Abstract
Zygomatic fractures are the second most common fractures of the facial skeleton, after nasal bone fractures. Due to its uniqueness, the malar bone plays a very important role in maintaining appropriate facial contours. Zygomatic fractures can cause ocular and mandibular functional impairment, along with cosmetic defects. With the help of advanced imaging techniques and various treatment options, the management of zygomatic fractures has become more sophisticated and less invasive. This article discusses zygomatic fractures in detail: their clinical and radiographic features, and the various treatment options available.
The malar bone plays a unique role in maintaining facial contours and the underlying bony architecture1. Any break in continuity or dislocation of this bone disrupts ocular and mandibular functions, and may cause cosmetic defects. The zygoma is most vulnerable to fracture beyond the dorsum of the nose2. Due to its unique bony architecture, it can withstand blows of significant impact without being fractured. Zygomatic fractures can also lead to disarticulation from the suture line along the four articulation surfaces (i.e., the zygomaticomaxillary complex, the zygomatic complex [ZMC] proper, and the orbitozygomatic complex). Zygomatic fractures should be treated early because they can cause both functional and cosmetic defects. The most important functional defect encountered is reduced mouth opening due to impingement on the coronoid process3. This makes early diagnosis and management important. Zygomatic fractures require appropriate treatment because inadequate skeletal healing can cause reduced malar projection, resulting in facial cosmetic deformities. Accurate positioning of the fractured bone (posterior to the skull base and anterior to the midface) should be performed in order to repair the fragments. The ability to withstand the forces of a blow to the midface comes via a strong attachment of the frontal, maxillary, zygomatic, and sphenoid bones to one another. These bones are enclosed by the thicker bones of the facial buttress, providing strength and stability. The elements of the facial buttress are listed in Table 14.
The most accepted radiological procedure for establishing a proper diagnosis for midface fracture and zygomatic fracture is computed tomography (CT) scan. Bony structures, foreign bodies, hematoma, herniation, and emphysema are well depicted by this method8. Injuries can be analyzed in axial, coronal, and sagittal sections. For intricate trauma, three-dimensional reconstruction can be performed to further evaluate injury. Cone-beam computed tomography may be preferred for the three-dimensional presentation of zygomatic bone fractures, but the disadvantage of this procedure is its low significance regarding soft tissue structures. In this respect, the CT diagnostic procedure is superior. Furthermore, the orbit, eye muscles, optic nerve, and retroglobal hematoma can be well assessed with computed tomography9.
Undisplaced fractures without functional disturbances do not require surgical therapy8. Complex fractures lead to impairment of the infraorbital nerve (temporarily or permanently) due to trauma or impingement on its bony canal. Impingement of the infraorbital nerve by dislocated bone fragments indicates surgical correction1011. Dislocation of the fractured fragment in the medial direction can lead to impaired coronoid function, and thus impaired opening of the mouth. Such cases usually require open or closed reduction of the fracture fragments8.
In cases of undisplaced or minimally displaced fractures of the zygomatic bone, conservative procedures are the preferred options. These include physical measures (e.g., cooling) and drug therapy (e.g., analgesics or decongestion medication). The patient is instructed to eat soft meals to avoid secondary dislocation of the zygoma due to traction of the masseter muscle. Conservative treatment may also be indicated for severely impaired fractures, despite dislocation of the zygomatic bone. Patients with orbital complications, even without dislocation of the zygomatic bone complex, are candidates for emergency surgery12.
The reduction and fixation of fracture fragments should be performed as early as possible to avoid any functional and cosmetic deformities. The two biggest problems encountered are an uncertain repositioning of the fracture gaps, and an inappropriate postoperative stability of the repositioned zygomatic body. A closed reduction of zygomatic fractures is contraindicated if surgical correction of the orbital floor is required11. Closed reduction procedures are less labor-intensive, but still provide appropriate decompression of the infraorbital nerve. For the closed reduction of the zygomatic bone, two transcutaneous approaches are recommended. According to Gillies, the first approach consists of reaching the zygomatic bone through a small temporal incision8. The fascia of the temporalis muscle is incised to insert an elevator below the zygomatic arch. The second approach is performed percutaneously with a bone hook. A small incision is made 2 cm laterally to the temporal canthus, and the hook is inserted through the skin under the zygomatic bone, where it is then repositioned13. Percutaneous insertion of a “Caroll-Girard” screw is a less traditional technique to pull the zygomatic bone into an undislocated position, and to reposition it11. In 2014, Patil and Patil14 used Gillies temporal approach in three cases of left ZMC fracture. They concluded that it is a desirable approach for undisplaced zygomatic fractures due to its simple, effective, and cosmetically acceptable results. In 2013, Salinas et al.15 treated 23 patients with zygomaticomaxillary complex fractures using a closed reduction method with Steinmann-pin fixation. They compared their outcomes (reduction and esthetic) with those of patients who underwent open reduction and internal fixation (ORIF) techniques. They found that the average facial incision length was shorter than that associated with traditional methods, which often require multiple incisions. They concluded that their method of repairing ZMC fractures provided adequate bony alignment and esthetics, shorter operating times, only one small incision, and excellent patient outcomes.
