Abstract
Background
In a previous biomechanical study, eccentric glenospheres with more inferior position of the center of rotation were shown to improve range of motion and reduce the incidence of scapular notching after reverse total shoulder arthroplasty (RSA). The purpose of this study was to compare the clinical and radiological results of RSA using an eccentric glenosphere to those using a concentric glenosphere and to determine the usefulness of the eccentric glenosphere.
Methods
From 2009 to 2015, we performed a retrospective review of 20 consecutive patients who underwent RSA using a deltopectoral approach. Nine patients underwent RSA using a concentric glenosphere (group A) while 11 had an eccentric glenosphere (group B). The average follow-up period was 13.9 months (range, 12 to 18 months). All glenoid components were placed with 15° of inferior tilt. Clinical results were assessed using the visual analog pain scale score (VAS), the American Shoulder and Elbow Surgeon (ASES) score, the Korean shoulder scoring system (KSS), and the Constant score. On radiological evaluation, prosthesisscapular neck angle (PSNA), peg-glenoid rim distance (PGRD), scapular neck-inferior glenoshere rim distance (inferior glenoshpere overhang), acromion-greater tuberosity (AT) distance, glenoid-greater tuberosity (GT) distance, and severity of notching according to the Nerot-Sirveaux classification were assessed.
Results
The clinical results improved significantly in both groups, but there was no statistically significant difference between the two groups. A significant intergroup difference was observed with regard to PGRD (24.8 ± 1.6 mm for group A vs. 22.2 ± 1.9 mm for group B; p = 0.002) and inferior glenosphere overhang (2.0 ± 1.7 mm for group A vs. 5.8 ± 1.6 mm for group B; p = 0.000). Seven of 9 patients in group A developed notching compared with 2 of 11 patients in group B (p = 0.022). The other radiological parameters such as inferior tilt and AT and GT distances were not significantly different between two groups. Complications such as loosening and scapular fractures did not occur.
Since Grammont et al.1) introduced reverse total shoulder arthroplasty (RSA) in 1987, many authors have reported good results of the procedure in terms of pain relief and functional recovery. However, scapular notching, caused by mechanical impingement between the humeral cup and the scapular neck, has been noted in 44% to 96% after RSA in several studies.23) In an attempt to prevent this phenomenon, various methods have been suggested, such as eccentric (inferior) positioning,4) inferior tilting,5) lateral offset,6) reduction of the humeral neck-shaft angle,4) larger glenoid component insertion,6) and increasing humeral component retroversion.7)
de Wilde et al.4) compared the six different methods using a 2-dimensional (2D) computer simulation without taking into account the soft tissues and muscles. They concluded that inferior positioning of the glenosphere was the most effective way to overcome the problem of scapular notching. In a biomechanical study related to RSA, inferior positioning of the glenosphere with more inferior position of the center of rotation was shown to improve the range of motion and reduce the incidence of scapular notching.5) Based on such research, eccentric glenospheres have been introduced in RSA. However, in spite of the advantage of reducing scapular notching through inferior positioning of the center of rotation, inferior glenosphere positioning raises the risk of acromial fracture caused by excessive tension due to the increased lever arm of the deltoid. The purpose of this study was to evaluate the clinical and radiological results of RSA using an eccentric glenosphere compared with RSA using a concentric glenosphere and to determine the usefulness of the eccentric glenosphere. We established two hypotheses regarding the consequences of the more inferior positioning of the center of rotation in RSA using an eccentric glenosphere. First, the increase in inferior glenosphere overhang would be related to reduction in scapular notching. Second, the increase in the deltoid lever arm could cause complications such as loosening or scapular fracture.
