Abstract
A goal of total knee arthroplasty is to obtain symmetric and balanced flexion and extension gaps. Controversy exists regarding the best surgical technique to utilize to obtain gap balance. Some favor the use of a measured resection technique in which bone landmarks, such as the transepicondylar, the anterior-posterior, or the posterior condylar axes are used to determine proper femoral component rotation and subsequent gap balance. Others favor a gap balancing technique in which the femoral component is positioned parallel to the resected proximal tibia with each collateral ligament equally tensioned to obtain a rectangular flexion gap. Two scientific studies have been performed comparing the two surgical techniques. The first utilized computer navigation and demonstrated a balanced and rectangular flexion gap was obtained much more frequently with use of a gap balanced technique. The second utilized in vivo video fluoroscopy and demonstrated a much high incidence of femoral condylar lift-off (instability) when a measured resection technique was used. In summary, the authors believe gap balancing techniques provide superior gap balance and function following total knee arthroplasty.
Creation of symmetric balanced flexion and extension gaps is a surgical goal of a total knee arthroplasty (TKA).1) Precise soft tissue balancing combined with accurate bone resections determine rotation of the femoral component.2) Improper femoral component rotation results in patellofemoral instability,3) anterior knee pain, arthrofibrosis,4) and flexion gap instability.5,6) Gap balancing and measured resection techniques have been used to determine femoral component rotation. This chapter will review gap balancing techniques, emphasizing key surgical techniques to achieve correct femoral component rotation and flexion stability as well as discuss measured resection methodologies.
Gap balancing techniques rely on ligament releases prior to bone cuts. These ligament releases correct fixed deformities and bring the limb into the correct approximate alignment before determination of femoral component rotation.7) There are basically two gap balancing sequences. One relies on balancing the flexion gap first. The other technique initially balances the knee in extension and later balances the flexion gap to the initially established extension gap. This section will review both techniques and discuss advantages and disadvantages of each.
Many surgeons balance the flexion gap before the extension gap. After initial knee exposure, a perpendicular proximal tibial resection is made relative to the longitudinal axis of the tibia. An accurate proximal tibial cut is crucial because the tibial resection will serve as a base and reference for the femoral bone resections. A varus tibial resection will result in internal rotation of the femoral component when a tensioned rectangular flexion gap is created.8) Conversely, a valgus tibial resection will lead to excessive external rotation of the femoral component. It is critical to remove all osteophytes before any extensive soft tissue releases or femoral bone resections are performed. When the joint is accurately tensioned in flexion, the tibial cut should align parallel to the transepicondylar axis (TEA) and will be perpendicular to the anteroposterior (AP) axis (Fig. 1). Corrective soft tissue releases can then be performed if these axes do not align properly. Once the joint is accurately tensioned in flexion, anterior and posterior femoral condylar resections are made using an anterior referencing AP cutting block. Spacer blocks can be inserted into the flexion gap to assure appropriate flexion gap symmetry.
After accurate balancing in flexion, attention is directed toward the extension gap. With the knee in extension, tensioning devices, set at a similar tension level to flexion gap, establish the extension gap (Fig. 2). An intramedullary or extramedullary guide is attached to the tensioning jig and the lower extremity alignment versus the mechanical axis is carefully evaluated. Additional soft tissue balancing can be done to correct alignment. Once a symmetric flexion and extension gap is obtained, the distal femoral cutting jig is applied and the distal femoral cut is made. Again, a spacer block is inserted into the extension gap to check extension gap symmetry and equality with the flexion gap.
