Abstract
Perforating granuloma annulare (PGA), a rare variant of granuloma annulare, is characterized by transepidermal elimination of altered collagen that clinically manifests an umbilicated papule with a central crust. It can be confused with papulonecrotic tuberculid (PNT) because of their similar appearance. Unlike PGA, PNT is usually related to tuberculosis infection with a typical histologic finding of wedge-shaped dermal necrosis. Here, we report the first Korean case of PGA mimicking PNT both clinically and histologically. A 43-year-old Korean woman presented with erythematous papules localized on the extensor surface of her limbs for one year. Some of these papules had a central umbilication or a crust. Regarding comorbidity, she had latent tuberculosis diagnosed with QuantiFERON®-TB Gold test about five months ago. She was on antituberculous medication. Initially, a diagnosis of papulonecrotic tuberculid accompanied by latent tuberculosis was considered. However, despite taking the antituberculous medication for five months, her skin lesions were not improved. Biopsy specimen from her arm lesion showed wedge-shaped area of necrosis in the dermis. Additionally, there were multiple focal mucin depositions and palisading granulomatous inflammation throughout the dermis. A diagnosis of PGA was made and she was treated with topical corticosteroid. After two weeks of applying topical corticosteroid, most of her skin lesions disappeared, leaving some hyperpigmented scars.
Granuloma annulare (GA) is an idiopathic granulomatous condition characterized by a set of morphologic variants, including perforating GA (PGA) that shows unique clinical and histological features1. Papulonecrotic tuberculid (PNT) is thought to represent a cutaneous immunologic reaction to Mycobacterium tuberculosis2. Both PGA and PNT share similar appearance characterized by erythematous papules with an umbilicated necrotic center. They commonly have predilection for extremities23.
Distinguishing these two conditions is imperative because antituberculous medication is the mainstay of treatment for PNT. However, it is generally an ineffective and unnecessary treatment for patients with PGA4. Clinically, PNT is usually associated with tuberculosis infection, unlike PGA. Histologically, it shows a typical wedge-shaped necrotic area in the dermis2.
PGA is a rare subtype of GA. Only 7 cases of PGA have been previously reported in the Korean literature567891011. However, none of them has a histologic finding of wedge-shaped dermal necrosis mimicking PNT. Herein, we report the first Korean case of PGA mimicking PNT both clinically and histologically.
A 43-year-old female had a 1-year history of erythematous papules with crusts on her extensor surface of extremities. She said that some papules developed to pustules, later leaving a central crust or ulceration. At first, these papules were diagnosed as folliculitis at a private clinic. They were treated with several antibiotics without any sign of improvement. Regarding comorbidity, she had latent tuberculosis diagnosed with QuantiFERON®-TB Gold (Cellestis Limited, Carnegie, VIC, Australia) test about five months ago. She was on antituberculous medication (isoniazid). Physical examination revealed 3~5 mm sized numerous erythematous to brownish papules on the extensor surface of her limbs. Some of these papules had a central umbilication or crust (Fig. 1). Laboratory findings including complete blood count, liver, and renal function tests yielded normal results. Chest X-ray showed no abnormality. Initially, a diagnosis of papulonecrotic tuberculid accompanied by latent tuberculosis was considered. However, despite taking antituberculous medication for five months, new skin lesions continuously appeared while existing ones did not improve. To confirm the diagnosis, skin biopsy was done for a centrally crusted papule on the arm and an umbilicated papule on the lower leg. Histologically, the arm lesion showed a wedge-shaped area of necrosis in the upper dermis composed of altered collagen fibers based on Masson's trichrome staining (Fig. 2A, B). Focal mucin deposition surrounded by palisades of histiocytes near the wedge-shaped area of dermal necrosis was revealed (Fig. 2C, D). Special stains for acid-fast bacilli and polymerase chain reaction (PCR) for Mycobacterium tuberculosis were all negative. Specimen from the lower leg lesion showed increased mucin coupled with collection of histiocytes intercalated between collagen bundles in the lower dermis (Fig. 3A, B). Based on these findings, a diagnosis of PGA was made and she was treated with topical corticosteroid. After two weeks of applying topical corticosteroid, most of her skin lesions disappeared, leaving some hyperpigmented scars.
PGA is a rare subtype of GA named by Owens and Freeman12 in 1971. The precise etiology of PGA has been poorly understood. Clinically, PGA is usually present as umbilicated papules with a central crust. Some authors have noted that there are four stages in the progression of PGA3: (1) erythematous papules that evolve into (2) yellowish, pustular-appearing lesions that discharge a clear fluid. Later, they develop (3) a central umbilication or a small crust, and then (4) regress, leaving a punctate scar. It can be either localized to dorsal hands and fingers or generalized over the trunk and extremities.
