Abstract
Purpose
Although many patients with hepatocellular carcinoma experience recurrence within 2 years after hepatectomy, some patients with T1 and T2 hepatocellular carcinoma show recurrence-free survival for more than 5 years after surgery. This study was designed to analyze the optimal follow-up period on patients with T1 and T2 hepatocellular carcinoma (HCC) showing recurrence-free survival 5 years after surgery.
Methods
One hundred seventy patients underwent hepatectomy from January 1995 to December 1999. Numbers of patients with T1 and T2 HCC were 76 and 73, respectively. The recurrence patterns of patients experiencing recurrence more than 5 years after liver resection were analyzed in aspect of clinicopathological features and follow-up period.
Results
Thirteen patients experienced recurrence more than 5 years after surgery. Only age was found as a significant factor for recurrence. Eight patients were checked regularly with 6-month intervals and the others were checked with 12-month or more intervals. The size of the recurrent tumors in the 6-month interval group had a median of 1.1 cm (range, 1 to 4.2 cm) and the size of the recurrent tumors in the 12-month or more interval group had a median of 3 cm (range, 1.6 to 4 cm). The tumor size was significantly smaller in the 6-month interval group.
Conclusion
Though the patients with early stage HCC showed high overall survival, some patients experienced a late recurrence of more than 5 years after surgery. Patients less than 60 years old with early stage HCC should be checked regularly with 6-month intervals even over 5 years after liver resection.
Hepatocellular carcinoma (HCC) is a very common disease in Korea as well as throughout the world. Several guidelines recommend treatment strategies [1-3]. Liver resection has been recognized as a curative treatment modality of HCC. Mortality after liver resection has dramatically decreased due to improved understanding of liver anatomy, surgical and anesthetic technique and patient selection [4-7]. Recent mortality rates after liver resection is less than 5% and liver resection is usually accepted as a safe treatment modality for HCC [4,8,9]. However, the number of patients who can receive liver resection is still limited since it is impossible to operate on patients with advanced staged HCC or poor liver function [10].
The Barcelona-Clinic Liver Cancer staging system recommends liver resection on only very early stage HCC [1]. The Asia Pacific Association for the Study of the Liver recommends liver resection on solitary or multifocal HCC confined to the liver, anatomically resectable, and with satisfactory liver function reserve [3]. Additionally, those guidelines recommend surveillance for HCC by ultrasonography and α-fetoprotein (AFP) every 6 months in patients with high risk of HCC development [1-3]. A surveillance program is important in detecting HCC early in high risk patients. As a result of surveillance, the rate of detection for early stage HCC has been increased to 5-10% of patients in the West and 30% in Japan [1]. Recent data show that the 5-year overall survival rate of patients with early stage HCC is similar between liver resection and liver transplantation, which is both around 80% [11-13]. Among those patients, some showed no recurrence during the follow-up term, which was longer than 5 years after liver resection. But others experienced their first recurrence more than 5 years after liver resection.
However, there is still a debate about the optimal follow-up interval in patients having recurrence-free survival of more than 5 years after liver resection. We investigated the correlation between the follow-up interval and clinicopathological features and the recurrence patterns in patients having recurrence-free survival of more than 5 years after liver resection.
One hundred seventy patients with HCC underwent liver resection with curative intent between January 1995 and December 1999. Among them, the numbers of patients with T1 and T2 stage HCC were 76 and 73, respectively according to the 7th American Joint Committee on Cancer (AJCC) staging system. We retrospectively reviewed the medical records of those patients with T1 and T2 HCC.
Preoperatively, all patients were evaluated by AFP and at least two image modalities. Functional reserve capacity of liver was checked by indocyanine retention rate at 15 minutes (ICG R15). The extent of liver resection was decided according to the liver function and correlation between tumor and vascular structure.
Preoperatively, all patients were regularly checked for tumor recurrence by AFP and computer tomographic (CT) scan every 3 months during the first 2 years. Then, AFP and CT scans were regularly performed every 6 months in patients without recurrence. If the elevation of AFP level or suspicious nodule on CT was shown, further evaluation was conducted by magnetic resonance imaging for intrahepatic lesions and positron emission tomography CT scan for extrahepatic lesions. Repeat resection, ablation therapy, transcatheter arterial chemoembolization or salvage liver transplantation was performed according to the extensiveness of tumor and liver function. In my institute, however, there is no protocol about the optimal follow-up interval for patients who are free from recurrence for more than 5 years after liver resection as of yet.