In order to avoid making further incisions, several authors have described approaching a fracture through traumatic skin lesions. According to Kühnel et al., midface trauma is closely related to soft tissue lesions. If these lesions are located and sized appropriately, they can be used as access points for fracture reduction and fixation. If access to the fracture is small, the incision can be extended parallel to the natural skin lines11.
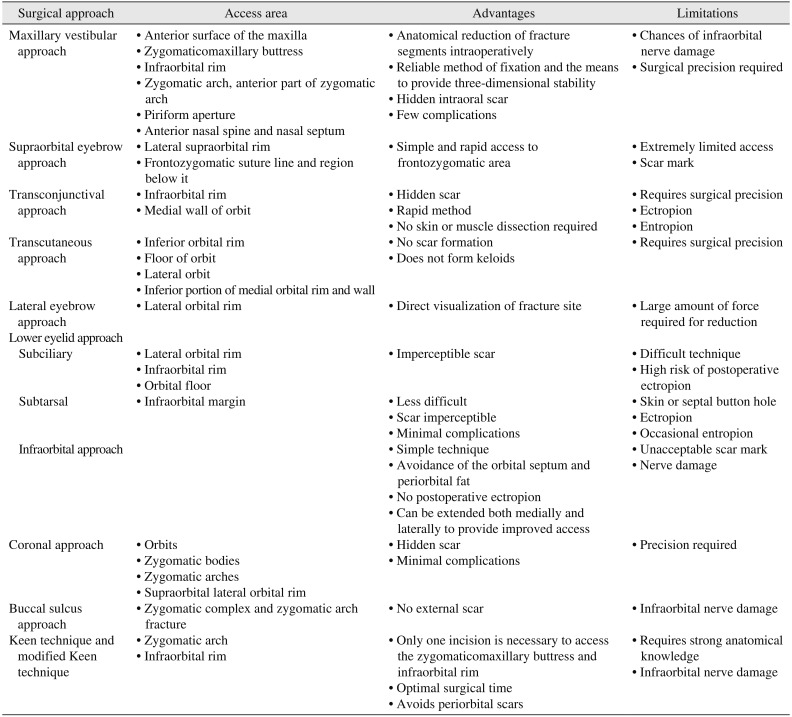
According to The AO Foundation, this method can be used for the complete exposure of the maxilla, nose, and ethmoid region. Rehman et al.16 conducted a study on 81 patients with zygomatic bone fractures to determine patterns of fracture, etiology, and treatment options. The author described several advantages to this approach.(Table 4)
This popular approach is used to gain access to the lateral orbital rim. No important neurovascular structures are at risk with this approach. If the incision is extended inferiorly for better exposure, it crosses the resting tension line (or crow's feet) perpendicularly. This affects cosmetic eyebrow removal, and restricts its use in women17. This approach has certain advantages and limitations.(Table 4) Fernandes et al.18 used this technique on 16 patients and concluded that this approach is safe and useful in selected cases (e.g., lesions near the anterior fossa, suprasellar cisterns, and Sylvian fissure). The authors described good postoperative and cosmetic results. Other researchers treated ZMC fractures using two point fixations and a supraorbital approach. They also obtained favorable results in relation to postoperative stability and esthetics19.
The transconjunctival incision is also known as the inferior fornix incision. Depending on the relationship of the orbital septum to the path of dissection, Bourguet in 1928 described this approach as preseptal or retroseptal. On the basis of skin incisions in the lower eyelid, the transcutaneous approach has been given many names in the literature (e.g., blepharoplasty, subciliary, lower eyelid, mid-eyelid, subtarsal, and infraorbital rim)17. In 2010, Langsdon et al.20 conducted a retrospective study on 45 patients to compare the transconjunctival approach with the transcutaneous approach. They concluded that the upper-lid transconjunctival approach was a safe technique offering excellent access to the lateral orbital rim, with few complications. When compared with a lower-lid transconjunctival incision, it offered reduction of zygomaticomaxillary complex fractures without any external scar marks. When compared with traditional transcutaneous approaches, it had fewer postoperative complications. All of these techniques have certain advantages and limitations. (Table 4) Rajkumar et al.21 conducted a prospective evaluation of ten patients using the ‘Y’ modification of the transconjunctival approach for ZMC fractures. They concluded that this modification provided excellent surgical exposure of the fracture site while avoiding the second incision in the area of the frontozygomatic (FZ) suture. Apart from its advantages, this modification had certain limitations, such as increased operating times and the need for a complete knowledge of the anatomy of the lateral canthal region. Few authors have mentioned these approaches in their studies, or that the ZF suture can be visualized by dissecting up along the lateral orbital rim. However, this can lead to a prolonged duration of swelling in the upper lid, resulting in a “hooded” appearance for a period of time22.
The lateral eyebrow approach is the most commonly used technique to elevate the fracture segment through an eyebrow incision17. In a study on 30 patients, Thangavelu et al.23 observed that this approach is not advisable for treating an isolated arch fracture. It also leaves a visible scar in the lateral orbital region. They concluded that this approach is ideal for the reduction and treatment of zygomatic bone and arch fractures. Ebenezer et al.24 observed that this approach provides minimal postoperative complications. This technique has certain advantages and limitations.(Table 4)
In 1944, Converse et al. first reported the open reduction of infraorbital rim and floor fractures through subciliary incision, and acknowledged the superior scar produced by this technique25. In 1924, Bourguet et al. were the first to use the transconjunctival approach for cosmetic blepharoplasty (to remove a herniated fat pad)26. This incision (with a lateral canthotomy) exposes infraorbital rim and floor fractures of the entire lower orbital rim and zygoma27. Crosara et al.28 analyzed and compared esthetic outcomes after the use of subciliary, subtarsal, and infraorbital incisions to approach the infraorbital rim and orbital floor in the repair of orbital fractures. The author reported better surgical and esthetic results with subciliary and subtarsal incisions, compared to infraorbital incisions. The rate of unnoticeable scars was significantly higher with subciliary and subtarsal incisions relative to infraorbital incisions. Holtmann et al.29 reported no significant difference in the rate of scarring among subciliary, subtarsal, and infraorbital incisions. Heckler et al.30 analyzed 154 subciliary incisions and reported that in 100% of cases, the scar appearance was considered to be excellent. The incidence of ectropion varies across different studies. All of these techniques have certain advantages and limitations.(Table 4) One study evaluated and compared the efficacy of the two most commonly applied approaches for the treatment of infraorbital floor and rim fractures in twenty patients: the preseptal transconjunctival approach with lateral canthotomy, and the subciliary approach. The results showed a higher rate of ectropion in the transconjunctival group than in the subciliary group. The subciliary approach also offered lower morbidity and a lower risk of complications31. Other researchers evaluated the ‘Y modification’ of the transconjunctival approach for ZMC fractures. They concluded that this modification provides excellent surgical exposure and esthetics while avoiding the second incision in the area of the ZF suture32. But this modification also requires more operating time and a detailed knowledge of the anatomy of the lateral canthal region33.