From December 2009 to February 2015, we performed a retrospective review of 22 consecutive patients who underwent RSA due to cuff tear arthropathy (CTA). The inclusion criteria were patients who underwent RSA for CTA and functional and radiological evaluation for a minimum follow-up of 12 months. The exclusion criteria were the following: (1) RSA for fracture; (2) RSA for rheumatoid arthritis; (3) hemi- or total shoulder arthroplasty for CTA; (4) inadequate follow-up (less than 12 months); and (5) patients without radiological evaluation for at least 1 postoperative year. Two of the 22 patients were lost to follow-up ultimately leaving 20 patients for analysis. The patients were divided into two groups. Nine patients in group A received a 36-mm concentric glenosphere (Aequalis Reverse Prosthesis; Tornier, Houston, TX, USA) between December 2009 and June 2013. Eleven patients in group B had a 36-mm eccentric glenosphere (SMR Reverse Shoulder Prosthesis; Lima Corporate, Udine, Italy) between February 2014 and February 2015, which was a different device but the surgical protocol was the same. Demographic data were collected on each patient including age, sex, the operated side, body mass index (BMI), indication for RSA, and history of surgery on the affected shoulder. The average follow-up period was 13.9 ± 2.6 months (range, 12 to 18 months). This study was approved by the Institutional Review Board of Daegu Catholoic University Medical Center and informed consent was exempted (No. CR-16-047-L).
All RSAs were performed in the beach chair position by a single senior author (CHC) using the deltopectoral approach under general anesthesia. The humeral head was cut with 20° of retroversion and the glenoid was reamed in approximately 15° of inferior tilt. A guide wire and a glenoid baseplate were inserted using the same surgical technique in both groups. However, the eccentric glenosphere (SMR Reverse Shoulder Prosthesis) provided 4-mm inferior offset to generate inferior overhang. Suitable tension could be adjusted after template reduction using the trial component. This could be noted at surgery as the openbook phenomenon when the arm was internally and externally rotated. An improper tension could cause the open book phenomenon where the component is levered away from the glenoid. The final stability was checked by fluoroscopic examination. All patients underwent subscapularis tendon repair using transosseous suture in order to match the transverse force couple and a soft tissue biceps tenodesis when the tendon was still present.
Postoperatively, the patient wore an abduction brace for 4 weeks. Active elbow motion and hand grip exercises were started the day after surgery. Pendulum exercises and passive range of motion were started 2 weeks after surgery, depending on the status of the surgical wound. After 4 weeks, the brace was discontinued and normal daily activities were allowed as tolerated.
Patients were regularly followed up in the outpatient department. Clinical assessments were performed by the senior author. Medical records of all patients were reviewed independently. Radiological parameters were measured by two orthopedic surgeons, both of whom were blinded to the clinical outcomes. The averages of the measurements were used for statistical analysis of the radiological parameters.
Clinical results were assessed using the visual analog pain scale score (VAS), the American Shoulder and Elbow Surgeon (ASES) score,8) the Korean shoulder scoring system (KSS),9) and the Constant score10) preoperatively and postoperatively at the final follow-up between 12 to 18 months. The degrees of active forward flexion, external rotation, and internal rotation were measured at each follow-up.
Radiological examination was performed using anteroposterior (AP) views of the glenohumeral joint in neutral rotation. Postoperatively, the prosthesis-scapular neck angle (PSNA) was used to evaluate the inferior tilt (Fig. 1A), the peg-glenoid rim distance (PGRD) was measured to assess the inferior positioning of the baseplate (Fig. 1B), and the scapular neck-inferior glenosphere rim distance represented the degree of inferior glenosphere overhang (Fig. 1C).211) The acromion-greater tuberosity (AT) distance was used to evaluate the amount of humeral lengthening (Fig. 1D) and the glenoid-greater tuberosity (GT) distance was measured to assess the amount of medialization or lateralization of the humerus (Fig. 1E).12) Inferior scapular notching was classified according to the Nerot-Sirveaux classification at the final follow-up between 12 to 18 months (Fig. 2).13)