Alternatively, surgeons can balance the extension gap prior to the flexion gap. The authors currently favor this method of gap balancing as we have found that initial soft tissue releases of the knee in extension provide more precise and reproducible gap balance. With this technique, the distal femur is initially resected with an intramedullary guide followed by proximal tibial resection at a 90 degrees angle to the longitudinal tibial axis. Because of their tensioning effect on adjacent ligamentous structures, all osteophytes, including posterior femoral and tibial osteophytes, must then be removed at this point before any soft tissue releases are performed. Early removal of posterior femoral and tibial osteophytes, before final posterior femoral condylar resections are completed, is critical because they tension adjacent ligamentous structures and can cause flexion gap asymmetry leading to malrotation of the femoral component. It is typically difficult to gain access to posterior compartment osteophytes initially due to difficulty of instrument passage into the posterior compartment. The authors suggest making a preliminary four millimeter resection of the one or both of the posterior femoral condyles with the knee flexed 90 degress (Fig. 3A). Next, a laminar spreader is used to distract the flexion gap and provide access to the posterior osteophytes. A curved osteotome (Fig. 3B) is then used to remove the posterior femoral osteophytes (Fig. 3C). Following extension gap resection and osteophyte removal, gap symmetry, soft tissue balance and lower extremity alignment versus the mechanical axis is assessed by placing a spacer block into the extension gap (Fig. 4). If ligament imbalance is present, tight ligamentous structures are released until alignment of the limb is neutral and the extension gap is symmetric.9)
Once the knee is balanced symmetrically in extension, the goal is to balance the flexion gap by duplicating the dimensions of the extension gap. Implant specific tensioners or laminar spreaders can be used to equally tension the collateral ligaments with the knee at 90 degrees of flexion. The transepicondylar and AP axes are constructed and used as secondary determinants of femoral component rotation. When the knee is well balanced in extension and the tibial resection is accurate, the resected proximal tibia should be parallel to the TEA and perpendicular to the AP axis (Fig. 5). If there is a wide divergence of the TEA from the proximal tibial resection at this point (a nonparallel relationship) with each collateral ligament equally tensioned, one or more of three things has occurred: (1) an error in the proximal tibial resection; (2) an error in precise determination of the TEA; or (3) the flexion gap stabilizing structures being tensioned (superficial medial collateral ligament medially or lateral collateral ligament-popliteus tendon complex laterally) are incompetent. If these structures are considered to be damaged, the authors favor placement of the AP femoral cutting block parallel to the TEA. The appropriately sized AP femoral cutting block is then applied and adjusted until it is parallel with the resected proximal tibia. By adjusting the AP cutting block anteriorly or posteriorly, a flexion gap width equal to that of the previously established extension gap is created (Fig. 6).10-12) To assure flexion-extension gap symmetry, the same spacer block previously used to establish the symmetrical extension gap is placed beneath the AP cutting block and onto the resected proximal tibial surface and flexion gap tension is again assessed before resection of the posterior femoral condyles (Fig. 7).
Improved flexion stability can be obtained by using gap balancing techniques to create a rectangular flexion gap.11,12) Using eight frozen cadaver knees, Katz et al.12) compared the reliability of the TEA, AP axis, and gap balancing techniques to determine femoral rotational alignment. They found that the TEA was less predictable and significantly more externally rotated than the AP axis (p < 0.005) and the gap balancing method (p < 0.00001). Due to its independence from obscured or poorly identified bone landmarks, they suggested that the gap balancing method may offer superior reliability when compared to the transepicondylar or AP axes. In an in vivo study of flexion and extension gaps in 84 TKAs using the gap balancing technique, Griffin et al.13) found that none of the evaluated knees demonstrated a flexion versus extension gap difference more than 3 mm. In 90% of 38 randomly selected mobile-bearing gap balanced TKAs, Boldt et al.14) found that the posterior condylar angle was within three degrees of the surgical TEA when measured with a spiral computed tomography (CT) scan.
Dennis et al.15) compared the stability of 40 measured resection TKAs and 20 gap balanced TKAs. The presence and magnitude of femoral condylar lift-off was evaluated for each technique at 0, 30, 60, and 90 degrees of flexion using an automated 3-dimensional model fitting kinematic analysis. A gap balancing technique exhibited a much lower incidence of condylar lift-off greater than 1.0 mm (p < 0.0001). Using a measured resection technique, condylar lift-off greater than 1.0 mm was seen in 12 of 20 (60%) of posterior cruciate retaining (PCR) TKAs and nine of 20 (45%) of posterior stabilized (PS) TKAs performed using a measured resection technique. None of the posterior stabilized TKA performed using gap balancing (0 of 20; 0%) had condylar lift-off greater than 1.0 mm. The gap balancing technique also had a lower maximum magnitude of femoral condylar lift-off (0.9 mm) than either of the two measured resection groups (PCR, 3.1 mm; PS TKA, 2.5 mm; p = 0.0002).