This flap is an extremely useful incision for surgery of the zygomatic arch. It is a modified incision of the preauricular flap described by Al-Kayat and Bramley. It has several advantages and limitations.(Table 4) The incision for this approach varies in design from a bow-like incision to geometric patterns (zig-zag, saw tooth, stepwise, or wave-like designs). These types of incision allow an accurate closure34. According to Rajmohan et al.35, this incision (with its various modifications) provides a multifaceted approach with excellent exposure to various areas in the craniomaxillofacial region. The hidden scar in the hairline provides an esthetic advantage, and has thus gained popularity. The authors observed that this approach offers wide visibility and accessibility to the entire upper third and middle third of the face in less than twenty minutes. This approach has minimal postoperative complications and offers several other advantages relevant to surgical treatment of the craniomaxillofacial region, including superior esthetic results. According to Zhuang et al.36, this approach should be the first choice for comminuted and multiple zygomaticomaxillary complex fractures. This is due to its accurate reduction and fixation of fragments, its good cosmetic results, and its minimal complications.
According to some authors, this popular technique is considered a simple and productive alternative to other, more complicated procedures. It has many advantages.(Table 4) This approach is often seen as the initial procedure required for most ZMC fractures37. In a study of 50 cases, Courtney38 concluded that this approach is safe, rapid, and effective for treating zygomatic fractures.
This technique was first introduced by Keen in 1909. It allows an adequate visualization and reduction of zygomaticomaxillary buttress and zygomatic arch fractures39.(Table 4) Researchers have since modified the Keen technique. In this technique, a horizontal upper sulcus incision is made from the lateral incisor to the first molar. The mucoperiosteal flap is elevated, and the infraorbital nerve is dissected to reach the infraorbital rim. This allows the visualization, reduction, and fixation of the zygomaticomaxillary buttress. In addition, it is possible to install a miniplate when necessary. These advantages minimize morbidity and reduce surgical time39.
The zygomatic bone plays a critical role in maintaining normal facial esthetics and function. It also plays an important role in protecting the eyes. Rarely is the malar bone alone involved in fractures. Its articulating surfaces (with the maxilla, temporal, frontal, and sphenoid bones) are typically also involved. Hence, the malar bone needs to be stabilized at all its surfaces to achieve normal facial esthetics and function. The osteosynthesis of zygomatic bone fractures is classified as 1-point, 2-point, 3-point, or 4-point fixation, depending on the position of the fracture fragments40. The Reference Guide of the AO Foundation suggests that a 3-point fixation gives better stabilization than a 2-point fixation (which still gives considerable stabilization)11. However, studies have suggested that for non-comminuted fractures of the zygomatic bone or the lateral orbital wall, a 1-point fixation gives acceptable results for esthetics and stabilization40.
Simple fractures of the ZMC can be easily fixed with one miniplate. The most common access strategy uses an intraoral approach, providing a view of the zygomaticoalveolar crest and the infraorbital rim. Indications for this approach include a break in continuity only at the FZ suture. This fixation technique is most commonly used at the FZ suture. Some researchers have found that non-comminuted tripod fractures with mild or no displacement can be stabilized with a single-point fixation in the FZ area, without any diplopia or enophthalmos. The zygoma provides the attachment point for muscles of mastication and facial animation, and it withstands the forces of contraction of the masseter muscle41. Fujioka et al.42 demonstrated that 1-point fixation gives 3-point alignment and rigidity for non-comminuted fractures. Kim et al.43 reduced ZMC fracture fragments through an intraoral approach. In the absence of comminution of the zygoma or the lateral orbital rim (with or without minimal displacement), they achieved sufficient rigidity and esthetics with a 1-point fixation at this region.
This is a useful strategy for the exposition of the lateral orbital rim, the zygomaticosphenoid suture, and the infraorbital rim when the second point of stabilization by means of a plate is required. This method gives an accurate, three-dimensional reposition as well as a stable osteosynthetic fixation11. Ebenezer et al.24 concluded that a 2-point miniplate fixation at the infraorbital and FZ region gave acceptable results for postoperative stability and esthetics. It also ruled out infraorbital paresthesia in ZMC fractures.