The IBM SPSS ver. 19.0 (IBM Co., Armonk, NY, USA) was used for statistical analysis of clinical and radiological results. A p-values were calculated using the Mann-Whitney U-test, Wilcoxon signed-rank test, and Fisher exact test, and the statistical significance was assumed at p < 0.05.
This study included a total of 20 patients: 9 in group A and 11 in group B. The mean age at the time of surgery was 39.0 years (range, 52 to 86 years). There were 8 men and 12 women. The surgery was performed on the right shoulder in 11 and on the left shoulder in 9. The mean BMI at the time of surgery was 23.7 kg/m2 (range, 17.7 to 27.1 kg/m2). The mean follow-up period was 13.9 months (range, 12 to 18 months). Patient demographics for each group are summarized in Table 1. There was no statistically significant difference in patient demographics between the two groups (p > 0.05).
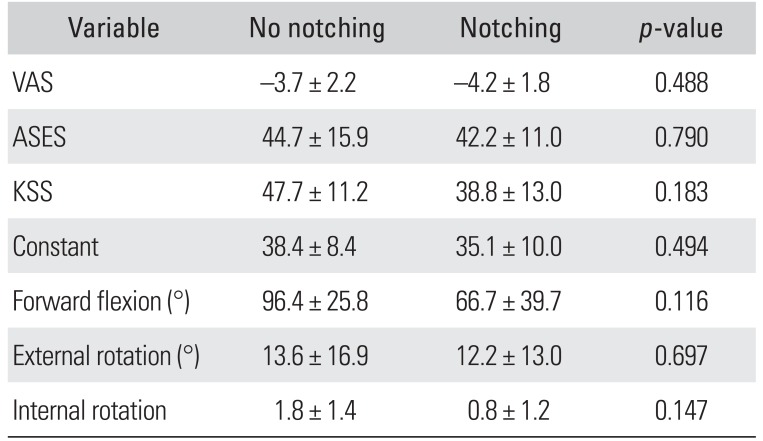
The mean clinical test scores and range of motion in all planes are presented in Tables 2 and 3. Compared to preoperative values, the postoperative clinical results were significantly improved at the final follow-up in both groups (p < 0.05) (Table 2). However, there was no statistically significant difference between the two groups (p > 0.05) (Table 3).
The mean radiological assessment results for each group are listed in Table 4. Compared to group B, the PGRD was significantly greater in group A (p = 0.002). The AT and GT distances were longer in group B than in group A, but the difference did not reach statistical significance (p > 0.05). Compared to group A, inferior overhang was significantly greater in group B (p = 0.000). Inferior scapular notching was present in 9 patients: 7 of 9 patients in group A and 2 of 11 patients in group B. The notching was grade 1 in all patients, there was no patient with grades 2, 3, and 4. There was a significant difference in the incidence of notching between the groups (p = 0.022).
The principal finding of this study is the usefulness of the eccentric glenosphere with 15° of inferior tilt based on comparison with the concentric glenosphere. de Wilde et al.4) demonstrated in a computer model that the largest reduction in notching was observed in the first 2 mm of overhanging and the prosthetic overhang seemed to be an important factor in preventing notching. Mizuno et al.14) reported that 2 mm of inferior overhang could not prevent notching but reduced the severity of scapular notching. The incidence of scapular notching was 40.4% in their study. De Biase et al.11) showed that inferior scapular notching did not occur in the patients who had a 4.3-mm eccentric glenosphere. In the patients, the mean PSNA, PGRD, and inferior overhang were 92°, 21.2 mm, and 4.3 mm, respectively. Poon et al.15) suggested that more than 3.5 mm of inferior overhang could prevent notching; however, there were no differences in the incidence of notching or clinical results between concentric and eccentric glenospheres. In our study, the 5.8 mm eccentric glenosphere with 15° of inferior tilt could reduce the incidence of notching, but grade 1 notching occurred in 2 patients. Compared to the concentric glenosphere with 2.0 mm of overhang and 15° of tilt, the eccentric glenosphere resulted in a statistically significant decrease in the incidence of notching.
Gutierrez et al.16) reported in a biomechanical study that approximately 15° of inferior tilt maximized compression and minimized tension and amount of micromotion at the bone-prosthetic interface. They emphasized that the inferior tilt was most effective in reducing the mechanical failure of the glenoid implant. de Wilde et al.4) demonstrated in a computer simulation that the inferior glenoid inclination was associated with a 1° increase in impingement-free range of motion for each degree of inclination. Nyffeler et al.5) showed in a cadaver study that oblique resection of the glenoid improved abduction and adduction impingement-free range of motion, but it reduced the hard subchondral bone and could weaken fixation of the glenoid implant. Simovitch et al.2) reported that inferior tilt resulted in an increase in PSNA, which increased the incidence of notching. In a prospective study by Edwards et al.,17) inferior tilt did not decrease the severity or incidence of scapular notching. In our study, the 15° of inferior tilt was the same in both groups. The incidence of scapular notching in the concentric glenosphere group was 77.8% (7 of 9 patients) and thus we thought that the inferior tilt alone was not effective in preventing scapular notching.
