Abstract
Ortner syndrome or cardiovocal syndrome is a rare condition characterized by hoarseness of voice associated with cardiovascular pathology. Compression of the left recurrent laryngeal nerve by the pulmonary artery or left atrium is usually responsible. Recurrent aspiration pneumonia may cause significant morbidity and mortality. Early recognition and treatment along with removal of the underlying cause, if possible, may change an otherwise poor prognosis of the condition. The case presented here describes a 35-year old female with hoarseness of voice in association with mitral stenosis and bronchiectasis. Presence of dual pathology contributed to the overall pathophysiology of the disease, and made its management difficult.
Ortner syndrome or cardiovocal syndrome is a rare condition characterized by hoarseness of voice associated with cardiovascular pathology. Left recurrent laryngeal nerve palsy is the source of the hoarseness. Mitral stenosis is a common cause, but a myriad of other cardiac and non-cardiac conditions may be responsible as well.
A 35-year-old non-smoker, normotensive female patient presented with progressive breathlessness, recurrent episodes of productive cough and occasional haemoptysis for six months and hoarseness of voice for 1 month. She was on anti-TB drugs with standard regimen for the presumptive diagnosis of pulmonary tuberculosis, to which the response was poor. On examination, she was dyspnoic, mildly anaemic, had early clubbing but was not cyanosed. Her respiratory rate was 22/min, pulse 100/min, regular, blood pressure 100/60 mm of Hg, JVP raised with prominent a wave. There was a tapping apex beat, left parasternal heave, palpable P2 and a diastolic thrill over the apical area. The 1st and the pulmonary component of the 2nd heart sounds were loud, and a low-pitched, localised, mid diastolic murmur of grade 4/6 was heard over the apical area. Her breath sound was vesicular with bilateral coarse crepitations throughout the lower and mid chest. Total leukocyte count was 8000/mm3, erythrocyte sedimentation rate 15 mm in 1st hour, hemoglobin 10.8 gm/dL, C-reactive protein negative, anti-streptolysin O titer <200 IU, bleeding time 4 minutes, clotting time 5 minutes, prothrombin time was normal. Acid-fast bacilli were not found in the sputum and antibodies from lymphocyte secretions for the diagnosis of TB were negative. Ultrasonogram of the whole abdomen was unremarkable. Chest X-ray showed straightening of the left cardiac border and bilateral ring shadows in mid and lower lurg zones (Fig. 1). Echocardiography revealed moderate mitral stenosis with mitral valve area 1.35 cm2, mildly dilated left atrium (41 mm), dilated pulmonary artery and its branches and severe pulmonary hypertension (pulmonary artery systolic pressure, PASP 92 mm Hg). High resolution computed tomography (CT) scan of the chest (Fig. 2) revealed features of bilateral bronchiectasis, whereas CT pulmonary arteriography (Fig. 3) found dilated pulmonary arteries (pulmonary trunk 34 mm, right pulmonary artery 23.8 mm and the left pulmonary artery 18.7 mm). Left vocal cord palsy was detected in fibreoptic laryngoscopy (Fig. 4).
A diagnosis of chronic rheumatic heart disease, moderate mitral stenosis, bilateral bronchiectasis and Ortner syndrome was made. The patient was treated conservatively with rheumatic fever prophylaxis, additional antibiotics on the basis of culture and sensitivity report of sputum, chest physiotherapy, bronchodilators, diuretics and nifedipine. Over the next few months, she improved clinically, PASP came down to 62 mm Hg, but the findings remained unchanged in follow-up chest X-rays, and the hoarseness of voice did not improve significantly. While staying in the village, suddenly her condition deteriorated and on the way to the hospital she expired.
Ortner syndrome was first described by Nobert Ortner, a Viennese physician in 1897, in a case of mitral stenosis with dilated left atrium.1) Subsequently, it was reported with mitral stenosis,2)3) mitral regurgitation,4) atrial myxoma,5) primary pulmonary hypertension,6)7) thoracic aortic aneurysm,8)9) aortic dissection,10) pulmonary embolism,11) defibrillation,12) transcatheter ablation of atrial fibrillation,13) cardiothoracic surgery14) and heart-lung transplantation.15) The basic abnormality is paralysis of the left recurrent laryngeal nerve. Though an initially enlarged left atrium was thought to be the main culprit, the current understanding favours pressure in the pulmonary artery playing the most important role in causing the nerve compression in a majority of the cases.10) The incidence of cardiovocal syndrome in mitral stenosis ranges from 0.6% to 5%.16)
The most common manifestation of Ortner syndrome is hoarseness of voice. Unilateral vocal cord paralysis increases the risk of aspiration which may be present in up to 40% of patients.17)
In the present case, the left recurrent laryngeal nerve was most probably compressed by the dilated pulmonary artery, not by the left atrium because the latter was only mildly dilated. Also the moderate mitral stenosis in isolation was unlikely to cause severe pulmonary hypertension. Bilateral bronchiectasis probably contributed to the major share of the severity of pulmonary hypertension which ultimately caused dilatation of the pulmonary arteries. Presence of dual pathology aggravated the situation.
