This article has been corrected. See "Erratum to "Inflammatory Responses in the Muscle Coat of Stomach and Small Bowel in the Postoperative Ileus Model of Guinea Pig" by Choi HK, et al. (Yonsei Med J 2013;54:1336-41.)" in Volume 55 on page 549.
Abstract
Purpose
Small intestinal function returns first after surgery, and then the function of the stomach returns to normal after postoperative ileus (POI). The aim of this study was to investigate inflammatory responses in the muscle coat of stomach and small intestine in guinea pig POI model.
Materials and Methods
The distance of charcoal migration from pylorus to the distal intestine was measured. Hematoxylin and eosin (H&E) and immunohistochemical stain for calprotectin were done from the histologic sections of stomach, jejunum and ileum obtained at 3 and 6 hour after operation. Data were compared between sham operation and POI groups.
Results
The distance of charcoal migration was significantly reduced in the 3 and 6 hour POI groups compared with sham operated groups (p<0.05). On H&E staining, the degree of inflammation was significantly higher in the stomach of 3 hour POI groups compared with jejunum and ileum of POI groups or sham operated groups (p<0.05). Calprotectin positive cells were significantly increased in the muscle coat of stomach of 3 hour POI groups compared with jejunum and ileum of POI groups or sham operated groups (p<0.05). There was strong association between the degree of inflammation and calprotectin positive cells in stomach.
Conclusion
Postoperative ileus induced by cecal manipulation significantly increased the degree of inflammation and calprotectin positive cells in the muscle coat of stomach as a remote organ. The relevance of degree of inflammation and the recovery time of ileus should be pursued in the future research.
Postoperative ileus (POI) is characterized by a transiently impaired propulsive function of the entire gastrointestinal tract after abdominal surgery.1 Most of patients who had abdominal surgeries may suffer from ileus, and it is a temporary condition which lasts for about 3-5 days.2 The prevention of post-operative ileus is an important matter because ileus have a negative impact on the quality of life and are related to the delayed return to the social activity and increased medical bills.3,4 To date, there is no approved medication to prevent or to treat post-operative ileus. The basic clinical trials are being conducted, however, the results are not yet satisfactory.2,5
Five main theories on the mechanism of postoperative ileus have been proposed. The activation of inhibitory spinal and inhibitory sympathetic reflexes, anesthesia, humoral agents, and inflammation have been implicated as causes.6 Inflammation theory has received the most attention among all the five theories. Even the minimal touch of the small intestine activates inflammatory processes within the muscle coat of the intestinal wall. When resident macrophages are activated, phosphorylation of transcription factors results in the release of chemokines, nitric oxide (NO) and prostaglandins. This inflammatory processes cause the upregulation of adhesion molecules, that recruits leukocytes into the muscle coat.7-10
Calprotectin is usually expressed in neutrophils and macrophages whereas it is not mostly present in lymphocytes. In calprotectin expression, activated macrophages and monocytes in acute inflammation are positive, while resident macrophages and macrophages in chronic inflammation are negative.11-13
To date, most of the studies on the inflammatory responses in the intestinal muscle coat of ileus models have been focused on jejunum and ileum, and there has been no report on the inflammatory responses in the muscle coat of stomach and small intestine according to different time points in guinea pig POI model. The aim of this study was to investigate inflammatory responses in the muscle coat of stomach and small intestine in guinea pig POI model.
Hartley breed 4 week old healthy male guinea pigs, weighting 300-330 g, were used. The breeding condition was 20-22℃ temperature, 50% humidity and the lighting was regulated in 12 hour cycle (07:00-19:00) by fluorescent lights. The protocol was approved by the Department of Laboratory Animal Medicine, Medical Research Center, Yonsei University College of Medicine and followed animal experiment guideline.
The subjects were in fasting state except water until 24 hours prior to the operation. Pentobarbital sodium (40 mg/kg) was injected into their abdominal cavities. After anesthesia took effects completely, the abdominal hair was shaved. The subjects in the control group were stunned by being hit on the occipital area and were bled by dissecting the carotid artery (n=3). The skin and the muscle coat were incised after cleaning the area with alcohol gauze, and a minimal incision was done to the peritoneum. Some of the subjects had their incised portion closed without any bowel manipulations (sham operation group, n=15), whereas others were closed after being rubbed with wet gauze for 1 minute gently with cecum taken out (POI group, n=16). No parts of bowel had been touched except for the cecum. Then, guinea pigs recovered in the breeding environments.
Charcoal was administered through orogastric tube to evaluate gastric and bowel movement. Barium, charcoal and normal saline were mixed in the ratio of 2 : 1 : 6 for the use. The subjects were stunned by being hit on the occipital area and bled by dissecting their carotid arteries at 3 or 6 hour after charcoal was administered. The distance of charcoal migration from pylorus was measured and compared between sham-operated and POI groups.