Roche et al.18) demonstrated in a three-dimensional (3D) computer simulation that the oval/curved-back glenoid baseplate could decrease bone removal at the bone implant interface as compared to a circular/flat-back design. The concentric glenosphere (Aequalis Reverse Prosthesis) had a 29-mm diameter circular glenoid baseplate with a flatback and the eccentric glenosphere (SMR Reverse Shoulder Prosthesis) had a small-R oval baseplate with a curvedback. In our study, the PGRD in the eccentric group was smaller than that in the concentric group and we thought that the removal of a relatively large bone in the concentric group induced the increase in PGRD.
The eccentric glenosphere allows for increased range of motion, especially adduction, due to the inferior center of rotation.19) The inferior center of rotation could result in overtension of the deltoid muscle. Inadequate tension of the deltoid muscle could result in brachial plexus injury, prosthetic instability, deltoid insufficiency, or fatigue fracture of the scapular spine or acromion.1220) In our study, the deltoid lever arm parameters such as the AT and GT distances were larger in the eccentric glenosphere group than in the concentric glenosphere group, but the difference did not reach statistical significance because we matched the tension intraoperatively. As a result, the range of motion was not different between the groups, indicating that soft tissue balancing might be a more influencing factor. In addition, glenoid component loosening and scapular fracture did not occur.
Falaise et al.21) evaluated the relationship between the BMI and the development of notching and reported that thin patients had a higher risk of scapular notching. In our study, there was no significant difference in BMI between the patients with or without inferior scapular notching.
This study had several limitations. First, this was a retrospective study and grouping was done based on the time interval rather than by randomization. Second, the follow-up period was short. It has been known that inferior notching occurs at a mean of 4.5 months after surgery and no later than 14 months after surgery, but it does not progress in grade and size at a mean of 18 months after surgery.2) In our study, only grade 1 notching was observed and the short follow-up period might have caused this. However, the follow-up period did not affect generation of notching because the purpose of this study was to compare the two glenosphere designs. Progression of notching could be investigated in further research. Third, the study was based on a small population and thus had insufficient statistical power to accept the null hypothesis. We limited the use of RSA to CTA patients and expected to obtain significant results in a small group. Fourth, this was a heterogeneous study including two different prosthesis types manufactured by different companies. The concentric glenosphere was designed in the same radius, but the eccentric glenosphere was designed with three different sections of different radii. However, the strength of this study is that the surgery was performed by one surgeon at a single center using the same surgical technique regardless of the prosthesis design.
In summary, there was no significant difference in the clinical results and range of motion between the two groups. The eccentric glenosphere with 15° of inferior tilt could reduce the incidence of notching at a statistically significant level. Inferior tilt alone did not appear to affect prevention of scapular notching. The deltoid lever arm was slightly larger in the eccentric glenosphere compared with the concentric glenosphere, although this difference did not reach statistical significance. Finally, glenoid component loosening and scapular and acromial fractures did not occur.
In conclusion, the clinical results and range of motion improved in both groups after RSA showing no statistically significant intergroup difference. However, the eccentric glenosphere was superior to the concentric glenosphere in reducing the incidence of notching.
References
1. Grammont P, Trouilloud P, Laffay J, Deries X. Concept study and realization of a new total shoulder prosthesis. Rhumatologie. 1987; 39:407–418.
2. Simovitch RW, Zumstein MA, Lohri E, Helmy N, Gerber C. Predictors of scapular notching in patients managed with the Delta III reverse total shoulder replacement. J Bone Joint Surg Am. 2007; 89(3):588–600. PMID: 17332108.

