INTRODUCTION
Snoring and obstructive sleep apnea (OSA) can induce excessive daytime sleepiness, increased risk of car accidents, and several cardiovascular and neurovascular medical complications.1) As the prevalence and socio-economic burden of OSA is steadily increasing each year, many researchers and clinicians have focused on its treatment.1)
Mainstream OSA treatments are continuous positive airway pressure (CPAP) and surgical intervention. CPAP, a so-called ‘pneumatic splint,’ can effectively treat apnea by preventing airway collapse with positive pressure.2)3) However, low long-term compliance is a major disadvantage of CPAP.4)5) A variety of surgical procedures have been developed, including uvulopalatopharyngoplasty; however, their success rates remain suboptimal at 60 to 70%.6)7) Therefore, new treatment strategies with high compliance rates and minimal morbidity are desired.
Some researchers have investigated the effects of mechanical dilation of the nasal valve area for the treatment of snoring and OSA. Nasal dilators could be classified into two groups: external dilators (EXDs) and endonasal dilators (ENDs). Typically, an EXD is applied to the external skin of the bilateral nasal alar area, whereas an END is inserted directly into the nostril. Both forms seek to dilate the nostril and nasal valve area. Although there are many commercially available EXDs and ENDs worldwide, most researchers have used Breathe Right® (GlaxoSmithKline, Middlesex, United Kingdom) for the EXD model and Nozovent® (Biorevive, Victoria, Australia) as the END model.8)9) Both have been reported to have beneficial effects, with decreased nasal resistance and improved airflow in the Western population.8)9) Ellegård suggested that the effects of END could be lower in non-Caucasian people because of anatomical differences.10) However, nearly all of these studies have focused on Caucasian populations and there have been very few studies on Asians.
Therefore, we sought to evaluate the effect of END in Asian patients with OSA by evaluating changes in (a) acoustic parameters such as the dimension and volume of the nasal cavity, (b) nasal airflow measured by peak nasal inspiratory flow (PNIF), (c) daytime sleepiness measured by the Epworth Sleepiness Scale (ESS) questionnaire, and finally (d) several parameters of portable polysomnography (PSG) such as the apnea-hypopnea index (AHI), respiratory distress index (RDI) and oxygen desaturation index (ODI) before and after wearing the END.
MATERIALS AND METHODS
Patients
Thirteen patients who suffered from snoring and OSA were enrolled in the study (11 males and 2 females, 33 to 59 years old). We included adult patients (20 to 65 years of age), who had been diagnosed as OSA (AHI >5 measured by portable polysomnography). We excluded those with significant co-morbidity such as coronary artery disease, unstable angina and also those with severe respiratory diseases such as chronic obstructive pulmonary disease. After nasal endoscopy, patients with chronic rhinosinusitis and/or nasal polyposis, severe septal deviation or severe tonsillar hypertrophy (grade IV) were also excluded. Ten of the enrolled patients complained of subjective nasal obstruction and three did not complain of nasal obstruction.
After obtaining informed consent, their height and weight was measured to calculate
Tonsil size (grade I to IV) and palate position (grade I to IV) was also determined in order to classify subjects according to Friedmann staging. They then completed the ESS questionnaire to determine baseline sleepiness score before any intervention. This study was approved by the institutional review board of our hospital. All patients were enrolled in this study after detailed explanation of the aims of this study and gave written informed consent.
Measurement of baseline acoustic parameters and PNIF
Before END application, acoustic rhinometry was performed to measure the volume and dimension of the nasal cavity, according to our previously published protocol.11)12) Briefly, patients waited 15 minutes in a room with a constant temperature (about 22℃) and humidity (about 50%) for acclimatization. Using the ECCOVISION acoustic rhinometer (E. Benson Hood Laboratories, MA, United States), we measured volume and dimensions inside the nasal cavity. We inserted a nose tip into the nostril, taking care not to change the shape of the nostril. The direction of the nose tip was parallel to the patient's sagittal plane, 45 degrees from the vertical line. Patients were encouraged to hold their breath for a short period (about 1 second) during the measurement. Total nasal volume (TNV) was defined as the summation of all cross-sectional areas from the nostril to 7-cm deep into the nasal cavity. Minimal cross-sectional area (MCA) was defined as the dimension with the smallest value.
The baseline PNIF was also measured as liter/minute in each patient using a portable nasal inspiratory flow meter (Clement Clarke International Ltd., UK). Patients were asked to breathe in with maximal effort with masks attached to their face.
