. 1990. 11:346–349.
13. Folpe AL, Devaney K, Weiss SW. Lipomatous hemangiopericytoma: a rare variant of hemangiopericytoma that may be confused with liposarcoma. Am J Surg Pathol. 1999. 23:1201–1207.
14. Ceballos KM, Munk PL, Masri BA, O'Connell JX. Lipomatous hemangiopericytoma: a morphologically distinct soft tissue tumor. Arch Pathol Lab Med. 1999. 123:941–945.
15. Domanski HA. Fine-needle aspiration smears from lipomatous hemangiopericytoma need not be confused with myxoid liposarcoma. Diagn Cytopathol. 2003. 29:287–291.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download