We assessed the time that recurrence developed after liver resection and identified the patients whose recurrence developed after more than 5 years after liver resection, which is defined as late recurrence in this paper. To determine risk factors for late recurrence, clinicopathological characteristics including age, gender, tumor marker, size, ICG R15, operation type, vascular invasion, and satellite nodule were analyzed. In addition, we specifically focused on the difference in HCC recurrence patterns by follow-up interval.
Statistical analysis was performed using SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA). All continuous variables are presented as a median (range) and all categorical variables as a number (percentage).
Disease-free survival (DFS) rate was calculated by the Kaplan-Meier method. Comparison between patients with recurrence and without recurrence was performed by logistic regression analysis. When the difference of variables was compared between the different follow-up intervals, the Mann-Whitney ranked sum test was used for continuous variables and the Fisher exact test for categorical variables. Statistical significance was defined as P-value < 0.05.
One hundred forty-nine patients with T1 or T2 HCC underwent liver resection with curative intent. Baseline characteristics of patients are presented in Table 1. Seventy-six patients were diagnosed as T1 stage and 73 patients as T2 stage. Sixty-nine patients underwent major liver resection and 72 patients had vascular invasion.
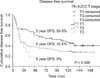
Five-year DFS rates of patients with T1 and T2 stage were 55.8% and 35.4%, respectively (Fig. 1). Ninety-one patients experienced recurrence within 5 years after liver resection. Thirty-four patients with T1 stage and 24 patients with T2 stage showed recurrence-free survival for more than 5 years after liver resection. Among them, eight patients with T1 and 5 patients with T2 stage had recurrence more than 5 years after liver resection.
We compared the clinicopathological characteristics between patients with recurrence and without recurrence at more than 5 years after liver resection. The results are presented in Table 2. Functional reserve capacity of liver and pathological characteristics did not show a significant difference between the two groups. Only age of more than 60 years was found as a significant prognostic factor (hazard ratio, 0.2; P = 0.03).
Among thirteen patients with recurrence more than 5 years after liver resection, 8 patients were regularly checked with 6-month intervals and 5 patients were checked with 12-month intervals. The median tumor size showed significant difference (P = 0.045) between the 6-month follow-up group (1.1 cm) and the 12-month follow-up group (3 cm). Preoperative clinicopathological characteristics including tumor marker, tumor size, number, and vascular invasion did not show significant difference between the 2 groups (data is not shown), except ICG R15, which was significantly poorer in the 12-month follow-up group (ICG R15, 6.5% vs. 14%; P = 0.006).
The median survival time was 39 months in the 6-month interval follow-up group and 31 months in the 12-month interval follow-up group after detecting the recurrence. Curative treatment such as repeat resection and ablation therapy could be applied to 37.5% of the patients in the 6-month interval follow-up group and 40% of the patients in 12-month interval follow-up group. There were no significant differences between the two groups in survival time and curative treatment application. There were more candidates for salvage liver transplantation in the 6-month interval follow-up group (5, 62.5%) than in the 12-month interval follow-group (2, 40%). However, it did not show significant difference.
There was one randomized controlled study about the benefit of surveillance systems in patients with high risk of HCC development [14]. They reported that surveillance systems decreased the mortality brought on by HCC development. Recently, the number of patients who are diagnosed at early stage has increased due to surveillance systems [15] and when these patients underwent surgical resection, they showed good results. Especially, patients with T1 stage HCC showed similar overall survival after liver resection to those after liver transplantation [16,17].
However, those patients still experienced high recurrence rates and most recurrences developed within 2 years after liver resection [16,17], though some patients had recurrence more than 2 years after liver resection. It might be regarded as a de novo development of HCC [18,19]. Sometimes, some patients experienced recurrence more than 5 years after liver resection. In our study, eight patients with T1 stage HCC and 5 patients with T2 stage HCC showed late recurrence at more than 5 years after liver resection.
The optimal interval of surveillance is broadly investigated in high-risk patients. A six-month interval time is usually accepted as the optimal period in consideration of risk-benefit balance and cost [1,3,20-22]. Tumor marker and ultrasonography are useful methods to detect HCC in surveillance. However, there is no consensus for optimal follow-up period after liver resection.
Many surgeons have adopted a postoperative follow-up interval of 3 months in the first 2 years and 6 months after 2 years. This interval is commonly accepted as the optimal follow-up period [23]. However, there is no consensus about the follow-up interval after 5 years.
