1. Scivoletto G, Fuoco U, Badiali D, Braccl F, Lucente LD, Patrelli A, Vona VU, Tnillo D, Castellano V, Corazzian E. Gastrointestinal dysfunction following stroke. J Neurol Sci. 1997; 150:S151.
2. Robain G, Chennevelle JM, Petit F, Piera JB. Incidence of constipation after recent vascular hemiplegia: a prospective cohort of 152 patients. Rev Neurol. 2002; 158:589–592. PMID:
12072827.
3. Harari D, Norton C, Lockwood L, Swift C. Treatment of constipation and fecal incontinence in stroke patients: randomized controlled trial. Stroke. 2004; 35:2549–2555. PMID:
15486330.
4. Krogh K, Christensen P, Laurberg S. Colorectal symptoms in patients with neurological disease. Acta Neurol Scand. 2001; 103:335–343. PMID:
11421845.
5. Roth EJ. Medical complication encountered in stroke rehabilitation. Phy Med Rehabil Clin North Am. 1991; 2:563–578.
6. Wrenn K. Fecal impaction. N Engl J Med. 1989; 321:658–662. PMID:
2671728.

7. Bracci F, Badiali D, Pezzotti P, Scivoletto G, Fuoco U, Di Lucente L, Petrelli A, Corazziari E. Chronic constipation in hemiplegic patients. World J Gastroenterol. 2007; 13:3967–3972. PMID:
17663511.
8. Garrigues V, Bau I, Bastida G, Galvez C, Ponce J. Concordance between rome and rome II criteria for chronic constipation, a population-based study. Gastroenterology. 2001; 120:A634.

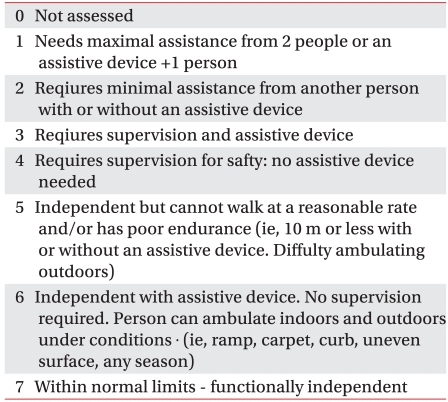
9. Demeurisse G, Demol O, Robaye E. Motor evaluation in vascular hemiplegia. Eur Neurol. 1980; 19:382–389. PMID:
7439211.

10. Korner-Bitensky N, Mayo N, Cabot R, Becker R, Cooperismith H. Motor and functional recovery after stroke: accuracy of physical therapists' predictions. Arch Phys Med Rehabil. 1989; 70:95–99. PMID:
2644920.
11. Su Y, Zhang X, Zeng J, Pei Z, Cheung RT, Zhou QP, Ling L, Tan J, Zhang Z. New-onset constipation at acute stage after first stroke incidence, risk factors, and impact on the stroke outcome. Stroke. 2009; 40:1304–1309. PMID:
19228840.
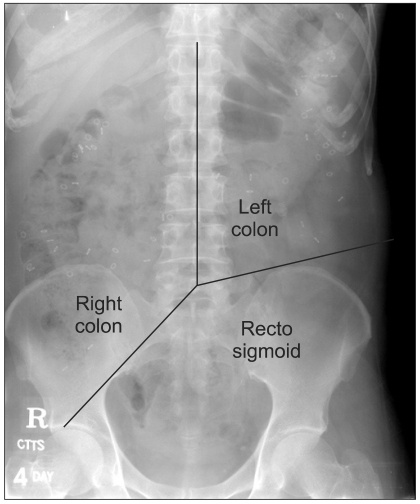
12. Metcalf AM, Phillips SF, Zinsmeister AR, MacCarty RL, Beart RW, Wolff BG. Simplified assessment of segmental colonic transit. Gastroenterology. 1987; 92:40–47. PMID:
3023168.

13. De Looze DA, De Muynck MC, Van Laere M, De Vos MM, Elewaut AG. Pelvic floor function in patients with clinically complete spinal cord injury and its relation to constipation. Dis Colon Rectum. 1998; 41:778–786. PMID:
9645749.

14. Choi H. Measurement of Colon transit time. Korean J Gastrointest Motil. 1999; 5:198–206.
15. Belsey J, Greenfield S, Candy D, Geraint M. Systemic review: impact of constipation on quality of life in adults and children. Aliment Pharmacol Ther. 2010; 31:938–949. PMID:
20180788.
16. Lehmann JF, DeLateur BJ, Fowler RS Jr, Warren CG, Arnhold R, Schertzer G, Hurka R, Whitemor JJ, Masock AJ, Chambers KH. Stroke rehabilitation: outcome and prediction. Arch Phys Med Rehabil. 1975; 56:383–389. PMID:
809023.
17. Jongbloed L. Prediction of function after stroke: a critical review. Stroke. 1986; 17:765–776. PMID:
3526649.

18. Skilbeck CE, Wade DT, Hewer RL, Wood VA. Recovery after stroke. J Neurol Neurosurg Psychiatry. 1983; 46:5–8. PMID:
6842200.

19. Rao SS, Sadeghi P, Beaty J, Kavlock R, Ackerson K. Ambulatory 24-h colonic manometry in healty humans. Am J Physiol Gastrointest Liver Physiol. 2001; 280:G629–G639. PMID:
11254489.
20. Min KC, Chong SY, Chung JS. A survey of defecation pattern after discharge in stroke patients. J Korean Acad Rehabil Med. 2000; 24:388–394.
21. Nino-Murcia M, Stone JM, Chang PJ, Perkash I. Colon transit in spinal cord-injury patients. Invest Radiol. 1990; 25:109–112. PMID:
2312245.
22. Lim SS, Choi KH, Myung SJ, Sung IY. Evaluation of the neurogenic bowel by colon transit time and anorectal manometry in the spinal cord injured patients. J Korean Acad Rehabil Med. 2001; 25:249–255.
23. Del Giudice E, Staiano A, Capano G, Romano A, Florimonte L, Miele E, Ciarla C, Campanozzi A, Crisanti AF. Gastrointestinaal manifestations in children with cerebral palsy. Brain Dev. 1999; 21:307–311. PMID:
10413017.
24. Park ES, Park CI, Cho SR, Na SI, Cho YS. Colonic transit time and constipation in children with spastic cerebral plasy. Arch Phys Med Rehabil. 2004; 85:453–456. PMID:
15031832.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download