H&E staining was done with the histologic sections obtained from the muscle coat of stomach, jejunum and ileum at 3 and 6 hour after operation. We compared the degree of inflammation between the sham-operated and POI groups at different time intervals. To evaluate the degree of inflammation, a semi-quantitative scoring scale14 from 0 to 3 was utilized, 0, being non inflamed; 1, very mildly inflamed; 2, mildly inflamed; 3, inflamed. These histologic sections were scored by Park JP, pathologist.
The histologic sections of stomach, jejunum and ileum at 3 and 6 hour after operation were dissected and fixed in 4% formaldehyde. This paraffin block was cut at 4 µm thickness and mounted onto poly-L-lysine-coated slides. For deparaffinization, the fixed paraffin-embedded section was dehydrated successively with xylene for 9 min and then the tissue was rehydrated with 100%, 90% and 70% alcohol, and heated in a microwave oven for 10 min to retrieve antigen, after which the section was cooled at room temperature. The slide was rinsed with 0.02 mol L-1 phosphate-buffered saline (PBS) for 10 min. Endogenous peroxidase activity in the tissue section was blocked by incubation for 10 min in a solution of H2O2 (3%) at room temperature, followed by 10 min washing with PBS. A protein block solution (DAKO, Carpinteria, CA, USA) was added for 30 min. The tissue was incubated overnight at 4℃ with calprotectin-monocyte/macrophage/L1 protein Ab-1 (1 : 1000; Lab Vision, Fremont, CA, USA) as a primary antibody. The section was washed again with PBS and incubated along with anti-mouse as a secondary antibody. After washing with PBS, the section was then incubated with streptavidin-horseradish peroxide, for 30 min at room temperature. Finally, the section was washed with PBS for 10 min. The section was put on the DAB-peroxidase solution for about 1-3 min and counterstained with haematoxylin. The numbers of positive cells in the muscle coat were counted by i-solution program (IMT, Daejeon, Korea): They were counted at five randomly chosen areas in each slides at a magnification of 400× (cells/400× field). We used spleen tissues as a positive control, and compared it between the sham-operated groups and POI groups at two time points.
Data were expressed as mean±standard error. Data analysis was done using SPSS software (19th version, SPSS Inc., Chicago, IL, USA). Data were analyzed using independent t-test. Correlation between the degree of inflammation and calprotectin positive cells was assessed using Pearson.s correlation test. p value <0.05 was considered as significant.
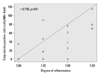
The distance of charcoal migration was reduced significantly in the 3 hour POI groups (n=8) compared with the sham operated groups (n=7) (7.25±2.09 cm vs. 99.07±16.78 cm, p<0.05). The distance of charcoal migration was reduced significantly in the 6 hour POI groups (n=8) compared with the sham operated groups (n=8) (48.88±5.02 cm vs. 116.25±11.27 cm, p<0.05) (Fig. 1).
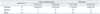
The degree of inflammation was significantly higher in the stomach of the 3 hour POI compared with sham-operated groups (p<0.05). Furthermore, the degree of inflammation was significantly higher in the stomach of the 3 and 6 hour POI groups compared with jejunum and ileum of POI groups (p<0.05). However, the degree of inflammation in the stomach of the 3 hour POI groups was not significantly different from that of the 6 hour POI groups (Table 1).
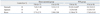
Calprotectin positive cells were significantly increased in the 3 hour POI compared with the sham-operated groups (53.63±16.40 vs. 7.43±5.18 cells/400× field, p<0.05). Calprotectin positive cells were significantly increased in the stomach of 3 hour POI groups compared with jejunum and ileum of POI groups (p<0.05). However, calprotectin positive cells in the 3 hour POI groups were not significantly different from those of 6 hour POI groups (Table 2).
Calprotectin positive cells in the 3 and 6 hour POI groups were not significantly different from the sham-operated groups. Calprotectin positive cells in the 3 hour POI groups were not significantly different from the 6 hour POI groups (Table 2).
Degree of inflammation was strongly associated with calprotectin positive cells in stomach (r=0.730, p<0.01) (Fig. 2).
There are two significances in this study. First, this study analyzed the degree of inflammatory responses in the stomach. To date, most of previous studies on the inflammatory responses of ileus have been focused on small intestine, especially on jejunum and ileum. Furthermore, earlier studies8,16 suggested that inflammatory infiltrate is confined only to the manipulated small intestine, therefore, it was a surprise to find that the degree of inflammation and calprotectin positive cells were significantly increased in the stomach of 3 hour groups, but not in jejunum and ileum. Second, this study would help to understand the characteristics of early stage inflammatory responses by comparing calprotectin positive cells in 3 hour and in 6 hour.
The degree of inflammation was analyzed twice; in 3 hour and in 6 hour. In our previous study, the ileus degree assessed by a simple radiograph was found to be maximal at 3 hour and recovered at 6 hour in POI groups.7 This is the reason of why the comparison in 3 hour and 6 hour is considered to be the best to understand early stage inflammatory characteristics within 24 hour.