A precise proximal tibial resection is critical when using a gap balancing technique. A varus tibial resection will result in increased internal rotation of the femoral component when the femoral component is placed parallel to the resected proximal tibia. Correspondingly, a valgus tibial cut will lead to excessive external rotation of the femoral component. Over- or under-resection of the femoral or tibial bone resections can lead to a mismatch of flexion and extension gap dimensions. The authors recommend distal femoral and proximal tibia resections that approximate the implant thickness. Over-resection of the distal femur results in an enlarged extension gap. Typically, a thicker tibia component is then used to accurately tension the extension gap. To avoid increased tension in the flexion gap, this error will necessitate over-resection of the posterior condyles of the femur and a subsequent reduction in posterior femoral offset. Under-resection of the proximal tibia also will lead to over-resection of the posterior femoral condyles to avoid increased tension in the flexion gap.
The integrity of the collateral ligaments and precise ligament balancing are critical components of the gap balancing technique. The superficial medial collateral ligament is the primary stabilizer of the medial aspect of the flexion gap. The lateral aspect of the flexion gap is stabilized by the lateral collateral ligament and popliteus tendon. When the superficial medial tibial ligament is deficient, tensioning of the medial flexion gap will result in an excessive medial flexion gap. This will lead to excessive internal rotation if the femoral component is placed parallel to the resected tibia. When the lateral collateral ligament-popliteus tendon complex is deficient, positioning the femoral component parallel to the resected tibia can result in excessive external rotation.
Bony landmarks such as the TEA,16,17) the AP axis,18,19) and the posterior condylar axis20,21) are used to set femoral component rotation when using a measured resection technique. Unlike gap balancing, bone cuts are initially made independent of soft tissue tension.8) This section will describe the advantages and disadvantages of using the TEA, the AP axis, and the posterior condylar axis to set femoral rotation.
The TEA is a line connecting the prominence of the lateral epicondyle to the medial epicondylar ridge (clinical TEA) or the medial epicondylar sulcus (surgical TEA) (Fig. 8).16,22) Approximating the flexion-extension axis of the knee, the TEA corresponds to the femoral collateral ligamentous origin.22) According to Berger et al.,16) the surgical TEA can be a useful landmark in determining the native neutral rotational orientation of the femoral component. Enhanced central patellofemoral tracking and improved femorotibial kinematics can be obtained by placing the femoral component parallel to the TEA.23-26) A lower incidence and magnitude of femoral condylar lift-off (better coronal stability) was demonstrated by Insall et al.26) if the femoral component was placed parallel to the TEA axis in a kinematic analysis. Placement of the femoral component parallel to the TEA assists in obtaining a rectangular flexion gap (90% using the TEA, 83% using the AP axis, and 70% using the posterior condylar axis) in an analysis performed by Olcott and Scott25) The TEA can also be referenced in revision TKA and in Primary TKA where there is posterior condylar hypoplasia or erosion.
