Abstract
Background
Psychological stress is an important factor of acne pathogenesis. Stress related production of hormones, cytokines and neuropeptides may result in the chronic course and exacerbations of the disease.
Objective
The aim of the study was to evaluate the relationship between acne severity, intensity of emotional stress and serum concentration of substance P (scSP), to compare the intensity of adversities, psychological stress and scSP in acne patients with healthy controls and to compare coping techniques for stress.
Methods
The study consisted of 80 patients. Emotional stress was analyzed with the use of social readjustment rating scale, whereas the methods of coping with stress were assessed with the coping inventory for stressful situation questionnaire. The blood concentration of substance P was analyzed by enzyme-linked immunosorbent assay method in a group of 40 patients with acne vulgaris and in control subjects.
Results
There was no statistically significant difference between the severity of acne and the intensity of stress. Acne patients presented a higher average scSP than the controls. No statistically significant correlation was observed between the severity of acne and scSP; however, the intensity of stress correlated with scSP in the control group. The evaluation of methods of coping with stress showed significantly higher rate for the avoidance-oriented coping among acne patients.
Patients suffering from skin diseases are often affected by a variety of psychopathologic problems such as depression, anxiety, disorders of self-image, distortion of body image, behavioral problems, and low self-esteem123. These conditions occur in about 30%~60% of dermatological patients, significantly more often than the general population, and might have their source in a complex interplay that takes place between the skin and neuroendocrine and immune systems234. The risk of depressive symptoms or suicidal thoughts increases particularly in case of chronic dermatoses and lesions located on the visible parts of the body, especially involving the face. Also clinically mild and moderate severity skin lesions may be associated with significant suicidal ideation35. The close interaction between the skin and the mind is revealed in chronic and cosmetically disfiguring lesions in the course of atopic dermatitis, psoriasis, alopecia areata, acne vulgaris, and vitiligo146.
Thus, broader diagnostic approach should be used to evaluate exacerbating factors in order to design comprehensive treatment plan for various skin diseases. Attention should be paid to the psychological condition and behavioral challenges of patients and, in cases when it seems appropriate, attempts should be made to arrange psychological and psychiatric consultations for the affected individuals. Current treatment of psychocutaneous disorders requires holistic therapy. Depending on the nature of the underlying psychopathology, psychological methods and psychotropic agents should be applied together with dermatologic treatment. Psychological stress is an exacerbating factor for inflammatory cutaneous diseases such as atopic dermatitis, psoriasis and acne46. Acne vulgaris is believed to affect 85%~100% of the population, at various ages and stages of life78. Acne lesions occur often in adolescents and adults and negatively influence the quality of their life, especially in women89. Numerous reports on higher prevalence of emotional disturbances and psychiatric comorbidities in female patients with skin conditions have been reported. The chronic course of the disease is associated with stress-related production of adrenal hormones and neuropeptides Propionibacterium acnes colonization and genetic factors10.
Various studies proved that the inflammatory process within the pilosebaceous unit is modulated by neuropeptides, especially substance P but serum concentration in acne patients was not evaluated1112. Chronic psychological stress is an important pathogenic factor of acne10. Difficulties with expressing emotions, especially stress and conflicts, play a significant role as well. Attempts of an individual to overcome stress and its consequences are defined as coping with stress. The aims of the study were: to evaluate the relationship between acne severity and intensity of emotional stress and scSP, to compare the intensity of adversities and psychological stress and scSP in acne patients and healthy controls and to compare stress coping techniques in both groups.
The study included 80 patients (22 men and 58 women), aged 18~34 years (mean 24.4±5.7) suffering from acne, recruited prospectively from the dermatology out-patient clinic of the hospital of the Ministry of Interior Affairs in Poznan between 2009~2012. These patients were generally in good health and did not use any medications for 6 months before the study, were not treated for acne before presentation and were healthy otherwise. Participants were graded on their acne severity using the investigator's global assessment (IGA) scale presented in Table 11314. The control group consisted of 40 healthy volunteers (18 men and 22 women), aged 20~34 years (mean 25.7±3.9). Emotional stress was analyzed with the use of the social readjustment rating scale (SRRS) by Holmes and Rahe15, which consists of 43 stressful life events (over the last 12 months) that could have contributed to the illness, with relative impact expressed in life change unit on a scale from 1 to 100. Coping inventory for stressful situation (CISS) questionnaire was used to assess the coping styles for stress16. The subjects assessed the frequency of their activities undertaken in stressful, difficult situations on a 5-point scale. The CISS questionnaire measures three dimensions of coping: task-oriented coping, emotion-oriented coping, and avoidance-oriented coping (AOC) with two subscales: distraction and social diversion. The questionnaire, being a standardized tool, meets the psychometric criteria of the investigating tools. ScSP was examined using the enzyme-linked immunosorbent assay (ELISA, substance P Assay Kit; R&D Systems, Minneapolis, MN, USA) in a group of 40 patients with acne and controls. The results were analyzed statistically with the use of IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA). The statistical analysis was completed using ANOVA and independent sample t-test. Before performing analysis assumptions were checked. Normality of data was analyzed with Kolmogorov-Smirnov test and equality of variances was checked by Levene's test. In case ANOVA has shown significant differences additionally Tukey's post-hoc tests were performed. The level of statistical significance was estimated at p≤0.05. The study was approved by the Ethics Committee of Poznan University of Medical Sciences (No. 547/09, 18 Jun 2009). Written informed consent from all subjects was obtained.