The lateral orbital rim, the infraorbital edge, and the zygomaticoalveolar crest can be exposed and stabilized three-dimensionally at all three points by means of osteosynthesis11. Rana et al.44 conducted a study on 100 patients to compare the zygomatic bone after ORIF treatment using 2-point or 3-point fixation procedures. The authors concluded that ORIF using a 3-point fixation procedure with miniplates is the best available method for the treatment of zygomatic bone fractures.
This method of exposition and fixation is used for exposing the three above-mentioned areas, and requires stabilization with osteosynthesis. It is indicated in isolated lateral fractures of the midface, and in pan-facial fractures with comminuted zygomatic bone and loss of facial projection. Coronal incision is the preferred method for exposition of the zygomatic arch40.
The treatment of facial fractures has undergone several improvements over recent decades. Methods of rigid internal fixation have allowed for accurate repairs of facial fractures and have reduced morbidity. Over the past ten years, surgeons have refined various endoscopic approaches to facial fracture repair in an effort to achieve results similar to traditional open (surgical) approaches, but with less morbidity. These technological advancements can be classified as (1) computer-aided pre-surgical planning; (2) intraoperative navigation; and (3) incision techniques. Computer-aided technology involves transferring CT data onto medical software platforms (CAD/CAM), where information can be analyzed and evaluated in three-dimensional planes. This allows three-dimensional reconstruction and/or reduction as required45. The preferred approaches for the diagnosis and evaluation of malar bone fractures are the transconjunctival approach, the limited blepharoplasty incision, and the transoral approach. Lee et al.46 have introduced an endoscopy-assisted repair procedure for malar bone fractures. This procedure requires a limited-access incision at the anterior margin of the helical crus, extending 2 cm superior to the auricle. This incision is used primarily to gain endoscopic access, and to facilitate the fixation of the proximal zygomatic arch fracture. A 1 cm transverse incision at orbital region I (a skin crease superior to the lateral canthal region) is used to gain access for plate fixation at the FZ and distal arch fracture. An upper buccal sulcus incision is used to directly access and stabilize the zygomaticomaxillary and infraorbital rim fracture.
ZMC fractures are the most common facial fractures after nasal fractures. Recent advances in imaging, incision techniques, and materials for fixation have given promising functional and esthetic outcomes. Surgeons have developed various incision techniques for treating zygomatic fractures. These include coronal, eyebrow, upper eyelid, transconjunctival, infraciliary, and lower eyelid incisions. They also include the maxillary vestibular approach, the temporal approach, and the supraorbital approach. Du Verney et al. have described closed reduction techniques that take advantage of the mechanical forces of the masseter and temporalis muscles on the zygoma23. Another closed reduction technique is Lothrop's transantral approach through the maxillary sinus, below the inferior turbinate. This technique does not provide a complete reduction of the zygomatic bone. The Keen intraoral approach offers the advantage of avoiding skin incisions, thereby avoiding visible scaring. This approach provides minimal dissection and excellent reduction, but it may result in increased rates of infection by introducing oral flora into the infratemporal fossa. Compared to the lateral orbital approach, Gillies temporal approach requires an extra incision to elevate the zygoma. Without this, the temporalis muscle may get injured, resulting in post-reduction trismus and damage to the superficial temporal artery. Dingman and Natvig concluded that most displaced zygomatic fractures should be treated by open reduction and direct wire fixation.23 These authors preferred the suprafrontal approach. Although various methods are available to treat a fractured zygoma, the most common techniques in use are Gillies temporal approach and the intraoral approach. While these methods provide excellent access to reduce fractures of the body and arch, the lateral orbital approach provides simple and rapid access to the lateral orbital rim. The same incision can be used for miniplate fixation at the FZ suture. No functionally important neurovascular structures are at risk in this approach. And, the treatment can be done under local anesthesia. The supraorbital approach can be used to reduce all types of zygoma and arch fractures23. The chosen incision technique depends entirely on the clinical situation of the patient and the surgeon's preference and expertise, although the most popular incision techniques for such fractures are the lateral eyebrow, the buccal sulcus, and the infraorbital incision techniques. To avoid unacceptable scarring and postoperative sequelae, the coronal approach is the preferred method for unhindered exposure of the ZMC, to achieve accurate reduction and fixation of the fracture fragments. This approach has the added advantage of minimal post-surgical complications. For mildly displaced fractures, closed reduction by the temporal (or intraoral) approach is equally good. In cases where an open reduction is required, fixation by miniplates is superior to fixation by wires. Similarly, a 3-point fixation is superior to a 2-point fixation, especially when wires are used as the fixation devices. Various modifications have been developed for these different incisions, to overcome the complications inherent to the different techniques. In conclusion, the selected approach must balance the perioperative risks, a surgeon's particular abilities (in terms of preferred incisions), the requirements of treatment, and the potential postoperative complications.
Notes
References
1. Ellis E 3rd, Kittidumkerng W. Analysis of treatment for isolated zygomaticomaxillary complex fractures. J Oral Maxillofac Surg. 1996; 54:386–400. PMID: 8600255.