The muscularis macrophages were negative for the activation marker lymphocyte function associated antigen-1 at 1 hour after operation, but intensively positive at 3 hour after operation.6 The inflammatory mediators and cytokines reach the highest point in 3-4 hour and reduced afterwards. Our data are consistent with previous study6 and contribute to the understanding of characteristics of early stage inflammatory responses in the muscle coat.
Neutrophilic infiltrates at 24 hour after operation in fixed whole mounts of the manipulated jejunum, stomach, and colon of rat were found to be 64.4±5.0, 18.1±6.2, and 22.4±5.6 myeloperoxidase+ cells/field at 200× magnification, respectively.17 Control whole mounts had only 2.2±0.5, 1.8±0.8, and 2.9±0.8 respectively. In this study, jejunal neutrophilic infiltrates were significantly higher than those of stomach and colon. There are three differences between this study17 and our study. First, our study manipulated cecum whereas this study manipulated jejunum. Most of earlier studies8,16,17 manipulated jejunum and investigated the same organ. However, our study manipulated only cecum and investigated stomach, jejunum, and ileum. Second, our study used guinea pigs while they used rats. Guinea pigs are more similar to human in neuromuscular physiology of gut than rat or mouse,18-20 therefore, we chose guinea pigs. To our best knowledge, our study is the first one that compared inflammation between stomach and small intestine in guinea pigs. Third, our study investigated at 3 hour and 6 hour after operation, but they investigated at 24 hour after operation. These differences could make significant discrepancy between our study and previous studies.8,16,17
CCR9+ plasmacytoid dendritic cells in small intestine could affect the degree of inflammation and calprotectin positive cells in our study.21,22 CCR9+ plasmacytoid dendritic cells reside in small intestine, but not in colon. They are critically involved in immunological homeostasis in small intestine and suppress development of inflammation in mice.22
In rat, manipulation of colon results in activation of inflammatory mediators such as interleukin 6, inducible nitric oxide synthase (iNOS).23,24 Mast cell in the peritoneal cavity may promote the translocation of bacterial products and causes more general inflammatory processes. This occurs during a short time window within 3-4 h after manipulation.25,26 Therefore, bacterial translocation could affect, in the 3 hour POI group, why quantities of inflammatory cells in stomach were more than small intestine.
In our study, the degree of inflammation was strongly associated with calprotectin positive cells in stomach. Fecal calprotectin is a promising marker of neutrophilic intestinal inflammation.27,28 It has been consistently shown to be elevated in patients with known irritable bowel disease (IBD), and has an excellent negative predictive value in ruling out IBD in underdiagnosed, symptomatic patients. Fecal calprotectin correlates well with severity of inflammation, as judged by both endoscopic and histological scoring system.29 This study supports our present study in that calprotectin correlates well with degree of inflammation.
The late phase of postoperative ileus after bowel handling results from inflammatory responses in the muscule coat of small intestine.8 Although this theory can explain the impaired motility of small intestine, it can't explain impaired motility of stomach and colon. The late phase of postoperative ileus after intestinal manipulation is mediated by an inhibitory enterogastric neural pathway that is triggered by inflammatory infiltrate recruited in the intestinal muscularis.16 They proposed that inflammatory infiltrate is confined to the manipulated small intestine, focused on the fact that inflammation theory can't explain the hypomotility of untouched parts of the gastrointestinal tract. However, this theory also can't explain why small intestine recovers earlier than stomach.
In our present study, the degree of inflammation and calprotectin positive cells were significantly increased in the stomach of 3 hour POI group compared with sham operated groups or jejunum and ileum. When the resident muscularis macrophages are activated, arachidonic acid, activated oxides, hormones, NO, prostaglandins, and cytokines are synthesized and released. Among these, NO and prostaglandins can directly regulate the bowel movement.30-32 If a large amount of macrophages are activated, the synthesis of NO and prostaglandins will increase and affect the bowel movement.
The recovery periods from the ileus varied depending on the organ. Small intestinal function returns first, as early as within 24 hours after surgery, then the function of stomach returns to normal in 24 to 48 hours, and finally that of colon returns to normal in 48 to 72 hours.33 It was found that the imperative quantities of inflammatory cells could play a role in determining the recovery time from ileus, although we didn.t analyze temporal relationship between the degree of inflammation and the recovery time from ileus. The relevance of the degree of inflammation and recovery time from ileus should be pursued in the future research. In the present study, we compared stomach and small intestine only. We think that comparison of stomach, small intestine and colon in the future research may be fruitful.
Figures and Tables
Fig. 1
Distances of charcoal migration of POI and sham operation groups. The distance of charcoal migration was reduced significantly in the 3 hour POI groups (n=8) compared with sham operation groups (n=7) (7.25±1.76 cm vs. 99.07±16.78 cm). The distance of charcoal migration was reduced significantly in the 6 hour POI groups (n=8) compared with sham operation groups (n=8) (40.63±5.99 cm vs. 116.25±11.27 cm).