3. Werner CM, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005; 87(7):1476–1486. PMID: 15995114.

4. de Wilde LF, Poncet D, Middernacht B, Ekelund A. Prosthetic overhang is the most effective way to prevent scapular conflict in a reverse total shoulder prosthesis. Acta Orthop. 2010; 81(6):719–726. PMID: 21110704.

5. Nyffeler RW, Werner CM, Gerber C. Biomechanical relevance of glenoid component positioning in the reverse Delta III total shoulder prosthesis. J Shoulder Elbow Surg. 2005; 14(5):524–528. PMID: 16194746.

6. Gutierrez S, Comiskey CA 4th, Luo ZP, Pupello DR, Frankle MA. Range of impingement-free abduction and adduction deficit after reverse shoulder arthroplasty: hierarchy of surgical and implant-design-related factors. J Bone Joint Surg Am. 2008; 90(12):2606–2615. PMID: 19047705.
7. Stephenson DR, Oh JH, McGarry MH, Rick Hatch GF 3rd, Lee TQ. Effect of humeral component version on impingement in reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2011; 20(4):652–658. PMID: 21144775.

8. Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002; 11(6):587–594. PMID: 12469084.

9. Tae SK, Rhee YG, Park TS, et al. The development and validation of an appraisal method for rotator cuff disorders: the Korean Shoulder Scoring System. J Shoulder Elbow Surg. 2009; 18(5):689–696. PMID: 19278871.

10. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987; (214):160–164. PMID: 3791738.

11. De Biase CF, Delcogliano M, Borroni M, Castagna A. Reverse total shoulder arthroplasty: radiological and clinical result using an eccentric glenosphere. Musculoskelet Surg. 2012; 96(Suppl 1):S27–S34. PMID: 22528848.

12. Otto RJ, Virani NA, Levy JC, Nigro PT, Cuff DJ, Frankle MA. Scapular fractures after reverse shoulder arthroplasty: evaluation of risk factors and the reliability of a proposed classification. J Shoulder Elbow Surg. 2013; 22(11):1514–1521. PMID: 23659805.

13. Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Mole D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff: results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004; 86(3):388–395. PMID: 15125127.
14. Mizuno N, Denard PJ, Raiss P, Walch G. The clinical and radiographical results of reverse total shoulder arthroplasty with eccentric glenosphere. Int Orthop. 2012; 36(8):1647–1653. PMID: 22534957.

15. Poon PC, Chou J, Young SW, Astley T. A comparison of concentric and eccentric glenospheres in reverse shoulder arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2014; 96(16):e138. PMID: 25143506.
16. Gutierrez S, Greiwe RM, Frankle MA, Siegal S, Lee WE 3rd. Biomechanical comparison of component position and hardware failure in the reverse shoulder prosthesis. J Shoulder Elbow Surg. 2007; 16(3 Suppl):S9–S12. PMID: 16990024.
17. Edwards TB, Trappey GJ, Riley C, O'Connor DP, Elkousy HA, Gartsman GM. Inferior tilt of the glenoid component does not decrease scapular notching in reverse shoulder arthroplasty: results of a prospective randomized study. J Shoulder Elbow Surg. 2012; 21(5):641–646. PMID: 22079769.