Post-intervention ESS questionnaire, acoustic rhinometery and PNIF
Each patient was given an END donated by BANDYCO Co., Ltd. (Cheonan, Korea). We carefully chose the size of each END to fit and gently dilate the patient's nostrils without excessive tension or discomfort. Fig. 1 shows the shape and placement of the END.
Then, with the inserted END, acoustic rhinometry and PNIF measurements were repeated. Patients were asked to use the END for 14 consecutive days while sleeping. After 2 weeks, we repeated the ESS questionnaire to evaluate for any improvement in daytime sleepiness.
Portable PSG before and after END application
The portable Watch-PAT (peripheral arterial tone) 100 PSG machine (Itamar, Caesarea, Israel) was used for the sleep apnea study. AHI, RDI, ODI, sleep time, sleep position and loudness of snoring (in decibels) were evaluated before any intervention as a baseline value. After 2 weeks, patients were asked to insert the END and repeat the portable PSG.
RESULTS
END significantly improved nasal volume, dimension and inspiratory flow
The baseline data of the patients are summarized in Table 1. Baseline TNV and MCA were 11.4±3.1 cm3 and 0.7±0.2 cm2, respectively. After END use, these values significantly increased to 19.4±5.7 cm3 and 0.9±0.1 cm2 (p=0.001, respectively) (Fig. 2A and B).
Compared to baseline, PNIF also significantly increased after END application (147.3±39.5 L/min to 194.6±57.6 L/min, p=0.001) (Fig. 2C).
Improvement in daytime sleepiness
Among 13 patients, 2 patients dropped out and the remaining 11 patients agreed to a 14-day follow-up. Among these 11 patients, 7 (63.6%) reported some improvement in daytime sleepiness. Although the ESS score after 2 weeks of END use showed some improvement (10.7±4.3 to 10.1±4.6), this change was not statistically significant (p >0.05) (Fig. 3).
Demographic variables were compared between patients with an improvement in their ESS score (responsive group) and those without reported improvement (non-responsive group). Patients in the responsive group were significantly younger compared to those in the non-responsive group (43.7±7.8 years versus 54.5±4.7 years, p=0.038) (Fig. 4). There were no significant differences in the other variables such as BMI and Friedmann staging.
Change in PSG parameters after END use
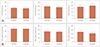
Several PSG parameters such as AHI, RDI and ODI showed no statistically significant change before and after END application (p>0.05) (Fig. 5).
However, after END use, the proportion of patients that slept in a supine position increased from 38.0 to 44.5% (Fig. 6). There was no significant change in sleep time or loudness of snoring before and after END use.
DISCUSSION
The present study revealed a significant increase in acoustic parameters such as TNV and MCA after END use. This result is in accordance with that of previous studies in Caucasian patients. Although EXD and END both have been reported to significantly increase the dimensions of the nasal cavity, END has been shown to be much more effective for reducing nasal resistance.13)14) Latte and Taverner suggested that EXD induced a significant increase in MCA.15) The beneficial effect of increasing the MCA and reducing nasal resistance is especially notable in patients with septal deviation.16) Metes et al. suggested that the nasal resistance in 72 individuals was significantly decreased from 0.164±0.128 to 0.065±0.037 Pa/cm3/sec after END use.17)
We also observed that PNIF, an objective parameter for the evaluation of nasal airflow, significantly increased after END use. In their recent study with adolescents, Dinardi et al. suggested that PNIF significantly increased from 116.±38 to 123±38 L/minute after EXD use.18) END has also been reported to increase PNIF significantly in adolescent athletes.19) When Barnes and Lipworth compared two different types of END, Sinuscone® and Nozovent®, they found that only the former caused a significant increase in PNIF.20) Comparing EXD and END, Raudenbush suggested that END was superior to EXD for dilating the nasal cavity and improving nasal airflow.21) END proved to also be excellent in increasing the volume/dimensions of the nasal cavity and improving nasal airflow in Asian patients.