2. Chowdhury SR, Menon PS. Etiology and management of zygomaticomaxillary complex fractures in the armed forces. Med J Armed Forces India. 2005; 61:238–240. PMID: 27407768.

3. Nayyar MS. Management of zygomatic complex fracture. J Coll Physicians Surg Pak. 2002; 12:700–705.
4. Manson PN, Hoopes JE, Su CT. Structural pillars of the facial skeleton: an approach to the management of Le Fort fractures. Plast Reconstr Surg. 1980; 66:54–62. PMID: 7394047.
5. Hwang K, Kim DH. Analysis of zygomatic fractures. J Craniofac Surg. 2011; 22:1416–1421. PMID: 21772174.

6. Rowe NL, Killey HC. Fractures of the facial skeleton. 2nd ed. Edinburgh, London: E&S Livingstone;1968.
7. Knight JS, North JF. The classification of malar fractures: an analysis of displacement as a guide to treatment. Br J Plast Surg. 1961; 13:325–339. PMID: 13757119.

8. Marinho RO, Freire-Maia B. Management of fractures of the zygomaticomaxillary complex. Oral Maxillofac Surg Clin North Am. 2013; 25:617–636. PMID: 24055372.
10. Hardt N, Kuttenberger J. Craniofacial trauma. Berlin, Heidelberg, New York: Springer;2010.
11. Cornelius CP, Gellrich N, Hillerup S, Kusumoto K, Schubert W, Fusetti S. AO Surgery Reference [Internet]. Davos: AO Foundation;cited 2017 Jan 15. Available from: https://www2.aofoundation.org/wps/portal/surgery.
12. Evans BG, Evans GR. MOC-PSSM CME article: Zygomatic fractures. Plast Reconstr Surg. 2008; 121(1 Suppl):1–11.