PGA shows typical histologic findings of epidermal perforation and transepidermal elimination of altered collagen. Penas et al.4 have suggested that superficial localization of necrobiotic granuloma and subsequent vasculopathy could lead to ischemic epidermal alterations, resulting in epidermal destruction. In our case, the arm lesion showed numerous necrobiotic granulomas scattered throughout the whole dermis. The granuloma itself and ischemic alteration caused by the granuloma might have created the distinctive wedge-shaped dermal necrosis.
PGA can be confused with PNT because of their similar appearance and common predilection for extremities23. PNT is usually associated with tuberculosis infection. It shows a typical wedge-shaped necrotic area in the dermis2. However, in our patient, all these aforementioned features of PNT were seen. It was the first disease that had to be distinguished. The pathogenesis of PNT has been explained by immunologic reactions to mycobacterial products that cause initial vascular endothelial damage2. As a result of vasculopathy, the typical wedge-shaped necrotic area of the dermis is made13. Therefore, PNT shows good response to antituberculous therapy213. However, our patient did not show any improvement while taking the antituberculous medication for five months, indicating that tuberculosis was not related to its pathogenesis. It was just a coincidental finding. In addition, specimen from the arm lesion failed to show other supportive histologic findings favoring the diagnosis of PNT such as thrombotic occlusion or fibrinoid necrosis in dermal vessels13. There were multiple focal mucin depositions and palisading granulomatous inflammation near the wedge-shaped dermal necrotic area that favored the diagnosis of PGA. The negative result in PCR for Mycobacterium tuberculosis also helped us rule out the diagnosis of PNT. Unfortunately, tissue culture was not done due to the scarce amount of tissue obtained from skin biopsy and the relative fast response to topical corticosteroid.
To the best of our knowledge, there are two cases of PGA mimicking PNT clinically or histologically (Table 1)1415. One case of PGA is associated with lymph node tuberculosis infection14. In that case, the diagnosis of PGA was not difficult because typical histologic findings of PGA were seen. However, the patient's skin lesions were improved after just one week of antituberculous therapy, unlike our case. In this regard, the authors speculated that the patient's PGA was caused by an immune reaction to the systemic infection (tuberculosis). The other is a case of PGA occurred on a patient with a history of healed pulmonary tuberculosis15. The patient's skin biopsy specimen showed wedge-shaped area of necrosis in the upper dermis with granulomatous inflammation. At first, the diagnosis of PNT was made and the patient was treated with antituberculous medication for nine months. However, the patient's skin condition was not improved, like our case. After a series of re-biopsies, transepidermal elimination of degenerated collagen and small focus of necrobiotic granuloma with palisading of histiocytes were found and the diagnosis was revised as PGA. The patient was treated with topical corticosteroid, showing good response. As shown in our case and Yu's case15, careful review of biopsy specimen is needed for correct diagnosis of PGA.
Other differential diagnosis of PGA includes reactive perforating collagenosis, insect bite, pityriasis lichenoides et varioliformis acuta (PLEVA), and molluscum contagiosum. Reactive perforating collagenosis frequently occurs early in life. Histologically, vertically oriented basophilic collagen bundles are seen. Palisading granuloma is not a feature16. Others can be ruled out easily by their typical clinical and histological findings.
Generally, most cases of PGA will resolve spontaneously without treatment. Topical and intralesional corticosteroids could be considered for localized disease4. For generalized severe forms, other treatments such as antimalarial drugs, ultraviolet light, and systemic retinoid have been proposed with variable success4.
Our case illustrates that PGA can appear both clinically and histologically similar to PNT. In tuberculosis-endemic countries like Korea, tuberculosis infection can be accompanied by chance in PGA patients. It may mimic PNT. More attention should be paid for correct diagnosis, thus avoiding unnecessary treatment.
References
1. Piette EW, Rosenbach M. Granuloma annulare: clinical and histologic variants, epidemiology, and genetics. J Am Acad Dermatol. 2016; 75:457–465. PMID: 27543209.
2. Tirumalae R, Yeliur IK, Antony M, George G, Kenneth J. Papulonecrotic tuberculid-clinicopathologic and molecular features of 12 Indian patients. Dermatol Pract Concept. 2014; 4:17–22. PMID: 24855568.

