Abstract
Background
From November 2006, The national health insurance system in the Republic of Korea began to cover prescribed long-term oxygen therapy (LTOT) in patients with chronic respiratory insufficiency. This study examined the current status of LTOT after national health insurance coverage.
Methods
Between November 1, 2006 and June 30, 2008, the medical records of patients who were prescribed LTOT by chest physicians were reviewed. The data was collected from 13 university hospitals.
Results
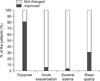
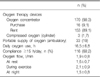
197 patients (131 male and 66 female) were prescribed LTOT. The mean age was 64.3±13.0 years. The most common underlying disease was chronic obstructive pulmonary disease (n=103, 52.3%). Chest physicians prescribed LTOT using arterial blood gas analysis or a pulse oxymeter (74.6%), symptoms (14%), or a pulmonary function test (11.2%). The mean oxygen flow rate was 1.56±0.68 L/min at rest, 2.08±0.91 L/min during exercise or 1.51±0.75 L/min during sleep. Most patients (98.3%) used oxygen concentrators. Only 19% of patients used ambulatory oxygen supplies. The oxygen saturation before and after LTOT was 83.18±10.48% and 91.64±7.1%, respectively. After LTOT, dyspnea improved in 81.2% of patients. The mean duration of LTOT was 16.85±6.71 hours/day. The rental cost for the oxygen concentrator and related electricity charges were 48,414±15,618 won/month and 40,352±36,815 won/month, respectively. Approximately 75% of patients had a regular visit by the company. 5.8% of patients had personal pulse oxymetry. 54.9% of patients had their oxygen saturation checked on each visit hospital. 8% of patients were current smokers. The most common complaint with LTOT was the limitation of daily activity (53%). The most common complaint with oxygen concentrators was noise (41%).
Figures and Tables
Figure 2
Changes of SaO2 before and after the use of LTOT Using the paired t-test, p<0.001. LTOT: long-term oxygen therapy.

References
1. Medical Research Council Working Party. Long term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema. Lancet. 1981. 1:681–686.
2. Nocturnal Oxygen Therapy Trial Group. Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease: a clinical trial. Nocturnal Oxygen Therapy Trial Group. Ann Intern Med. 1980. 93:391–398.
3. Croxton TL, Bailey WC. Long-term oxygen treatment in chronic obstructive pulmonary disease: recommendations for future research: an NHLBI workshop report. Am J Respir Crit Care Med. 2006. 174:373–378.
4. Jones A, Wood-Baker R, Walters EH. Domiciliary oxygen therapy services in Tasmania: prescription, usage and impact of a specialist clinic. Med J Aust. 2007. 186:632–634.
5. Borras JM, Granados A, Escarrabill J, de Lissovoy G. Complex decisions about an uncomplicated therapy: reimbursement for long-term oxygen therapy in Catalonia (Spain). Health Policy. 1996. 35:53–59.
6. Dilworth JP, Higgs CM, Jones PA, White RJ. Acceptability of oxygen concentrators: the patient's view. Br J Gen Pract. 1990. 40:415–417.
7. Pelletier-Fleury N, Lanoe JL, Fleury B, Fardeau M. The cost of treating COPD patients with long-term oxygen therapy in a French population. Chest. 1996. 110:411–416.
8. Department of Insurance Benefit, National Health Insurance Corporation, Korea. Report on the survey about home oxygen therapy 2007. 2007. Seoul: National Health Insurance Corporation.
9. National Health Insurance Corporation, Korea. Public bulletin No. 2006-1. 2006. Seoul: National Health Insurance Corporation, Korea.
10. Ministry for Health, Welfare and Family Affairs, Korea. Public notification No. 2007-66. 2007. Seoul: Ministry for Health, Welfare and Family Affairs, Korea.
11. Jemal A, Ward E, Hao Y, Thun M. Trends in the leading causes of death in the United States, 1970-2002. JAMA. 2005. 294:1255–1259.
12. Korea National Statistical Office. Annual report on the cause of death statistics 2006. 2007. Daejeon: Korea National Statistical Office.
13. Tarpy SP, Celli BR. Long-term oxygen therapy. N Engl J Med. 1995. 333:710–714.
14. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) [Internet]. c2009. [place unknown]: GOLD;Available from: http://www.goldcopd.com.
15. ACCP-NHLBI National Conference on Oxygen Therapy. Chest. 1984. 86:234–247.
16. Lowson KV, Drummond MF, Bishop JM. Costing new services: long-term domiciliary oxygen therapy. Lancet. 1981. 1:1146–1149.
17. Oxygen concentrators. Health Devices. 1993. 22:485–497.
18. Ministry for Health, Welfare and Family Affairs, Korea. Public notification No. 2006-77. 2006. Seoul: Ministry for Health, Welfare and Family Affairs, Korea.
19. Petty TL, O'Donohue WJ Jr. Further recommendations for prescribing, reimbursement, technology development, and research in long-term oxygen therapy. Summary of the Fourth Oxygen Consensus Conference, Washington, D.C., October 15-16, 1993. Am J Respir Crit Care Med. 1994. 150:875–877.
20. Huh JW, Lee JY, Hong SB, Oh YM, Shim TS, Lim CM, et al. Long-term oxygen therapy in patients with chronic respiratory failure in one university hospital. Tuberc Respir Dis. 2005. 58:160–166.
21. Katsenos S, Charisis A, Daskalopoulos G, Constantopoulos SH, Vassiliou MP. Long-term oxygen therapy in chronic obstructive pulmonary disease: the use of concentrators and liquid oxygen systems in north-western Greece. Respiration. 2006. 73:777–782.
22. Morrison D, Skwarski KM, MacNee W. The adequacy of oxygenation in patients with hypoxic chronic obstructive pulmonary disease treated with long-term domiciliary oxygen. Respir Med. 1997. 91:287–291.
23. Górecka D, Gorzelak K, Sliwińki P, Tobiasz M, Zieliński J. Effect of long-term oxygen therapy on survival in patients with chronic obstructive pulmonary disease with moderate hypoxaemia. Thorax. 1997. 52:674–679.
24. Ringbaek TJ, Lange P, Viskum K. Are patients on long-term oxygen therapy followed up properly? Data from the Danish Oxygen Register. J Intern Med. 2001. 250:131–136.
25. Article, No. 44. Law of National Health Insurance, Korea.
26. Center for Rare disorder, Korea Centers for Disease Control and Prevention. 2008 Rare disorders which were supported for medical cost. 2008. Seoul: National Institute of Health, Korea.
27. O'Reilly P, Bailey W. Long-term continuous oxygen treatment in chronic obstructive pulmonary disease: proper use, benefits and unresolved issues. Curr Opin Pulm Med. 2007. 13:120–124.




 PDF
PDF ePub
ePub Citation
Citation Print
Print










 XML Download
XML Download