Abstract
Acute suppurative thyroiditis is a rare disease because the thyroid gland is remarkably resistant to infection. We present a 2-year-old girl with refractory acute suppurative thyroiditis due to a pyriform sinus fistula (PSF). She complained of fever and painful anterior neck swelling. Her condition did not completely improved by multiple parenteral antibiotics along with incision and drainage. Barium esophagogram to detect PSF demonstrated no specific finding. Computed tomography scan showed air bubble superior to the left thyroid gland which indicated a possible fistula connected to the pyriform sinus. An intraoperative laryngoscopy revealed a 2-mm-sized fistula opening. The fistula was successfully treated by chemocauterization with trichloroacetic acid.
Acute suppurative thyroiditis (AST) is a rare infectious disease particularly in childhood because of the high iodine content, rich blood and lymphatic supply and protective fibrous capsule of the thyroid gland1,2). Accordingly, any thyroid or recurrent neck infection in immunocompetent children should raise a suspicion for the presence of predisposing conditions such as pyriform sinus fistula (PSF) or thyroglossal duct remnant. Diagnosis can be made by high resolution ultrasonogram (US), barium studies, computed tomography (CT) scan and endoscopic examination. Treatment with antibiotics and/or incision and drainage (I&D) is indicated during acute exacerbations. Permanent cure from PSF can only be attained by complete fistulectomy or chemocauterization.
A 2-year-old girl presented with fever for 1 week and painful anterior neck swelling for 4 days. Palpation revealed a 4-cm-×3-cm-sized anterior neck mass with tenderness and erythema of the overlying skin. Laboratory tests showed white blood cell count of 20,540/µL with shift to the left. C-reactive protein (CRP) was 17.6 mg/dL and erythrocyte sedimentation rate (ESR) was 120 mm/hr. Thyroid-stimulating hormone (TSH) was 1.75 mIU/L (normal range, 0.7-6.4 mIU/L), total T3 was 1.25 mmol/L (normal range, 1.54-4 mmol/L) and free-T4 was 20.32 pmol/L (normal range, 10-28 pmol/L). Thyroid scan showed diffusely decreased uptake of Tc-99m pertechnetate in the thyroid gland (Fig. 1). US demonstrated an enlarged thyroid gland with diffuse heterogeneous parenchymal echotexture and multiple reactive lymph node enlargement (Fig. 2). The fever subsided one day after intravenous cefotetan treatment, but the neck swelling persisted. Recurrence of the fever and fluctuation of the overlying skin on the swollen neck were noted on the 7th day of hospitalization. CT scan revealed multiple abscesses in both lobes of the thyroid gland without definite evidence of fistula connected to the pyriform sinus (Fig. 3). Antibiotics were changed to meropenem, teicoplanin and clindamycin. US-guided fine needle aspiration and I&D were performed on the 9th and 18th day, respectively. On 20th day, follow-up thyroid function test showed hypothyroidism. (TSH was 48.23 mIU/L, total T3 was 1.51 mmol/L and free-T4 was 5.06 pmol/L). Levothyroxine was prescribed at a dose of 3 mcg/kg. Pus continued to drain through the incision site even though the fever subsided. On the 32th day, removal of granulation tissues at the I&D site and drainage of pus was done. No bacteria was identified on three consecutive pus cultures. On the 37th day, she was trasferred to Seoul National University Hospital for further evaluation of the underlying deformity. Two esophagograms were unable to demonstrate fistula or other anatomical defect (Figs. 4, 5). Follow-up CT scan was taken because of continuous drainage of pus with erythema and tenderness of the skin. Air bubble superior to the left thyroid gland was discovered, suggestive of a fistula connected to the pyriform sinus (Fig. 6). Two-mm-sized fistula was identified and was successfully treated with chemocauterization using trichloroacetic acid by intraoperative laryngoscopy. The patient was discharged 5 days after the operation. Levothyroxine was stopped 1 week after the operation, and thyroid function test performed after 1week was normal. TSH was 3.9 mIU/L, total T3 was 78.2 ng/dL (normal range, 58-159 mmol/L) and free-T4 was 0.93 ng/dL (normal range, 0.8-2.2 ng/dL). No recurrence was observed after 2 years of follow-up.
AST is a rare infectious disease particularly in childhood. Usually, patients with AST have predisposing factors including congenital defect such as PSF or thyroglossal duct cyst, preexisting thyroid disease and compromised immune system3). A wide variety of microbial pathogens such as Staphylococcus, Streptococcus, Hemophilus influenza, Klebsiella, Escherichia coli, Pseudomonas, Enterobacter, Salmonella and anaerobes which are commonly found as normal flora in the oral cavity, have been reported as causes of AST. Rarely, Mycobacteria, Aspergillus, Coccidioidesimmitis, Cryptococcus neoformans, Histoplasma capsulatum, Candida, Treponema pallidum, and Echinococcus have been identified. As much as 30% of suppurative thyroiditis are polymicrobial infection1,3,4).
The routes of infection are through blood stream or lymphatics, direct inoculation from adjacent tissue or congenital anomaly such as PSF which is a remnant of the 3rd or 4th pharyngeal pouch. The sinus tract begins from the apex or base of the pyriform sinus, courses anterio-inferiorly, into either the perithyroid tissue or thyroid parenchyma5,6). Because of asymmetric embryological development, it usually located at left side and most often associated with left-sided neck infection. In the acute inflammatory phase, swelling of mucosa and adjacent tissue can cause partial or complete obstruction of the fistula tract and identification the fistula tract may be difficult3). Therefore, evaluation for anatomical defect in recurrent thyroiditis or neck infection should be done after management of the acute inflammation2,7). In our case, even though no evidence of PSF was seen at CT scan which was done in acute inflammatory phase, follow up CT scan detected air bubble, suggestive of PSF.
Clinical features of AST include fever, cough, hoarseness, dysphagia, sore throat, anterior neck swelling and limitation of cervical extension1). Both thyroid gland lobes can be affected but the left lobe is more frequently involved. Leukocytosis and increased ESR and CRP are common. Normal thyroid function tests are typical, although transient or permanent hypothyroidism can occur in about 2%-3% of patients and thyrotoxicosis may occur in 5% as a result of the disease or treatment1,3). US show heterogeneous echogenicity of the thyroid gland with irregular margin and inflammatory changes. CT scan is a useful modality for detecting loss of the normal high density of the thyroid gland, abscess formation and air density of a sinus or fistula. Radionulide thyroid scan generally shows absent or decreased uptake in the affected thyroid lobe. An esophagogram can detect underlying anatomical defect. Direct inspection by laryngoscopy or endoscopic hypopharyngoscopy is becoming increasingly useful to identify the internal opening of a PSF and appears to be a more sensitive diagnostic test compared with CT scan and barium esophagogram3,8).
Therapy with empiric antibiotics include penicillinase-resistant penicillin or combination of a penicillin and a β-lactamase inhibitor can improve the AST. Penicillin, clindamycin, combination of macrolide and metronidazole is sometimes recommended. Most suppurative thyroiditis are treated successfully and completely with appropriate antibiotics medication with I&D although transient alteration of thyroid function may occur. If no clinical improvement occurs after 36-48 hours of therapy, a reassessment is needed to detect the presence of abscess and PSF1,3). Also, recurrent infection of neck or thyroid gland, especially left sided, evaluation for underlying anomaly such as PSF should be done2,9). Treatment of choice for PSF is elective excision. Recently, electrical or chemical cauterization using silver nitrate, trichloroacetic acid or histoacry have been used in a lot of cases2,3) Most suppurative thyroiditis are treated successfully and completely even though transient altered thyroid function has occurred.
In conclusion, patients with recurrent or refractory AST frequently have an underlying predisposing condition. Esophagogram, CT scan or laryngoscopy should be used to look for an underlying anomaly such as PSF. Besides elective excision, cauterization, which is less invasive, can cure PSF successfully.
References
1. Brook I. Microbiology and management of acute suppurative thyroiditis in children. Int J Pediatr Otorhinolaryngol. 2003; 67:447–451. PMID: 12697345.