The severity of acne vulgaris in the study group is presented in Table 1. The analysis of emotional stress with respect to acne severity showed no statistically significant difference (p=0.143) (Fig. 1). No difference was found in average scores of SRRS in both groups: acne subjects and controls (Fig. 1). Acne patients presented a higher average scSP than controls: 0.6±0.09 vs. 0.49±0.12 (p<0.001). Analysis of acne patients showed no statistically significant differences in scSP level (p=0.611) (Fig. 2). As illustrated on Fig. 3. scSP was differed depending on stress intensity in the control group (p=0.026). No significant differences were found among acne patients. The comparison between control and acne patients showed significant differences in two subgroups of stress intensity: <149 SRRS 0.46±0.11 vs. 0.59±0.12 (p<0.001) and 200~299 SRRS 0.43±0.09 vs. 0.59±0.09 (p=0.019). Evaluation of stress-coping styles showed a significantly higher rate for the AOC among acne patients (p=0.037) (Fig. 4), whereas task-oriented and emotion-oriented coping did not differ significantly and were similar in both groups.
Acne vulgaris is the most common inflammatory skin disease of multifactorial pathogenesis. Increased sebum production, excessive and abnormal follicular hyperkeratinization is responsible for the development of microcomedones and proliferation of P. acnes within the follicle. The subsequent release of pro-inflammatory mediators in the skin millieau is thought to play the most significant role in the process of lesion formation10. The activity of sebaceous glands is regulated by a multitude of hormonal and nerve factors11. Contrary to popular belief, the course of acne is unpredictable, frustrating and often chronic. Persisting acne lesions are increasingly observed and reported in adults11. This chronic skin disorder induces negative psychological and social effects such as anxiety, decreased self-esteem, depression, suicidal ideation and reduction in social functioning5. It negatively affects the quality of life and the psychological consequences of the disease are usually present for many years, even after a successful therapy. On the other hand, the presence of acne-induced psychological problems which may increase stress level, is an indication for psychological and psychiatric evaluations. The psychological and psychiatric interventions should constitute an integral part of comprehensive treatment plan in qualifying individuals who present with this frequently difficult to treat condition. Stress, the key pathogenic element in the development of numerous dermatoses, remains the essential factor inducing or exacerbating preexisting acne. Immune system is affected by stress via neuropeptide receptors and release cytokines that affect central nervous system. Chronic psychological stress increases adrenal androgen secretion, stimulates cytokine production, causes growth and increases activity of the sebaceous glands, thus exacerbating acne. In recent years, our knowledge of the role of neuropeptides in the pathogenesis of chronic skin diseases, including acne vulgaris, has expanded. The prevalence of acne in adults is increasing and 80% of post-adolescent acne cases are persistent acne9. The majority of adult acne patients are female. Among these patients psychological stress seems to be the crucial factor inducing or exacerbating acne lesions7. Even mild and moderate forms of acne may be related to severe stress and may negatively affect the quality of life and emotional well-being of patients8. In our study, the majority of subjects suffered from mild to moderate acne. Nevertheless, no correlation between the acne severity and stress measured with the SRRS questionnaire was noted. The activity of the pilosebaceous unit is regulated by numerous hormones, medications, neurohormones, neuropeptides, growth factors and cytokines411. Incubation of sebaceous glands in a culture medium with selected neuropeptides such as substance P, vasoactive intestinal peptide, neuropeptide Y, calcitonin gene-related peptide revealed that only substance P affected the structure of sebaceous glands and that the effect was dose-dependent12. The release of neuropeptides is elicited by stress. Thus, all stressful events and life situations may lead to the development of an inflammatory process by stimulating the release of neuropeptides. In our study, acne patients turned out to have a higher mean concentration of substance P in comparison to controls, but no correlation was found between the clinical state and serum concentration of this neuropeptide. Even mild or moderate acne is a chronic disease, unpredictable and cosmetically disfiguring the face. As such, it often induces the feelings of low self-esteem, negative image of self, fear, depression, mood swings, suicidal thoughts and tendencies, obsessions, and delusions. Psychological factors, mostly the mechanisms of processing of emotions in stress, are the key factor responsible for exacerbation of acne skin lesions. The pilosebaceous unit works as an endocrinally independent organ and is the control center for a complex neuropeptide regulatory program which functions under control of hypothalamic-pituitary-adrenal (HPA) axis11. Healthy human skin produces