References
3. Collins TC, Daley J, Henderson WH, Khuri SF. Risk factors for prolonged length of stay after major elective surgery. Ann Surg. 1999; 230:251–259.

4. Longo WE, Virgo KS, Johnson FE, Oprian CA, Vernava AM, Wade TP, et al. Risk factors for morbidity and mortality after colectomy for colon cancer. Dis Colon Rectum. 2000; 43:83–91.

5. Lim HC, Chon NR, Choi EJ, Lee YH, Lee MG, Park H. The effect of itopride hydrochloride on the gastrointestinal motility in postoperative ileus of guinea pigs. Korean J Neurogastroenterol Motil. 2008; 14:18–23.
6. Kalff JC, Türler A, Schwarz NT, Schraut WH, Lee KK, Tweardy DJ, et al. Intra-abdominal activation of a local inflammatory response within the human muscularis externa during laparotomy. Ann Surg. 2003; 237:301–315.

8. Kalff JC, Schraut WH, Simmons RL, Bauer AJ. Surgical manipulation of the gut elicits an intestinal muscularis inflammatory response resulting in postsurgical ileus. Ann Surg. 1998; 228:652–663.

9. Kalff JC, Carlos TM, Schraut WH, Billiar TR, Simmons RL, Bauer AJ. Surgically induced leukocytic infiltrates within the rat intestinal muscularis mediate postoperative ileus. Gastroenterology. 1999; 117:378–387.

10. Kalff JC, Schraut WH, Billiar TR, Simmons RL, Bauer AJ. Role of inducible nitric oxide synthase in postoperative intestinal smooth muscle dysfunction in rodents. Gastroenterology. 2000; 118:316–327.

11. Zwadlo G, Brüggen J, Gerhards G, Schlegel R, Sorg C. Two calcium-binding proteins associated with specific stages of myeloid cell differentiation are expressed by subsets of macrophages in inflammatory tissues. Clin Exp Immunol. 1988; 72:510–515.
12. Bhardwaj RS, Zotz C, Zwadlo-Klarwasser G, Roth J, Goebeler M, Mahnke K, et al. The calcium-binding proteins MRP8 and MRP14 form a membrane-associated heterodimer in a subset of monocytes/macrophages present in acute but absent in chronic inflammatory lesions. Eur J Immunol. 1992; 22:1891–1897.

13. Lagasse E, Weissman IL. Mouse MRP8 and MRP14, two intracellular calcium-binding proteins associated with the development of the myeloid lineage. Blood. 1992; 79:1907–1915.

14. The FO, Bennink RJ, Ankum WM, Buist MR, Busch OR, Gouma DJ, et al. Intestinal handling-induced mast cell activation and inflammation in human postoperative ileus. Gut. 2008; 57:33–40.

15. Kim HS, Choi EJ, Park H. The effect of mosapride citrate on proximal and distal colonic motor function in the guinea-pig in vitro. Neurogastroenterol Motil. 2008; 20:169–176.