Unfortunately, numerous studies report that surgeons may be unable to accurately and reproducibly identify the TEA. Locating the medial and lateral epicondyles precisely is often difficult to reproduce intraoperatively.17,27-29) Jerosch et al.28) compared the difference in position of epicondyles marked by surgeons under experimental conditions. They demonstrated that the range of position chosen by the surgeons on the medial side varied 22.3 mm. They found that the range of position on the lateral epicondyle also varied by 13.8 mm. In a series of 74 TKA, Kinzel et al.29) studied the accuracy of epicondylar identification. Intraoperatively, they placed pins in the femoral epicondyles. When evaluated with postoperative CT scans, the epicondyles were correctly identified to within ± 3° in only 75% of the cases. They noted a wide range of error (six degrees of external rotation to 11 degrees of internal rotational error) and concluded that the TEA was an unreliable landmark to determine femoral component rotation. When the TEA was used to determine femoral component rotation, Yau et al.30) found that 56% of the time a range of error greater than five degrees occurred. They also noted a wide range of error in intraoperative surgeon identification of the femoral epicondyles (28 degree error range; 11 degrees external rotation to 17 degrees of internal rotation). In a cadaveric study using an imageless computer navigation system, Siston et al.31) compared the use of the posterior condylar, AP, and transepicondylar axes to set femoral component rotation. Only 17% of the actual registered landmarks fell within five degrees of the true epicondylar axis. Each of the 11 surgeons who participated in the study registered landmarks that tended to overly externally rotate the femoral component relative to the true TEA. Benjamin32) found that the TEA was only accurate to within one degree 34% of the time. The posterior condylar axis most frequently corresponded to the rotation alignment of the implanted femoral component, falling within ± 1° in 62% of the patients. They found that the AP axis was accurate only 26% of the time.
The AP axis has been used to set femoral rotation. This is a line that transects the center of the trochlear sulcus anteriorly and the midpoint of the posterior aspect of the intercondylar notch (Fig. 8). It is dependent on normal anatomy of the trochlear groove and intercondylar notch of the distal femur.12) Arima et al.33) evaluated patients whose femoral component rotation was determined based on the posterior condylar axis versus placement of the femoral component perpendicular to the AP axis. They found that patellofemoral problems were significantly reduced in knees in which the femoral component was positioned perpendicular to the AP axis as compared with knees in which the femoral component was placed parallel to the posterior condylar axis. Unlike the posterior condylar axis, the AP axis can also be utilized in cases of posterior condylar bone erosion or hypoplasia. Some surgeons have demonstrated that there is a wide range of error when the AP axis is used as the sole determinant of femoral component rotation. In a study of 100 arthritic knees, Poilvache et al.18) found that severe trochlear dysplasia resulted in excessive external rotation of the femoral component. Nagamine et al.34) noted that the line perpendicular to the AP axis in normal knees was externally rotated 3.5 degrees relative to the posterior condylar axis in a study of CT scans of 84 knees. They found that the line perpendicular to the AP axis was rotated externally more in knees with medial femorotibial osteoarthritis compared with normal knees. This indicated that the patellar groove was directed distally and medially. They therefore suggested isolated use of the AP axis to determine femoral component rotation in subjects with medial osteoarthritic knees may result in excessive external rotation of the femoral component and subsequent coronal plane instability in flexion. In another study by Yau et al.30) which based femoral component rotation on the AP axis, a 32 degrees range of error (15 degrees external rotation to 17 degrees of internal rotation) was found.
The posterior condylar axis refers to a line along the posterior aspect of the femoral condyles. When there is normal posterior condylar anatomy, a slight relative external rotation of three or four degrees relative to the posterior condylar axis will orient the AP femoral bone resections perpendicular to the resected tibial surface. A perpendicular tibial cut to the mechanical axis removes the normal three degree varus alignment of the articular surface of the tibia. Externally rotating the femur three degrees will therefore assist in stabilizing the lateral flexion gap.35) In neutral and varus knees with minimal deformity and no femoral bone erosion, instrumentation has been developed to assure a preselected amount (3°-5°) of external rotation relative to the posterior condylar axis. This instrumentation is simple and usually accurate (Fig. 9). As long as the posterior condyles were not eroded, Laskin and Rieger36) felt they were a good landmark to assist in determination of femoral component rotation. In another study, Hungerford and Krackow37) recommended first using posterior femoral condylar axis in primary TKA to rotationally align the femoral component and then secondarily checking that rotation with the TEA.