13. Kovács AF, Ghahremani M. Minimization of zygomatic complex fracture treatment. Int J Oral Maxillofac Surg. 2001; 30:380–383. PMID: 11720038.

14. Patil S, Patil RS. Zygomatic arch fracture reduction via Gillie's (temporal) approach—report of 3 cases. Indian J Mednodent Allied Sci. 2014; 2:126–129.

15. Salinas JB, Vira D, David H, Elashoff D, Abemayor E, John MS. Steimann pin repair of zygomatic complex fractures. Int J Otolaryngol Head Neck Surg. 2013; 2:74–78.

16. Rehman AU, Ansari SR, Shah SM, Rehman B. Pattern of zygomatic bone fractures and treatment modalities: a study. Pakistan Oral Dent J. 2010; 30:36–40.
17. Ellis E, Zide M. Surgical approaches to the facial skeleton. 2nd ed. Philadelphia: Lippincott Williams & Wilkins;2006.
18. Fernandes YB, Maitrot D, Kehrli P, Tella OI Jr, Ramina R, Borges G. Supraorbital eyebrow approach to skull base lesions. Arq Neuropsiquiatr. 2002; 60:246–250. PMID: 12068354.

19. Ahamed T, Sundararajan V, Ramanathan S. Management of zygomatic complex fractures with two point fixation. IJSS Case Rep Rev. 2014; 1:25–26.
20. Langsdon PR, Rohman GT, Hixson R, Stumpe MR, Metzinger SE. Upper lid transconjunctival versus transcutaneous approach for fracture repair of the lateral orbital rim. Ann Plast Surg. 2010; 65:52–55. PMID: 20548223.

21. Rajkumar K, Mukhopadhyay P, Sinha R, Bandyopadhyay TK. ‘Y’ Modification of the transconjunctival approach for management of zygomatic complex fractures: a prospective analysis. J Maxillofac Oral Surg. 2016; 15:45–51. PMID: 26929552.

22. Oestreicher J, Mehta S. Complications of blepharoplasty: prevention and management. Plast Surg Int. 2012; 2012:252368. PMID: 22655191.

23. Thangavelu K, Ganesh NS, Kumar JA, Sabitha S, Nikil . Evaluation of the lateral orbital approach in management of zygomatic bone fractures. J Nat Sci Biol Med. 2013; 4:117–121. PMID: 23633846.

24. Ebenezer V, Ramalingam B, Sivakumar M. Treatment of zygomatic complex fractures using two point fixation under general anaesthesia. World J Med Sci. 2014; 10:179–183.
25. Rohrich RJ, Janis JE, Adams WP Jr. Subciliary versus subtarsal approaches to orbitozygomatic fractures. Plast Reconstr Surg. 2003; 111:1708–1714. PMID: 12655219.

26. Habal MB, Chaset RB. Infraciliary transconjunctival approach to the orbital floor for correction of traumatic lesions. Surg Gynecol Obstet. 1974; 139:420–422. PMID: 4604609.

27. Manganello-Souza LC, Rodrigues de Freitas R. Transconjunctival approach to zygomatic and orbital floor fractures. Int J Oral Maxillofac Surg. 1997; 26:31–34. PMID: 9081250.

28. Crosara J, Rosa E, Silva M. Comparison of cutaneous incisions to approach the infraorbital rim and orbital floor. Braz J Oral Sci. 2009; 8:89–91.
29. Holtmann B, Wray RC, Little AG. A randomized comparison of four incisions for orbital fractures. Plast Reconstr Surg. 1981; 67:731–737. PMID: 7243973.

30. Heckler FR, Songcharoen S, Sultani FA. Subciliary incision and skin-muscle eyelid flap for orbital fractures. Ann Plast Surg. 1983; 10:309–313. PMID: 6847091.

