Abstract
Nontuberculous mycobacterial (NTM) diseases are increasing worldwide. However NTM lung disease in organ transplant recipients has been rarely reported. Here, we report 2 cases of NTM lung disease in heart transplant recipients. A 37-year-old man, who had undergone a heart transplant one year previous, was admitted to hospital due to a cough. Chest CT scan showed multiple centrilobular nodules in both lower lungs. In his sputum, M. abscessus was repeatedly identified by rpoB gene analysis. The patient improved after treatment with clarithromycin, imipenem, and amikacin. An additional patient, a 53-year-old woman who had undergone a heart transplant 4 years prior and who suffered from bronchiectasis, was admitted because of purulent sputum. The patient's chest CT scan revealed aggravated bronchiectasis; M. intracellulare was isolated repeatedly in her sputum. Treatment was successfully completed with clarithromycin, ethambutol, and ciprofloxacin. NTM lung disease should be considered as a potential opportunistic infection in organ transplant recipients.
Figures and Tables
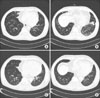
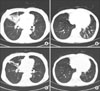
Figure 1
HRCT scan showed multiple centrilobular nodules with branching linear opacity and bronchiectasis predominantly in both lower lobes (A, B). After treatment for M. abscessus, the lesions were resolved (C, D).
References
1. Park JS. Respiratory review of 2009: nontuberculous mycobacterium. Tuberc Respir Dis. 2009. 67:395–401.
2. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007. 175:367–416.
3. Koh WJ, Kwon OJ. Diagnosis and treatment of nontuberculous mycobacterial lung disease. Korean J Med. 2008. 74:120–131.
4. Kotloff RM, Ahya VN, Crawford SW. Pulmonary complications of solid organ and hematopoietic stem cell transplantation. Am J Respir Crit Care Med. 2004. 170:22–48.
5. Kim YJ, Jeon EK, Cho BS, Choi SM, Lee S, Min CK, et al. A case of pneumatosis cystoides intestinalis in an allogenic stem cell transplant recipient who had bronchiolitis obliterans and pulmonary infection by mycobacterium abscessus. Infect Chemother. 2008. 40:271–275.
6. Doucette K, Fishman JA. Nontuberculous mycobacterial infection in hematopoietic stem cell and solid organ transplant recipients. Clin Infect Dis. 2004. 38:1428–1439.
7. Sexton P, Harrison AC. Susceptibility to nontuberculous mycobacterial lung disease. Eur Respir J. 2008. 31:1322–1333.
8. Novick RJ, Moreno-Cabral CE, Stinson EB, Oyer PE, Starnes VA, Hunt SA, et al. Nontuberculous mycobacterial infections in heart transplant recipients: a seventeen-year experience. J Heart Transplant. 1990. 9:357–363.
9. Razonable RR. Nontuberculous mycobacterial infections after transplantation: a diversity of pathogens and clinical syndromes. Transpl Infect Dis. 2009. 11:191–194.
10. Muñoz RM, Alonso-Pulpón L, Yebra M, Segovia J, Gallego JC, Daza RM. Intestinal involvement by nontuberculous mycobacteria after heart transplantation. Clin Infect Dis. 2000. 30:603–605.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download