Despite the apparent simplicity of using instrumentation based on the posterior condylar axis to set femoral component rotation, there are disadvantages to this technique. Fundamentally, the anatomy of each femur is different. The decision to externally rotate the cutting guides three to four degrees in relation to the posterior condylar axis to set femoral rotation was derived from mean data. While externally rotating the femur three or four degrees may be accurate in a majority of cases, there are definite outliners. Poilvache et al.18) measured the angles between the tangent line of the posterior condylar surfaces, the AP axis described by Whiteside,19) and the transepicondylar line in 100 knees undergoing TKA. They found a range of -1 to 7 degrees of external rotation between the epicondylar line and the posterior condylar line. Mantas et al.20) reported that in normal cadaveric femurs, the TEA varied from 0.1 to 9.7 degrees externally rotated compared to the posterior condylar axis. They found an average external rotation of five degrees. Because of this wide anatomic variation in the relationship of the posterior condylar axis to the TEA, a significant percentage of patients would incur greater than two degrees of malrotation (femoral component internal rotation) relative to the TEA if the femoral component were automatically rotated three degrees with regard to the posterior condyles.17) For example, if a patient's anatomical TEA is eight degrees externally rotated compared to the posterior condylar line and instrumentation is used which places the femoral component in three degrees of external rotation relative to the posterior condylar line, the femoral component will still be internally rotated five degrees relative to the TEA.15)
It is difficult to rely on the posterior condylar axis to set rotation in arthritic deformities and with knee revisions.38) In a valgus knee deformity, there commonly is hypoplasia or erosion of the posterior aspect of the lateral femoral condyle. If the posterior condylar axis is used as the primary determinate of femoral component rotation, this will lead to erroneous femoral component internal rotation.39) In varus knees with chronic insufficiency of the anterior cruciate ligament, the posterior aspect of the medial femoral condyle is often eroded. This can lead to placement of the femoral component in excessive external rotation if the posterior condylar axis is used. In 100 TKAs implanted using computer navigation, Schnurr et al.21) noted that a rectangular flexion gap would have been obtained in only 51% of the cases if the posterior condylar axis had been utilized to determine femoral component rotation. Fehring11) noted femoral rotational errors of at least three degrees in 45% of patients when comparing measured resection techniques (using fixed bony landmarks such as the posterior condyle for rotational positioning) to gap balancing techniques.
In summary, substantial error can occur when measured resection bone landmarks are used to determine femoral component rotation due to variations in femoral anatomy. It is important to utilize all bone landmarks available to determine femoral component rotation.
Currently, measured resection and gap balancing techniques can be used to establish femoral component rotation and a rectangular flexion gap. Review of the literatures suggests that while measured resection techniques can be accurate in a majority of cases, utilization of this technique exclusively often results in flexion gap asymmetry and an increased incidence of femoral condylar lift-off. The surgeon's ability to reproducibly identify the bone landmarks accurately used in measured resection techniques is limited. Because the gap balancing technique is less dependent bony anatomy, we feel that it can be used to provide more reproducible flexion gap stability.
Figures and Tables
Fig. 1
Intraoperative photograph of a flexion gap tensioning jig placed into the flexion gap, tensioning the gap, and positioned parallel to the transepicondylar axis before the anterior and posterior femoral resections are performed (Courtesy of Robert E. Booth, MD).

Fig. 2
Intraoperative photograph demonstrating a tensioning jig placed into the extension gap with an extramedullary guide used to determine alignment and width of the distal femoral resection (Courtesy of Robert E. Booth, MD).

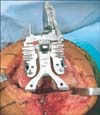
Fig. 3
(A) Intraoperative photograph demonstrating resection of 4 mm of the posterior aspect of the medial femoral condyle to gain access to posterior compartment osteophytes. (B) Photograph demonstrating how an osteotome with greater curvature allows for easier access to posterior femoral osteophytes than a traditional curved osteotome. (C) Intraoperative photograph demonstrating removal of posterior femoral osteophytes using a curved osteotome.

Fig. 4
Intraoperative photograph demonstrating assessment of lower extremity alignment and extension gap balance using a spacer block.