31. Bähr W, Bagambisa FB, Schlegel G, Schilli W. Comparison of transcutaneous incisions used for exposure of the infraorbital rim and orbital floor: a retrospective study. Plast Reconstr Surg. 1992; 90:585–591. PMID: 1409993.
32. Netscher DT, Patrinely JR, Peltier M, Polsen C, Thornby J. Transconjunctival versus transcutaneous lower eyelid blepharoplasty: a prospective study. Plast Reconstr Surg. 1995; 96:1053–1060. PMID: 7568479.
33. Giraddi GB, Syed MK. Preseptal transconjunctival vs. subciliary approach in treatment of infraorbital rim and floor fractures. Ann Maxillofac Surg. 2012; 2:136–140. PMID: 23482434.

34. Coronal approach [Internet]. Davos: AO Foundation;2009. 12. 03. cited 2017 Jan 15. Available from: https://goo.gl/SQAHMr.
35. Rajmohan S, Tauro D, Bagulkar B, Vyas A. Coronal/hemicoronal approach: a gateway to craniomaxillofacial region. J Clin Diagn Res. 2015; 9:PC01–PC05.
36. Zhuang QW, Zhang XP, Wang X, Zhang J, Li ZP, Si YM, et al. Coronal approach to zygomaticomaxillary complex fractures. Eur Rev Med Pharmacol Sci. 2015; 19:703–711. PMID: 25807420.
37. Srivastava A, Sharma R, Chandramala R. Versatility of buccal sulcus approach for zygomatic complex fractures. E-J Dent. 2012; 2:46–51.
38. Courtney DJ. Upper buccal sulcus approach to management of fractures of the zygomatic complex: a retrospective study of 50 cases. Br J Oral Maxillofac Surg. 1999; 37:464–466. PMID: 10687908.

39. de Souza Carvalho AC, Pereira CC, Queiroz TP, Magro-Filho O. Intraoral approach to zygomatic fracture: modified technique for infraorbital rim fixation. J Craniofac Surg. 2012; 23:537–538. PMID: 22421848.
40. Kühnel TS, Reichert TE. Trauma of the midface. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2015; 14:Doc06. PMID: 26770280.
41. Dakir A, Muthumani T, Prabu NP, Mohan R, Maity A. One point fixation of zygomatic tripod fractures in the zygomatic buttress through Keen's intraoral approach: a review of 30 cases. J Pharm Bioallied Sci. 2015; 7(Suppl 1):S238–S241. PMID: 26015722.

42. Fujioka M, Yamanoto T, Miyazato O, Nishimura G. Stability of one-plate fixation for zygomatic bone fracture. Plast Reconstr Surg. 2002; 109:817–818. PMID: 11818879.

43. Kim JH, Lee JH, Hong SM, Park CH. The effectiveness of 1-point fixation for zygomaticomaxillary complex fractures. Arch Otolaryngol Head Neck Surg. 2012; 138:828–832. PMID: 22986716.

44. Rana M, Warraich R, Tahir S, Iqbal A, von See C, Eckardt AM, et al. Surgical treatment of zygomatic bone fracture using two points fixation versus three point fixation--a randomised prospective clinical trial. Trials. 2012; 13:36. PMID: 22497773.

45. Bui TG, Bell RB, Dierks EJ. Technological advances in the treatment of facial trauma. Atlas Oral Maxillofac Surg Clin North Am. 2012; 20:81–94. PMID: 22365431.

46. Lee CH, Lee C, Trabulsy PP. Endoscopic-assisted repair of a malar fracture. Ann Plast Surg. 1996; 37:178–183. PMID: 8863979.