3. Samlaska CP, Sandberg GD, Maggio KL, Sakas EL. Generalized perforating granuloma annulare. J Am Acad Dermatol. 1992; 27:319–322. PMID: 1517496.

4. Penas PF, Jones-Caballero M, Fraga J, Sánchez-Pérez J, García-Díez A. Perforating granuloma annulare. Int J Dermatol. 1997; 36:340–348. PMID: 9199980.

5. Seong YK, Cho KH, Kim SH, Lee YS. A case of perforating granuloma annulare. Korean J Dermatol. 1986; 24:678–681.
6. Hong KT, Lee KH, Park CI. A case of generalized perforating granuloma annulare. Korean J Dermatol. 1988; 26:560–564.
7. Lee JD, Yi JY, Cho BK, Houh W. Anetoderma due to generalized perforating granuloma annulare. Ann Dermatol. 1990; 2:96–99.

8. Yoon SY, Kim KH, Suhr KB, Park JK. A case of generalized granuloma annulare with perforating and subcutaneous granuloma annulare. Korean J Dermatol. 1995; 33:1119–1123.
9. Lee SY, Han KP, Choi KC, Kim YK. A case of disseminated perforating granuloma annulare in a child. Ann Dermatol. 1996; 8:223–226.

10. Lee SW, Lee IW, Lee YS, Lee SC. Generalized perforating granuloma annulare. Korean J Dermatol. 2000; 38:1248–1249.
11. Koh BK, Park CJ, Yi JY, Cho BK. A case of generalized perforating granuloma annulare with diabetes mellitus. Korean J Dermatol. 2001; 39:491–493.
12. Owens DW, Freeman RG. Perforating granuloma annulare. Arch Dermatol. 1971; 103:64–67. PMID: 5539506.

13. Wilson-Jones E, Winkelmann RK. Papulonecrotic tuberculid: a neglected disease in Western countries. J Am Acad Dermatol. 1986; 14:815–826. PMID: 3711385.

14. Pereira AR, Vieira MB, Monteiro MP, Enokihara MM, Michalany NS, Bagatin E, et al. Perforating granuloma annulare mimicking papulonecrotic tuberculid. An Bras Dermatol. 2013; 88(6 Suppl 1):101–104. PMID: 24346892.

15. Yu JC, Lee KC. Generalised perforating granuloma annulare mimicking papulonecrotic tuberculid. Hong Kong J Dermatol Venereol. 2006; 14:139–142.
16. Woo TY, Rasmussen JE. Disorders of transepidermal elimination. Part 2. Int J Dermatol. 1985; 24:337–348. PMID: 3899955.
Fig. 1
About 3~5 mm sized, numerous erythematous to brownish colored papules on the extensor surface of limbs. Closer view of the papule shows an umbilication (arrow) and a central crust (empty arrow). We received the patient's consent form about publishing all photographic materials.