Fig. 5
Intraoperative photograph of the knee at 90 degrees of flexion and the collateral ligaments equally tensioned using laminar spreaders. Note the transepicondylar axis is parallel and anterior-posterior axis is perpendicular to the resected proximal tibia.

Fig. 6
Intraoperative photograph demonstrating placement of the anteroposterior femoral cutting block parallel to the resected proximal tibia with each collateral ligament tensioned to create a rectangular flexion gap.

Fig. 7
Intraoperative photograph demonstrating placement of a spacer block (same width as utilized in creation of the extension gap) into the flexion gap to assure appropriate width before performing the anterior and posterior femoral condylar resections.

References
1. Laskin RS. Flexion space configuration in total knee arthroplasty. J Arthroplasty. 1995; 10(5):657–660.
2. Scuderi GR, Komistek RD, Dennis DA, Insall JN. The impact of femoral component rotational alignment on condylar lift-off. Clin Orthop Relat Res. 2003; (410):148–154.
3. Berger RA, Crossett LS, Jacobs JJ, Rubash HE. Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res. 1998; (356):144–153.
4. Boldt JG, Stiehl JB, Hodler J, Zanetti M, Munzinger U. Femoral component rotation and arthrofibrosis following mobile-bearing total knee arthroplasty. Int Orthop. 2006; 30(5):420–425.
5. Incavo SJ, Wild JJ, Coughlin KM, Beynnon BD. Early revision for component malrotation in total knee arthroplasty. Clin Orthop Relat Res. 2007; 458:131–136.
6. Romero J, Stahelin T, Binkert C, Pfirrmann C, Hodler J, Kessler O. The clinical consequences of flexion gap asymmetry in total knee arthroplasty. J Arthroplasty. 2007; 22(2):235–240.
7. Insall JN, Scott WN. Insall & Scott surgery of the knee. 4th ed. Philadelphia: Church Livingstone/Elsevier;2006.
8. Lotke PA, Lonner JH. Knee arthroplasty. 3rd ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins;2009.
9. Heesterbeek PJ, Jacobs WC, Wymenga AB. Effects of the balanced gap technique on femoral component rotation in TKA. Clin Orthop Relat Res. 2009; 467(4):1015–1022.
10. Dennis DA. Measured resection: an outdated technique in total knee arthroplasty. Orthopedics. 2008; 31(9):940943–944.
11. Fehring TK. Rotational malalignment of the femoral component in total knee arthroplasty. Clin Orthop Relat Res. 2000; (380):72–79.
12. Katz MA, Beck TD, Silber JS, Seldes RM, Lotke PA. Determining femoral rotational alignment in total knee arthroplasty: reliability of techniques. J Arthroplasty. 2001; 16(3):301–305.
13. Griffin FM, Insall JN, Scuderi GR. Accuracy of soft tissue balancing in total knee arthroplasty. J Arthroplasty. 2000; 15(8):970–973.
14. Boldt JG, Stiehl JB, Munzinger U, Beverland D, Keblish PA. Femoral component rotation in mobile-bearing total knee arthroplasty. Knee. 2006; 13(4):284–289.
15. Dennis DA, Komistek RD, Kim RH, Sharma A. Gap balancing versus measured resection technique for total knee arthroplasty. Clin Orthop Relat Res. 2010; 468(1):102–107.
16. Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res. 1993; (286):40–47.
17. Griffin FM, Math K, Scuderi GR, Insall JN, Poilvache PL. Anatomy of the epicondyles of the distal femur: MRI analysis of normal knees. J Arthroplasty. 2000; 15(3):354–359.
18. Poilvache PL, Insall JN, Scuderi GR, Font-Rodriguez DE. Rotational landmarks and sizing of the distal femur in total knee arthroplasty. Clin Orthop Relat Res. 1996; (331):35–46.
19. Whiteside LA, Arima J. The anteroposterior axis for femoral rotational alignment in valgus total knee arthroplasty. Clin Orthop Relat Res. 1995; (321):168–172.
20. Mantas JP, Bloebaum RD, Skedros JG, Hofmann AA. Implications of reference axes used for rotational alignment of the femoral component in primary and revision knee arthroplasty. J Arthroplasty. 1992; 7(4):531–535.