Table 1
Elements of the facial buttress
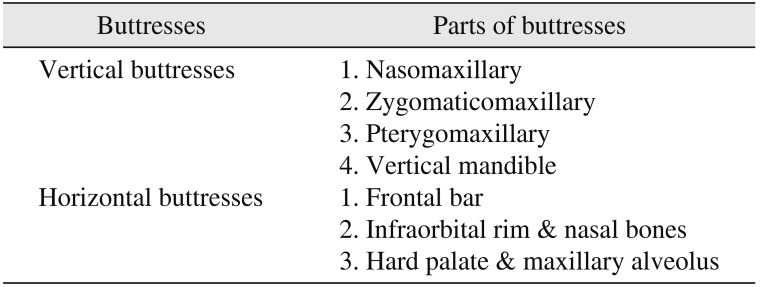
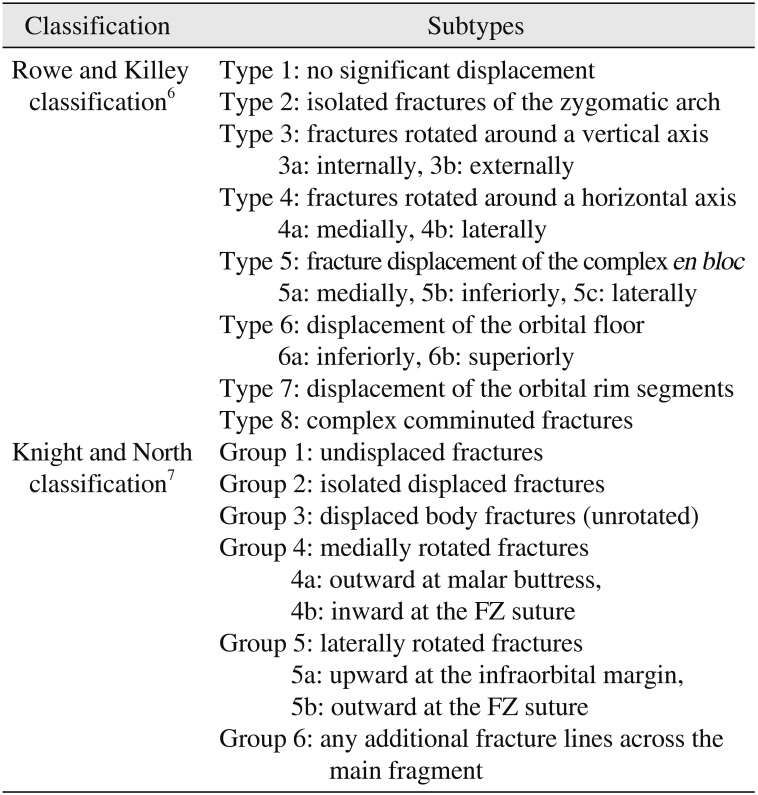
Table 2
Classification of zygomatic fractures
| Classification | Subtypes | |
|---|---|---|
| Rowe and Killey classification6 | Type 1: | no significant displacement |
| Type 2: | isolated fractures of the zygomatic arch | |
| Type 3: | fractures rotated around a vertical axis | |
| 3a: | internally, 3b: externally | |
| Type 4: | fractures rotated around a horizontal axis | |
| 4a: | medially, 4b: laterally | |
| Type 5: | fracture displacement of the complex en bloc | |
| 5a: | medially, 5b: inferiorly, 5c: laterally | |
| Type 6: | displacement of the orbital floor | |
| 6a: | inferiorly, 6b: superiorly | |
| Type 7: | displacement of the orbital rim segments | |
| Type 8: | complex comminuted fractures | |
| Knight and North classification7 | Group 1: | undisplaced fractures |
| Group 2: | isolated displaced fractures | |
| Group 3: | displaced body fractures (unrotated) | |
| Group 4: | medially rotated fractures | |
| 4a: | outward at malar buttress, | |
| 4b: | inward at the FZ suture | |
| Group 5: | laterally rotated fractures | |
| 5a: | upward at the infraorbital margin, | |
| 5b: | outward at the FZ suture | |
| Group 6: | any additional fracture lines across the main fragment main fragment | |
Table 3
Clinical symptoms of zygomatic bone complex fractures
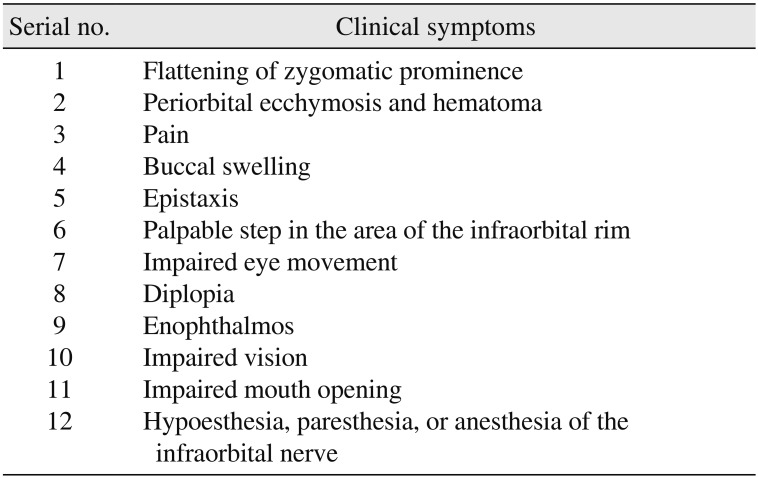
Table 4
Surgical approaches to zygomaticomaxillary complex fractures




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download