18. Roche CP, Diep P, Hamilton MA, Flurin PH, Routman HD. Comparison of bone removed with reverse total shoulder arthroplasty. Bull Hosp Jt Dis (2013). 2013; 71(Suppl 2):S36–S40. PMID: 24328578.
19. Chou J, Malak SF, Anderson IA, Astley T, Poon PC. Biomechanical evaluation of different designs of glenospheres in the SMR reverse total shoulder prosthesis: range of motion and risk of scapular notching. J Shoulder Elbow Surg. 2009; 18(3):354–359. PMID: 19393929.

20. Debeer P, Robyns F. Fracture of the scapular spine in a patient with a Delta III prosthesis. Acta Orthop Belg. 2005; 71(5):612–614. PMID: 16305089.
21. Falaise V, Levigne C, Favard L; SOFEC. Scapular notching in reverse shoulder arthroplasties: the influence of glenometaphyseal angle. Orthop Traumatol Surg Res. 2011; 97(6 Suppl):S131–S137. PMID: 21820377.

Fig. 1
Radiographic measurements. (A) The prosthesis-scapular neck angle. (B) The peg glenoid rim distance. (C) The scapular neck inferior glenosphere rim distance. (D) The acromion-greater tuberosity distance. (E) The glenoid-greater tuberosity distance.