21. Schnurr C, Nessler J, Konig DP. Is referencing the posterior condyles sufficient to achieve a rectangular flexion gap in total knee arthroplasty? Int Orthop. 2009; 33(6):1561–1565.
22. Aglietti P, Sensi L, Cuomo P, Ciardullo A. Rotational position of femoral and tibial components in TKA using the femoral transepicondylar axis. Clin Orthop Relat Res. 2008; 466(11):2751–2755.
23. Diduch DR, Insall JN, Scott WN, Scuderi GR, Font-Rodriguez D. Total knee replacement in young, active patients: long-term follow-up and functional outcome. J Bone Joint Surg Am. 1997; 79(4):575–582.
24. Miller MC, Berger RA, Petrella AJ, Karmas A, Rubash HE. Optimizing femoral component rotation in total knee arthroplasty. Clin Orthop Relat Res. 2001; (392):38–45.
25. Olcott CW, Scott RD. A comparison of 4 intraoperative methods to determine femoral component rotation during total knee arthroplasty. J Arthroplasty. 2000; 15(1):22–26.
26. Insall JN, Scuderi GR, Komistek RD, Math K, Dennis DA, Anderson DT. Correlation between condylar lift-off and femoral component alignment. Clin Orthop Relat Res. 2002; (403):143–152.
27. Hatayama K, Terauchi M, Higuchi H, Yanagisawa S, Saito K, Takagishi K. Relationship between femoral component rotation and total knee flexion gap balance on modified axial radiographs. J Arthroplasty. 2011; 26(4):649–653.
28. Jerosch J, Peuker E, Philipps B, Filler T. Interindividual reproducibility in perioperative rotational alignment of femoral components in knee prosthetic surgery using the transepicondylar axis. Knee Surg Sports Traumatol Arthrosc. 2002; 10(3):194–197.
29. Kinzel V, Ledger M, Shakespeare D. Can the epicondylar axis be defined accurately in total knee arthroplasty? Knee. 2005; 12(4):293–296.
30. Yau WP, Chiu KY, Tang WM. How precise is the determination of rotational alignment of the femoral prosthesis in total knee arthroplasty: an in vivo study. J Arthroplasty. 2007; 22(7):1042–1048.
31. Siston RA, Patel JJ, Goodman SB, Delp SL, Giori NJ. The variability of femoral rotational alignment in total knee arthroplasty. J Bone Joint Surg Am. 2005; 87(10):2276–2280.
32. Benjamin J. Determining femoral component position using CAS and measured resection. Clin Orthop Relat Res. 2008; 466(11):2745–2750.
33. Arima J, Whiteside LA, McCarthy DS, White SE. Femoral rotational alignment, based on the anteroposterior axis, in total knee arthroplasty in a valgus knee: a technical note. J Bone Joint Surg Am. 1995; 77(9):1331–1334.
34. Nagamine R, Miura H, Inoue Y, et al. Reliability of the anteroposterior axis and the posterior condylar axis for determining rotational alignment of the femoral component in total knee arthroplasty. J Orthop Sci. 1998; 3(4):194–198.
35. Bottros J, Gad B, Krebs V, Barsoum WK. Gap balancing in total knee arthroplasty. J Arthroplasty. 2006; 21:4 Suppl 1. 11–15.
36. Laskin RS, Rieger MA. The surgical technique for performing a total knee replacement arthroplasty. Orthop Clin North Am. 1989; 20(1):31–48.
37. Hungerford DS, Krackow KA. Total joint arthroplasty of the knee. Clin Orthop Relat Res. 1985; (192):23–33.
38. Pagnano MW, Hanssen AD. Varus tibial joint line obliquity: a potential cause of femoral component malrotation. Clin Orthop Relat Res. 2001; (392):68–74.
39. Griffin FM, Insall JN, Scuderi GR. The posterior condylar angle in osteoarthritic knees. J Arthroplasty. 1998; 13(7):812–815.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download