Our study showed that 8 patients with a 6-month follow-up interval had smaller tumors than patients with a 12-month follow-up interval and the difference was significant (P = 0.045). Repeat resection and salvage transplantation were effective treatment modalities for recurrent HCC. When patients with recurrence underwent repeat resection, those patients showed superiority in survival rates compared with those patients who received nonsurgical treatment [24-26]. Some reported that when patients with recurrence within Milan criteria underwent salvage transplantation, those patients showed similar survival compared with the survival of patients who underwent primary liver transplantation [27-30]. However, those treatments are limited to only highly select patients. In our study, patients who had a 6-month follow-up interval, showed a median 1.1 cm-sized tumors compared with 3 cm-sized tumors in patients who had a 12-month follow-up interval. Regardless of follow-up interval, most recurrent tumors are within Milan criteria; however, the tumors were smaller and more easily manageable when the follow-up interval was short-term (6 months).
Active hepatitis infection was reported as a prognostic factor of long-term prognosis and liver function was also reported to be associated with long-term prognosis. Only age was associated with prognosis at more than 5 years after liver resection in our study. Liver function and hepatitis infection status did not show a significant difference. Our study has some limitations. We checked the causes of underlying liver disease, which was mostly due to hepatitis B virus infection. However, we did not check the viral replication status or the antiviral treatment status. We have been prospectively collecting the data to check and analyze the effect of viral replication and antiviral treatment on the prognosis.
In conclusion, considering 13 out of 149 patients with T1 or T2 stage HCC exhibited recurrence more than 5 years after liver resection, the risk of late recurrence should not be underestimated. When the follow-up interval was short-term, 6 months, the recurrent tumors were detected at a smaller and more easily manageable state. The authors suggested that patients less than 60 years old have a 6-month follow-up period for easy detection and more effective management of recurrent tumor even 5 years after liver resection.
Figures and Tables
Fig. 1
Disease-free survival (DFS) rate after liver resection for patients with T1 and T2 stage hepatocellular carcinoma. Patients with T1 and T2 stage showed 55.8% and 35.4% 5-year disease-free survival rate, respectively (P = 0.033). AJCC, American Joint Committee on Cancer.
References
1. European Association For The Study Of The Liver. European Organisation For Research And Treatment Of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012; 56:908–943.
2. Bruix J, Sherman M. American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology. 2011; 53:1020–1022.
3. Omata M, Lesmana LA, Tateishi R, Chen PJ, Lin SM, Yoshida H, et al. Asian Pacific Association for the Study of the Liver consensus recommendations on hepatocellular carcinoma. Hepatol Int. 2010; 4:439–474.
4. Kim SH, Kang DR, Lee JG, Kim do Y, Ahn SH, Han KH, et al. Early predictor of mortality due to irreversible posthepatectomy liver failure in patients with hepatocellular carcinoma. World J Surg. 2013; 37:1028–1033.
5. Belghiti J, Hiramatsu K, Benoist S, Massault P, Sauvanet A, Farges O. Seven hundred forty-seven hepatectomies in the 1990s: an update to evaluate the actual risk of liver resection. J Am Coll Surg. 2000; 191:38–46.
6. Imamura H, Seyama Y, Kokudo N, Maema A, Sugawara Y, Sano K, et al. One thousand fifty-six hepatectomies without mortality in 8 years. Arch Surg. 2003; 138:1198–1206.
7. Jarnagin WR, Gonen M, Fong Y, DeMatteo RP, Ben-Porat L, Little S, et al. Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg. 2002; 236:397–406.
8. Bryant R, Laurent A, Tayar C, van Nhieu JT, Luciani A, Cherqui D. Liver resection for hepatocellular carcinoma. Surg Oncol Clin N Am. 2008; 17:607–633.
9. Fan ST, Lo CM, Liu CL, Lam CM, Yuen WK, Yeung C, et al. Hepatectomy for hepatocellular carcinoma: toward zero hospital deaths. Ann Surg. 1999; 229:322–330.
10. Stuart KE, Anand AJ, Jenkins RL. Hepatocellular carcinoma in the United States. Prognostic features, treatment outcome, and survival. Cancer. 1996; 77:2217–2222.
11. Lim KC, Chow PK, Allen JC, Siddiqui FJ, Chan ES, Tan SB. Systematic review of outcomes of liver resection for early hepatocellular carcinoma within the Milan criteria. Br J Surg. 2012; 99:1622–1629.
12. Kamiyama T, Nakanishi K, Yokoo H, Kamachi H, Tahara M, Suzuki T, et al. Recurrence patterns after hepatectomy of hepatocellular carcinoma: implication of Milan criteria utilization. Ann Surg Oncol. 2009; 16:1560–1571.