Fig. 2
Inferior scapular notching. (A) Scapular notching (arrow) in a patient with a concentric glenosphere. (B) Scapular notching (arrow) in a patient with an eccentric glenosphere.
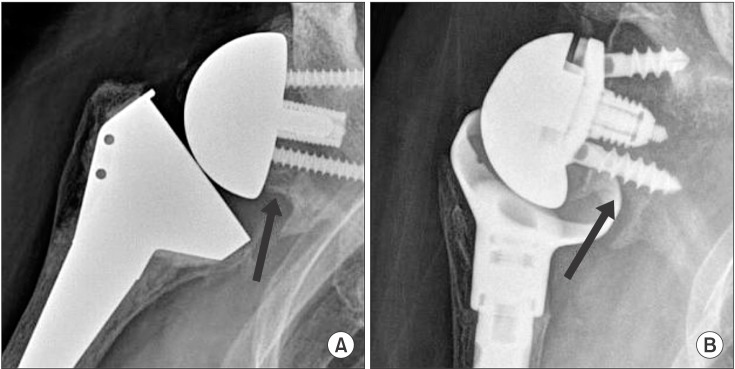
Table 1
Demographic Data
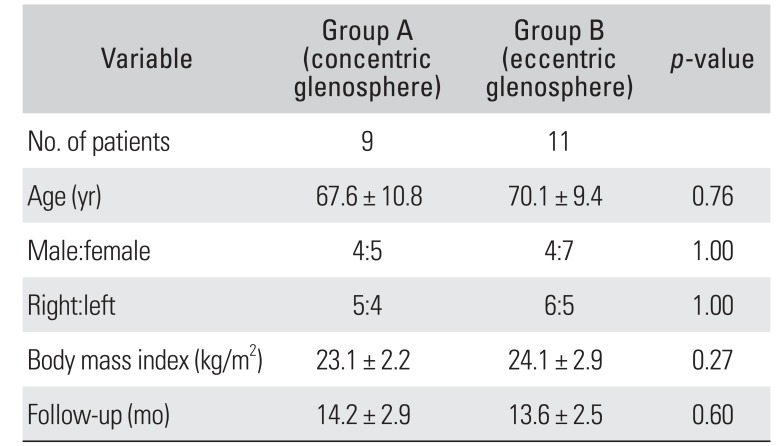
Table 2
Clinical Assessment: Comparison of Preoperative and Final Follow-up Values
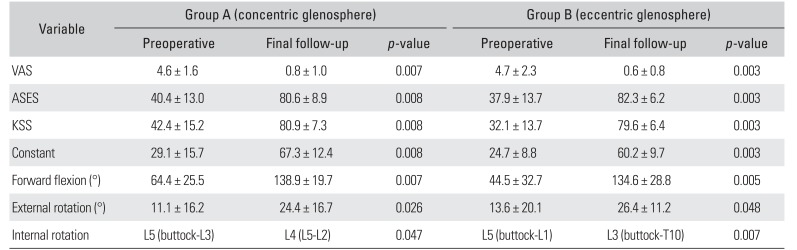
Table 3
Clinical Assessment: Comparison between the Groups
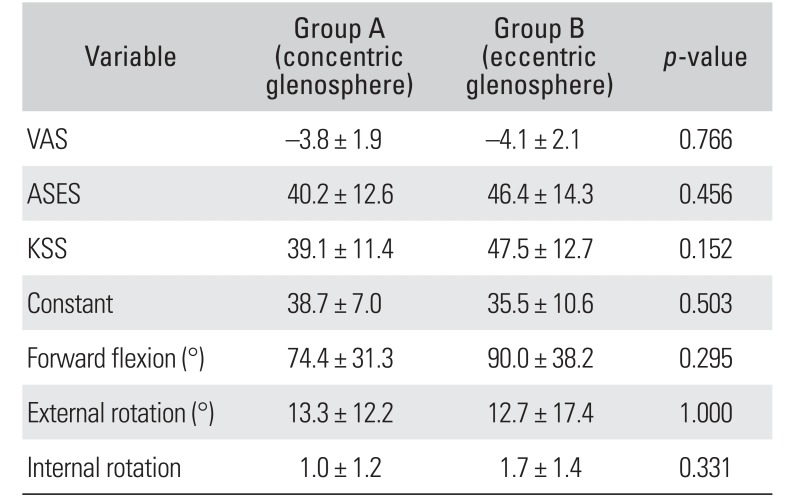
Table 4
Radiological Assessment: Comparison between the Groups
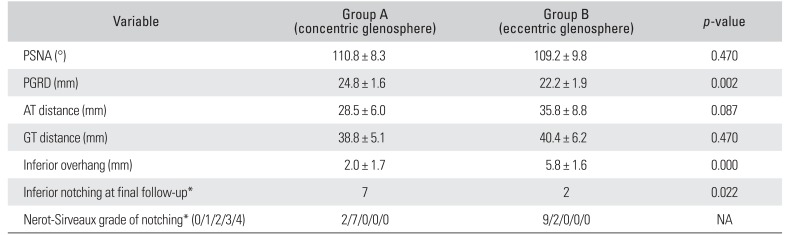
Table 5
Patient Factors according to the Presence of Scapular Notching
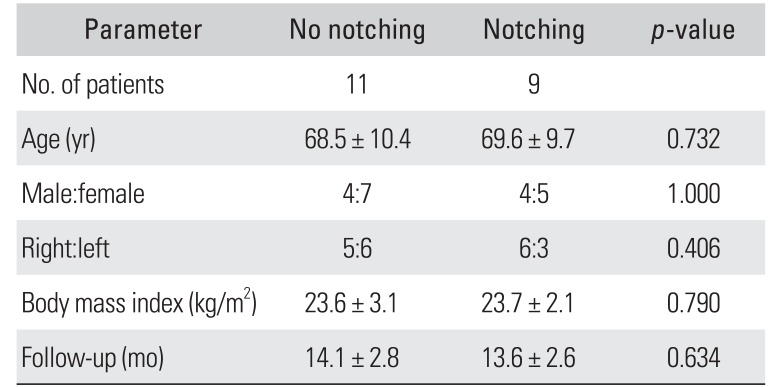
Table 6
Clinical Results according to the Presence of Scapular Notching




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download