Ortner syndrome is suspected from history and clinical examination; a chest X-ray or CT scans of the chest, fibreoptic laryngoscopy and laryngeal electromyography help confirmation of the diagnosis.18)
The prognosis of recurrent laryngeal nerve paralysis depends on the degree and duration of nerve compression.19) The treatment of unilateral vocal cord palsy consists of early rehabilitation, treatment of the primary etiology and endoscopic insertion of a prosthesis or injection of fat or collagen.10) There are two absolute indications for surgery: aspiration pneumonia and the patient's desire to improve the voice-related quality of life.20) Considering the general condition of the patient, conservative strategy was adopted. Relieve of mitral stenosis by percutaneous transluminal mitral commissurotomy could be done, but in presence of moderate degree of stenosis and high risk from comorbid lung disease, the idea was abandoned. In conclusion, Ortner syndrome is a rare entity. A number of cardiovascular conditions may contribute to its aetiopathogenesis. Presence of dual pathology may make the diagnosis and management difficult and worsen the prognosis.
Figures and Tables
Fig. 1
Radiologic findings of chest X-ray. A: postero-anterior view shows multiple ring shadows through the cardiac silhouette. B: left lateral view shows reduction of retrosternal and retrocardiac spaces and multiple ring shadows through the cardiac silhouette.
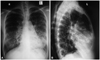
Fig. 2
High resolution CT scan of chest, lung window setting shows multiple cystic air spaces larger than the corresponding vessels in all segments of both lungs.

Fig. 3
CT pulmonary angiogram. A: coronal view shows CT pulmonary angiogram, coronal view shows the dilated pulmonary trunk. B: axial view shows CT pulmonary angiogram shows dilated pulmonary trunk and its branches; pulmonary trunk 34 mm, right pulmonary artery 23.8 mm and the left pulmonary artery 18.7 mm.

References
1. Ortner N. Recurrent laryngeal nerve paralysis due to mitral valve stenosis. Wien Klin Wochenschr. 1897. 10:753–755.
2. Plastiras SC, Pamboucas C, Zafiriou T, Lazaris N, Toumanidis S. Ortner's syndrome: a multifactorial cardiovocal syndrome. Clin Cardiol. 2010. 33:E99–E100.
3. Prada-Delgado O, Barge-Caballero E. Images in clinical medicine: Ortner's syndrome. N Engl J Med. 2011. 365:939.
4. Gulel O, Koprulu D, Kucuksu Z, Yazici M, Cengel S. Images in cardiovascular medicine: cardiovocal syndrome associated with huge left atrium. Circulation. 2007. 115:e318–e319.
5. Rubens F, Goldstein W, Hickey N, Dennie C, Keon W. Hoarseness secondary to left atrial myxoma. Chest. 1989. 95:1139–1140.
6. Kagal AE, Shenoy PN, Nair KG. Ortner's syndrome associated with primary pulmonary hypertension. J Postgrad Med. 1975. 21:91–95.
7. Nakao M, Sawayama T, Samukawa M, et al. Left recurrent laryngeal nerve palsy associated with primary pulmonary hypertension and patent ductus arteriosus. J Am Coll Cardiol. 1985. 5:788–792.
8. Ishimoto S, Ito K, Toyama M, et al. Vocal cord paralysis after surgery for thoracic aortic aneurysm. Chest. 2002. 121:1911–1915.
9. Escribano JF, Carnés J, Crespo MA, Antón RF. Ortner's syndrome and endoluminal treatment of a thoracic aortic aneurysm: a case report. Vasc Endovascular Surg. 2006. 40:75–78.
10. Lee SI, Pyun SB, Jang DH. Dysphagia and hoarseness associated with painless aortic dissection: a rare case of cardiovocal syndrome. Dysphagia. 2006. 21:129–132.
11. Albertini RE. Vocal cord paralysis associated with pulmonary emboli. Chest. 1972. 62:508–510.
12. Victoria L, Graham SM, Karnell MP, Hoffman HT. Vocal fold paralysis secondary to cardiac countershock (cardioversion). J Voice. 1999. 13:414–416.
13. Pai RK, Boyle NG, Child JS, Shivkumar K. Transient left recurrent laryngeal nerve palsy following catheter ablation of atrial fibrillation. Heart Rhythm. 2005. 2:182–184.
14. Tewari P, Aggarwal SK. Combined left-sided recurrent laryngeal and phrenic nerve palsy after coronary artery operation. Ann Thorac Surg. 1996. 61:1721–1722.
15. Murty GE, Smith MC. Recurrent laryngeal nerve palsy following heart-lung transplantation: three cases of vocal cord augmentation in the acute phase. J Laryngol Otol. 1989. 103:968–969.
16. Solanki SV, Yajnik VH. Ortner's syndrome. Indian Heart J. 1972. 24:43–46.
17. Meyer E, Jonas NE, Zühlke LJ. Ortner syndrome. S Afr J Child Health. 2008. 2:170–171.
18. Ishii K, Adachi H, Tsubaki K, Ohta Y, Yamamoto M, Ino T. Evaluation of recurrent nerve paralysis due to thoracic aortic aneurysm and aneurysm repair. Laryngoscope. 2004. 114:2176–2181.
19. Mulpuru SK, Vasavada BC, Punukollu GK, Patel AG. Cardiovocal syndrome: a systematic review. Heart Lung Circ. 2008. 17:1–4.
20. Hartl DM, Travagli JP, Leboulleux S, Baudin E, Brasnu DF, Schlumberger M. Clinical review: current concepts in the management of unilateral recurrent laryngeal nerve paralysis after thyroid surgery. J Clin Endocrinol Metab. 2005. 90:3084–3088.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download