2. Sai Prasad TR, Chong CL, Mani A, Chui CH, Tan CE, Tee WS, et al. Acute suppurative thyroiditis in children secondary to pyriform sinus fistula. Pediatr Surg Int. 2007; 23:779–783. PMID: 17534632.

3. Paes JE, Burman KD, Cohen J, Franklyn J, McHenry CR, Shoham S, et al. Acute bacterial suppurative thyroiditis: a clinical review and expert opinion. Thyroid. 2010; 20:247–255. PMID: 20144025.

4. Wongphyat O, Mahachoklertwattana P, Molagool S, Poomthavorn P. Acute suppurative thyroiditis in young children. J Paediatr Child Health. 2012; 48:E116–E118. PMID: 21535286.

5. Hatabu H, Kasagi K, Yamamoto K, Iida Y, Misaki T, Hidaka A, et al. Acute suppurative thyroiditis associated with piriform sinus fistula: sonographic findings. AJR Am J Roentgenol. 1990; 155:845–847. PMID: 2119120.

6. Nicoucar K, Giger R, Jaecklin T, Pope HG Jr, Dulguerov P. Management of congenital third branchial arch anomalies: a systematic review. Otolaryngol Head Neck Surg. 2010; 142:21–28.e2. PMID: 20096218.

7. Schneider U, Birnbacher R, Schick S, Ponhold W, Schober E. Recurrent suppurative thyroiditis due to pyriform sinus fistula: a case report. Eur J Pediatr. 1995; 154:640–642. PMID: 7588965.

8. Fukata S, Miyauchi A, Kuma K, Sugawara M. Acute suppurative thyroiditis caused by an infected piriform sinus fistula with thyrotoxicosis. Thyroid. 2002; 12:175–178. PMID: 11916288.

9. Yolmo D, Madana J, Kalaiarasi R, Gopalakrishnan S, Kiruba Shankar M, Krishnapriya S. Retrospective case review of pyriform sinus fistulae of third branchial arch origin commonly presenting as acute suppurative thyroiditis in children. J Laryngol Otol. 2012; 126:737–742. PMID: 22624855.

Fig. 1
Thyroid scan shows decreased uptake of Tc-99m pertechnetate in the diffuse area of the thyroid gland.

Fig. 2
Ultrasonogram shows (A) enlarged thyroidi gland with diffuse heterogenous echotexture (arrow) and (B) multiple reactive lymph node enlargement.

Fig. 3
Computed tomography scan shows multiple hypodense abscesses in both lobes of the thyroid gland.
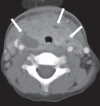
Fig. 4
Contrast was infused through an incision wound at the anterior side of the neck. There was contrast filling at the posterior pharynx, but the pathway was not compatible with a pyriform sinus fistula.

Fig. 5
Esophagogram was checked while swallowing contrast medium. No pyriform sinus fistula tract was demonstrated.

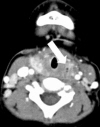
Fig. 6
Neck computed tomography scan shows air bubble superior to the left thyroid gland, which is suspicious for a fistula connected to the pyriform sinus (arrow). The scan also shows slightly decreased extent of the thyroid gland but no interval changes in the bilateral multiple enlarged lymph nodes, suggesting reactive hyperplasia.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download