various neuropeptides, released directly from the sensory neurons as well as skin cells and migratory cells appearing in the course of an inflammatory process. The connection between neuropeptide secretion during the period of emotional stress and the development of dermal inflammation results in exacerbation of such dermatological conditions as atopic dermatitis, psoriasis and alopecia areata4. Facial skin of acne patients is characterized by richer innervation, increased number of substance P-containing nerve endings and mast cells, and stronger expression of neutral endopeptidase in sebaceous glands and E-selectin in venules around pilosebaceous glands in comparison to healthy, unaffected skin12. Substance P induces, both directly and indirectly, inflammation by modulating the release of proinflammatory cytokines and chemokines (also in the skin). This neuropeptide affects the activity of the pilosebaceous unit by stimulating proliferation and differentiation of sebaceous glands, lipid synthesis and induction of neutral endopeptidase expression in sebaceous cells and of E-selectin in perifollicular vessels11. Substance P stimulates mast cell proliferation, degranulation and release of proinflammatory cytokines, among others: interleukin (IL)-1, IL-2 and tumor necrosis factor-α. It has chemotactic effect on monocytes, lymphocytes T and neutrophils1012. Thus, it seems plausible to investigate the correlation between serum concentration of substance P and acne severity. Current studies have demonstrated a strong association between psychological stress, high-fat diet, intestinal microflora, release of substance P, dermatological state and gastrointestinal disorders17. Toyoda and Morohashi18 proved that substance P, which can be elicited by stress, promoted the development of cytoplasmic organelles in sebaceous cells, stimulated sebaceous germinative cells, and induced significant increases in the area of sebaceous glands. It also increased the size of individual sebaceous cells and the number of sebum vacuoles for each differentiated sebaceous cell, all of which suggests that substance P promotes both the proliferation and the differentiation of sebaceous glands. Our study showed the higher serum concentration of substance P in acne patients in comparison with healthy subjects Emotional stress may affect the intestinal microflora and increase intestinal permeability, what in consequence leads to systemic inflammation in the body. Probiotics found in food, oxidative stress, regulation of carbohydrate and lipid distribution and even mood play an important role in the etiopathogenesis of acne17. Probiotics influence the release of substance P in the intestinal tract and the skin17. Even minute and short-term elevation in circulating substance P may lead to anxiety, depression and aggression17. Our study used the 4-point IGA scale, which correlates with one of the most commonly used scales for the assessment of acne intensity, i.e., the Leeds scale, currently recommended by the Food and Drug Administration. It is especially applicable in everyday clinical practice as it requires neither lesion count nor photographic records and allows for a speedy and objective assessment of the severity of the disease. The system, proposed by Allen and Smith Jr, is based on a descriptive text, not on photographs, and demonstrates a higher level of correlation when compared with the Leeds Revised Acne Grading System1314. Psychodermatology has proposed a classification of disorders of skin conditions associated with mental status by dividing them into four groups: psychophysiologic, primary psychiatric, secondary psychiatric and cutaneous sensory disorders. The effect of emotional stress on acne has been described as the psychophysiologic disorder by Arck et al.4. Acne may result in feelings of anxiety, anger and depression, which can worsen if there is no response to acne treatment. Both, mild and moderate acne can be associated with significant depression and suicidal ideation which might even require psychiatric intervention78. The psychological evaluation was performed with the use of two questionnaires evaluating the intensity of stress: the Holmes and Rahe's list15 of stressful life events and coping styles for stress (CISS questionnaire). According to the evolutionary standards, stress is defined as a collection of physiological adaptive processes which are the basis for all negative emotions. Regardless, the process is mostly biological even if its causative factors are psychological in nature. Stressors encompass acute and chronic changes, as well as sequences of stressors. Reactivity of the HPA axis is especially high in case of psychological stressors. The four aspects of stress: the stimuli for stress (stressors), subjective experience of stress by a subject, non-specific increased agitation (i.e., activation which is a stressful reaction) and its experience by the subject. Attempts of an individual to overcome stress and its consequences are called coping with stress. In most challenging situations human beings apply various techniques of coping with stress simultaneously. Resources that facilitate stress coping include individual features, positive perception of self and the world, available social support, group norms and financial means. Our analysis of coping styles revealed significantly higher scores for stress avoidance strategies in acne patients when compared to healthy controls, while other styles did not significantly differ from the general population mean, what might indicate ineffectiveness of coping strategies for stress in people with chronic acne lesions. The analysis of stressful events based on the SRRS questionnaire revealed that number of stressful events is not a factor that determines the severity of acne. Studies incorporating personality features are necessary to clarify this problem.
Figures and Tables
Fig. 1
The comparison of the intensity of stress expressed in life change unit with the use of social readjustment rating scale in acne patients and healthy volunteers.