Given our hypothesis that improvement in nasal breathing may have a beneficial effect on OSA, patients were given the ESS questionnaire before and after END use. Seven of 11 patients (63.6%) reported subjective improvement in their daytime sleepiness. However, as the overall decrease in ESS score after END was not statistically significant, it is unreasonable to interpret that daytime sleepiness improved significantly after END use in our study. Shinkawa and Sakai reported that 13 of 18 patients (72.2%) exhibited an improvement in snoring after END use.22) Scharf et al. suggested that 25.6% of patients reported improvement in ease of breathing, 34% in snoring loudness and 21.8% in quality of sleep with END use.23) After 10 days of END use, patients and their bedtime partners reported improved snoring and mouth dryness.24) On the other hand, EXD also caused significant improvement in snoring (evaluated by the patient's partner), dry mouth and daytime sleepiness (ESS score).8)
Our patients were classified into two subgroups, the responder and non-responder groups, according to their improvement in daytime sleepiness. Upon comparing several demographic variables such as sex, age, BMI, and Friedmann staging between groups, the responders were significantly younger than those in the non-responder group. There were no significant differences in the other variables. More research is needed to determine why this phenomenon occurs for some reason.
In this study, there was no improvement in PSG parameters, such as AHI, RDI and ODI. Djupesland et al. suggested that after EXD use, AHI was significantly increased in patients with larger nocturnal nasal dimensions.13) In patients with chronic rhinitis, EXD also failed to improve sleep parameters such as sleep quality, AHI and snoring loudness.25) However, END has been shown to have some beneficial effect on lowering the required CPAP pressure in patients who previously required more than 9 cmH2O of pressure.26) However, END had no effect on AHI, RDI, and oxygen saturation in patients with OSA.17)27)28) Therefore, these results observed in Caucasian patients may also be true in Asian populations.
Although END had no effect on the PSG parameters in our study, we found that the proportion of patients sleeping in the supine position increased with END use. We could hypothesize that as patients experienced sleep quality improvement due to improved nasal airway flow, they did not require sleep position changes. In fact, 10 of 11 patients reported a willingness to use the END after the end of this study due to patient satisfaction. To see whether this change in sleep position is really due to improved sleep quality, we could perform a repeated evaluation on a larger number of subjects. In addition, patients may be asked to perform sleep quality questionnaires such as ‘Pittsburgh Sleep Quality Index’ to see whether changes in sleep position are actually related to changes in sleep quality.
The main pitfalls of our study were a small study population and relatively short study period (2 weeks). Löth and Petruson reported that the 6-month compliance for nasal dilators was about 60%.29) When they performed long-term follow-up up to 5 years, compliance fell to 21% (only 9 of 42 initial patients continued to use the nasal dilator).30) Among these 9 patients with continued use, seven patients underwent additional surgical procedures such as an uvulopalatopharyngoplasty.30) Therefore, for long-term OSA control, it would be preferable to combine END with other treatment modalities.
A future study focusing on athletes could yield useful information. Although we first planned to conduct this study with athletes, they were reluctant due to a fear of spurring a doping controversy (regarding non-physiological methods of improving their athletic performance). In a study of 48 adolescents, Dinardi et al. suggested that they showed improved cardio-respiratory capacity and less dyspnea after a 1,000-m race.18) However, it is not likely that this could be related to an improvement in athletic performance. Adams and Peiffer suggested that EXD and END failed to improve the performance of 20-km cyclists.31) Furthermore, there was no significant change or improvement in athlete heart rate, oxygen saturation index, and maximal oxygen uptake.19) Therefore, END may be an effective non-pharmacological device that could improve athletes' discomfort and dyspnea without affecting their actual performance.
We can easily find patients who complain that the quality of sleep is impaired by nasal obstruction in the outpatient setting. Therefore, we can obtain more meaningful results by confirming the improvement of subjective symptom score (NOSE scale, for example), in addition to the objective improvement of nasal airflow after the use of END. In addition, as we have used portable PSG instead of full PSG, there might be limitations in the accuracy of the main index related to sleep apnea such as AHI, RDI and ODI.
In Korean adults, the average distance from the nostril to the internal nasal valve is about 1.8 cm.32) The END used in this study is inserted up to a depth of 1.2 to 1.5 cm from nostril. Although END does not directly dilate the internal nasal valve, it may be helpful to dilate the internal nasal valve due to the elasticity of the END. Indeed, the acoustic rhinometry of individual patients showed that the cross-sectional area of the internal nasal valve position increased after the END wear.
One of the pitfall in our study is that a placebo effect could not be ruled out without use of sham device. Also, one could argue that increase in a supine sleep position by use of END could be day-to-day variations. To prove that improved nasal flow by END resulted in more supine position during sleep, further repetitive testing with more subjects is needed.




 PDF
PDF ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download