Fig. 2
(A) Wedge-shaped area of necrosis in the upper dermis surrounded by perivascular lymphohistiocytic infiltration (H&E, ×40). (B) The necrotic area is consisted of altered collagen fibers (Masson's trichrome staining, ×40). (C, D) Focal mucin deposition surrounded by palisades of histiocytes near the wedge-shaped dermal necrosis (C: H&E, ×100, D: Alcian blue at pH 2.5, ×100).
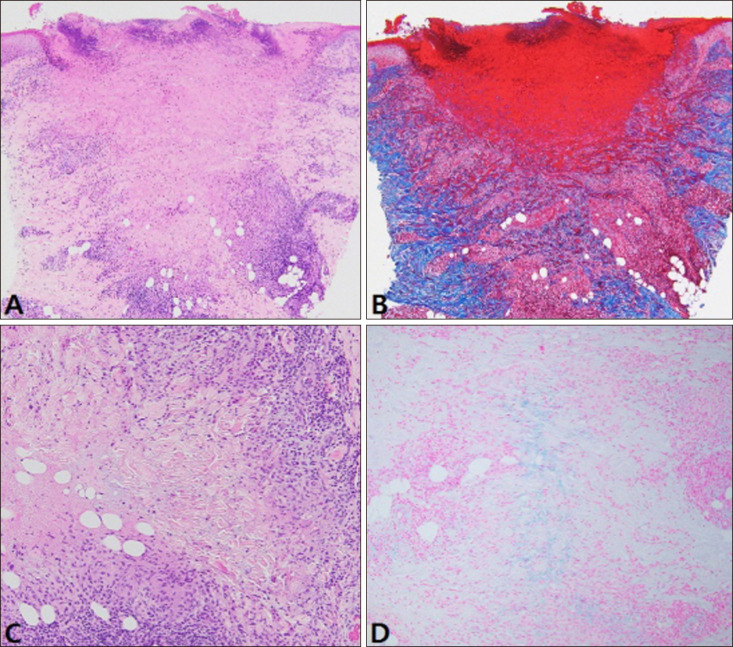
Fig. 3
(A, B) Increased mucin coupled with collection of histiocytes intercalated between collagen bundles in the lower dermis (A: H&E, ×100, B: Alcian blue at pH 2.5, ×100).
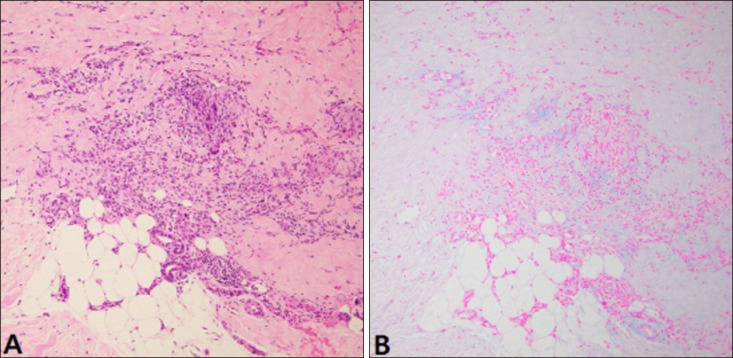
Table 1
Previously reported cases of PGA mimicking PNT
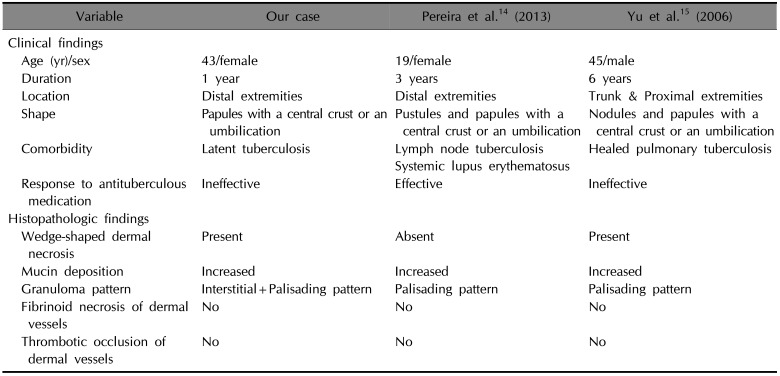
| Variable | Our case | Pereira et al.14 (2013) | Yu et al.15 (2006) |
|---|---|---|---|
| Clinical findings | |||
| Age (yr)/sex | 43/female | 19/female | 45/male |
| Duration | 1 year | 3 years | 6 years |
| Location | Distal extremities | Distal extremities | Trunk & Proximal extremities |
| Shape | Papules with a central crust or an umbilication | Pustules and papules with a central crust or an umbilication | Nodules and papules with a central crust or an umbilication |
| Comorbidity | Latent tuberculosis | Lymph node tuberculosis Systemic lupus erythematosus | Healed pulmonary tuberculosis |
| Response to antituberculous medication | Ineffective | Effective | Ineffective |
| Histopathologic findings | |||
| Wedge-shaped dermal necrosis | Present | Absent | Present |
| Mucin deposition | Increased | Increased | Increased |
| Granuloma pattern | Interstitial+Palisading pattern | Palisading pattern | Palisading pattern |
| Fibrinoid necrosis of dermal vessels | No | No | No |
| Thrombotic occlusion of dermal vessels | No | No | No |




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download