Fig. 3
The comparison of the intensity of stress expressed in life change unit with the use of social readjustment rating scale (SRRS) and substance P serum concentration in the studied group. A, b groups followed by the same letter do not differ statistically significantly.
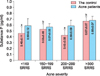
Fig. 4
The avoidance-oriented coping (AOC) with stress assessed with the use of coping inventory for stressful situation (CISS) in studied groups.

Table 1
The intensity of acne in the studied group assessed with the use of investigator's global assessment scale (n=80)

ACKNOWLEDGMENT
The study was financially supported by the grant from Poznan University of Medical Sciences, no 502-14-04402. All authors declare no conflict of interest.
References
1. Jafferany M. Psychodermatology: a guide to understanding common psychocutaneous disorders. Prim Care Companion J Clin Psychiatry. 2007; 9:203–213.
2. Halvorsen JA, Stern RS, Dalgard F, Thoresen M, Bjertness E, Lien L. Suicidal ideation, mental health problems, and social impairment are increased in adolescents with acne: a population-based study. J Invest Dermatol. 2011; 131:363–370.

4. Arck PC, Slominski A, Theoharides TC, Peters EM, Paus R. Neuroimmunology of stress: skin takes center stage. J Invest Dermatol. 2006; 126:1697–1704.

6. Liezmann C, Klapp B, Peters EM. Stress, atopy and allergy: a re-evaluation from a psychoneuroimmunologic persepective. Dermatoendocrinol. 2011; 3:37–40.
7. Lasek RJ, Chren MM. Acne vulgaris and the quality of life of adult dermatology patients. Arch Dermatol. 1998; 134:454–458.

8. Jones-Caballero M, Chren MM, Soler B, Pedrosa E, Peñas PF. Quality of life in mild to moderate acne: relationship to clinical severity and factors influencing change with treatment. J Eur Acad Dermatol Venereol. 2007; 21:219–226.

9. Khunger N, Kumar C. A clinico-epidemiological study of adult acne: is it different from adolescent acne? Indian J Dermatol Venereol Leprol. 2012; 78:335–341.

10. Zouboulis CC. Modern aspects of acne pathogenesis. J Dtsch Dermatol Ges. 2010; 8:Suppl 1. S7–S14.
11. Makrantonaki E, Ganceviciene R, Zouboulis C. An update on the role of the sebaceous gland in the pathogenesis of acne. Dermatoendocrinol. 2011; 3:41–49.

12. Lee WJ, Jung HD, Lee HJ, Kim BS, Lee SJ, Kim DW. Influence of substance-P on cultured sebocytes. Arch Dermatol Res. 2008; 300:311–316.

13. Tan JK, Tang J, Fung K, Gupta AK, Thomas DR, Sapra S, et al. Development and validation of a comprehensive acne severity scale. J Cutan Med Surg. 2007; 11:211–216.

14. Ramli R, Malik AS, Hani AF, Jamil A. Acne analysis, grading and computational assessment methods: an overview. Skin Res Technol. 2012; 18:1–14.

16. Endler NS, Parker JD. Multidimensional assessment of coping: a critical evaluation. J Pers Soc Psychol. 1990; 58:844–854.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download