16. de Jonge WJ, van den Wijngaard RM, The FO, ter Beek ML, Bennink RJ, Tytgat GN, et al. Postoperative ileus is maintained by intestinal immune infiltrates that activate inhibitory neural pathways in mice. Gastroenterology. 2003; 125:1137–1147.

17. Schwarz NT, Kalff JC, Türler A, Speidel N, Grandis JR, Billiar TR, et al. Selective jejunal manipulation causes postoperative pan-enteric inflammation and dysmotility. Gastroenterology. 2004; 126:159–169.

18. McConnell EL, Basit AW, Murdan S. Measurements of rat and mouse gastrointestinal pH, fluid and lymphoid tissue, and implications for in-vivo experiments. J Pharm Pharmacol. 2008; 60:63–70.

19. Kendall RA, Alhnan MA, Nilkumhang S, Murdan S, Basit AW. Fabrication and in vivo evaluation of highly pH-responsive acrylic microparticles for targeted gastrointestinal delivery. Eur J Pharm Sci. 2009; 37:284–290.

20. Merchant HA, McConnell EL, Liu F, Ramaswamy C, Kulkarni RP, Basit AW, et al. Assessment of gastrointestinal pH, fluid and lymphoid tissue in the guinea pig, rabbit and pig, and implications for their use in drug development. Eur J Pharm Sci. 2011; 42:3–10.

21. Papadakis KA, Prehn J, Nelson V, Cheng L, Binder SW, Ponath PD, et al. The role of thymus-expressed chemokine and its receptor CCR9 on lymphocytes in the regional specialization of the mucosal immune system. J Immunol. 2000; 165:5069–5076.

22. Mizuno S, Kanai T, Mikami Y, Sujino T, Ono Y, Hayashi A, et al. CCR9+ plasmacytoid dendritic cells in the small intestine suppress development of intestinal inflammation in mice. Immunol Lett. 2012; 146:64–69.

23. de Jonge WJ, van der Zanden EP, The FO, Bijlsma MF, van Westerloo DJ, Bennink RJ, et al. Stimulation of the vagus nerve attenuates macrophage activation by activating the Jak2-STAT3 signaling pathway. Nat Immunol. 2005; 6:844–851.

24. Bauer AJ. Mentation on the immunological modulation of gastrointestinal motility. Neurogastroenterol Motil. 2008; 20:Suppl 1. 81–90.

25. Schwarz NT, Beer-Stolz D, Simmons RL, Bauer AJ. Pathogenesis of paralytic ileus: intestinal manipulation opens a transient pathway between the intestinal lumen and the leukocytic infiltrate of the jejunal muscularis. Ann Surg. 2002; 235:31–40.
26. Türler A, Schnurr C, Nakao A, Tögel S, Moore BA, Murase N, et al. Endogenous endotoxin participates in causing a panenteric inflammatory ileus after colonic surgery. Ann Surg. 2007; 245:734–744.

27. Limburg PJ, Ahlquist DA, Sandborn WJ, Mahoney DW, Devens ME, Harrington JJ, et al. Fecal calprotectin levels predict colorectal inflammation among patients with chronic diarrhea referred for colonoscopy. Am J Gastroenterol. 2000; 95:2831–2837.

28. Costa F, Mumolo MG, Bellini M, Romano MR, Ceccarelli L, Arpe P, et al. Role of faecal calprotectin as non-invasive marker of intestinal inflammation. Dig Liver Dis. 2003; 35:642–647.

29. Konikoff MR, Denson LA. Role of fecal calprotectin as a biomarker of intestinal inflammation in inflammatory bowel disease. Inflamm Bowel Dis. 2006; 12:524–534.

30. Stark ME, Bauer AJ, Szurszewski JH. Effect of nitric oxide on circular muscle of the canine small intestine. J Physiol. 1991; 444:743–761.

31. van der Vliet A, Tuinstra TJ, Bast A. Modulation of oxidative stress in the gastrointestinal tract and effect on rat intestinal motility. Biochem Pharmacol. 1989; 38:2807–2818.

32. Petitclerc E, Levesque L, Grose JH, Poubelle PE, Marceau F. Pathologic leukocyte infiltration of the rabbit aorta confers a vasomotor effect to chemotactic peptides through cyclooxygenase-derived metabolites. J Immunol. 1996; 156:3426–3434.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download