13. Taura K, Ikai I, Hatano E, Yasuchika K, Nakajima A, Tada M, et al. Influence of coexisting cirrhosis on outcomes after partial hepatic resection for hepatocellular carcinoma fulfilling the Milan criteria: an analysis of 293 patients. Surgery. 2007; 142:685–694.
14. Zhang BH, Yang BH, Tang ZY. Randomized controlled trial of screening for hepatocellular carcinoma. J Cancer Res Clin Oncol. 2004; 130:417–422.
15. Llovet JM, Bruix J. Novel advancements in the management of hepatocellular carcinoma in 2008. J Hepatol. 2008; 48:Suppl 1. S20–S37.
16. Rahman A, Assifi MM, Pedroso FE, Maley WR, Sola JE, Lavu H, et al. Is resection equivalent to transplantation for early cirrhotic patients with hepatocellular carcinoma? A meta-analysis. J Gastrointest Surg. 2012; 16:1897–1909.
17. Silva MF, Sapisochin G, Strasser SI, Hewa-Geeganage S, Chen J, Wigg AJ, et al. Liver resection and transplantation offer similar 5-year survival for Child-Pugh-Turcotte A HCC-patients with a single nodule up to 5 cm: a multicenter, exploratory analysis. Eur J Surg Oncol. 2013; 39:386–395.
18. Imamura H, Matsuyama Y, Tanaka E, Ohkubo T, Hasegawa K, Miyagawa S, et al. Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J Hepatol. 2003; 38:200–207.
19. Kim SH, Choi SB, Lee JG, Kim SU, Park MS, Kim DY, et al. Prognostic factors and 10-year survival in patients with hepatocellular carcinoma after curative hepatectomy. J Gastrointest Surg. 2011; 15:598–607.
20. Cottone M, Turri M, Caltagirone M, Parisi P, Orlando A, Fiorentino G, et al. Screening for hepatocellular carcinoma in patients with Child's A cirrhosis: an 8-year prospective study by ultrasound and alphafetoprotein. J Hepatol. 1994; 21:1029–1034.
21. Gebo KA, Chander G, Jenckes MW, Ghanem KG, Herlong HF, Torbenson MS, et al. Screening tests for hepatocellular carcinoma in patients with chronic hepatitis C: a systematic review. Hepatology. 2002; 36:5 Suppl 1. S84–S92.
22. Pateron D, Ganne N, Trinchet JC, Aurousseau MH, Mal F, Meicler C, et al. Prospective study of screening for hepatocellular carcinoma in Caucasian patients with cirrhosis. J Hepatol. 1994; 20:65–71.
23. Benson AB 3rd, Abrams TA, Ben-Josef E, Bloomston PM, Botha JF, Clary BM, et al. NCCN clinical practice guidelines in oncology: hepatobiliary cancers. J Natl Compr Canc Netw. 2009; 7:350–391.
24. Itamoto T, Nakahara H, Amano H, Kohashi T, Ohdan H, Tashiro H, et al. Repeat hepatectomy for recurrent hepatocellular carcinoma. Surgery. 2007; 141:589–597.
25. Wu CC, Cheng SB, Yeh DC, Wang J, P'eng FK. Second and third hepatectomies for recurrent hepatocellular carcinoma are justified. Br J Surg. 2009; 96:1049–1057.
26. Ho CM, Lee PH, Shau WY, Ho MC, Wu YM, Hu RH. Survival in patients with recurrent hepatocellular carcinoma after primary hepatectomy: comparative effectiveness of treatment modalities. Surgery. 2012; 151:700–709.
27. Fuks D, Dokmak S, Paradis V, Diouf M, Durand F, Belghiti J. Benefit of initial resection of hepatocellular carcinoma followed by transplantation in case of recurrence: an intention-to-treat analysis. Hepatology. 2012; 55:132–140.
28. Hu Z, Wang W, Li Z, Ye S, Zheng SS. Recipient outcomes of salvage liver transplantation versus primary liver transplantation: a systematic review and meta-analysis. Liver Transpl. 2012; 18:1316–1323.
29. Hu Z, Zhou J, Xu X, Li Z, Zhou L, Wu J, et al. Salvage liver transplantation is a reasonable option for selected patients who have recurrent hepatocellular carcinoma after liver resection. PLoS One. 2012; 7:e36587.
30. Lee SG. Salvage living-donor liver transplantation to previously hepatectomized hepatocellular carcinoma patients: is it a reasonable strategy? Hepatobiliary Pancreat Dis Int. 2013; 12:10–11.




 ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download