Abstract
Appropriate prescription writing is one of the critical medical processes affecting the quality of public health care. However, this is a complex task for newly qualified intern doctors because of its complex characteristics requiring sufficient knowledge of medications and principles of clinical pharmacology, skills of diagnosis and communication, and critical judgment. This study aims to gather data on the current status of undergraduate prescribing education in South Korea. Two surveys were administered in this study: survey A to 26 medical schools in South Korea to gather information on the status of undergraduate education in clinical pharmacology; and survey B to 244 intern doctors in large hospitals to gather their opinions regarding prescribing education and ability. In survey A, half of the responding institutions provided prescribing education via various formats of classes over two curriculums including lecture, applied practice, group discussions, computer-utilized training, and workshops. In survey B, we found that intern doctors have the least confidence when prescribing drugs for special patient populations, especially pregnant women. These intern doctors believed that a case-based practical training or group discussion class would be an effective approach to supplement their prescribing education concurrently or after the clerkship in medical schools or right before starting intern training with a core drug list. The results of the present study may help instructors in charge of prescribing education when communicating and cooperating with each other to improve undergraduate prescribing education and the quality of national medical care.
Medical educational institutions in Korea have been focusing on the vocational education aspects of physician training by emphasizing broad clinical knowledge and skills that can be directly utilized in the daily medical practice, in addition to imparting in-depth knowledge. Due to recent developments in medical research and advances in the information service industry, a large amount of medical knowledge regarding both new and old drugs is produced and shared in real time with few filters. However, there is a limit to the traditional apprenticeship education system when considering these changes to the available medical knowledge. If a doctor fails to acquire the principles of personalized pharmacotherapy in selecting proper drugs and determining their regimens based on medical and clinical pharmacological evidence, it might be difficult for him/her to make a decision regarding the optimal drug therapy based on the latest medical information.
Prescribing appropriate medication is an important factor in determining the quality of public health care. This is a complex task that demands adequate knowledge of the medications and principles of clinical pharmacology, skills in diagnosis and communication, and critical judgment.[1] Some previous studies report that inadequate training is often a contributory factor to prescribing error-related adverse medication events.[234] However, most medical education institutions in Korea focus on education of the pathogenesis and diagnosis of diseases, and education on the treatment of diseases including drug prescriptions has traditionally only occurred in the form of memorization education. Even in the senior grade classes for clinical practice, medical students receive insufficient and fragmentary guidance on drug prescribing principles based on clinical pharmacological knowledge such as drug interaction and pharmacokinetic characteristics in special patients. This, in turn, negatively affects their drug prescribing proficiency and the quality of national medical care by practitioners (including interns and residents) who play a significant role in the care delivered at large hospitals.
Clinical pharmacology is an academic discipline that deals with dose responses and side effects of a drug beyond its basic pharmacological mechanism. This approach can be used to understand drug labels and facilitate prescription in clinical practice.[56] Therefore, we hypothesized that the status of undergraduate education for clinical pharmacology might influence the prescribing ability of newly qualified intern doctors (those who obtained the M.D. license right before entering the internship), and investigated the status of undergraduate education in clinical pharmacology and the prescribing ability of intern doctors in South Korea.
The study consisted of 2 surveys. Survey A was administered to 26 of a total of 41 medical schools in South Korea to gather information on the status of undergraduate education of clinical pharmacology. Survey B was given to 244 intern doctors who work in large domestic hospitals to obtain their subjective opinions related to prescribing education and ability.
Survey A was sent to professors in pharmacology and clinical pharmacology departments of 41 medical schools in South Korea in 2015 to investigate the current status of undergraduate prescribing education. The contents of the questionnaire included i) the timing and type of prescribing education during undergraduate education, ii) the number and composition of the faculty in charge of the curriculum, iii) the educational topics covered in prescribing education programs, and iv) the educational and evaluation methods. The questionnaires were designed as multiple choice questions and were developed by referring to previous studies.[78]
Intern doctors voluntarily responded to survey B, administered online or in paper, from May 2015 to February 2016. The contents of this questionnaire included i) undergraduate education for clinical pharmacology and drug prescribing (single choice), ii) experiences of drug prescribing in the intern period (multiple choice), iii) information sources for drug prescribing (single choice), and iv) subjective opinions about drug prescribing education (open questions). The questionnaires were developed by referring to previous studies.[2910]
Twenty-six of 41 medical schools answered the question regarding the types and timing of their curricula for drug prescribing. Thirteen of 26 institutions (50.0%) provided drug prescribing education in one curriculum, whereas the other half organized their drug prescribing education in 2–4 curricula. Table 1 summarizes the types of curricula in the 26 institutions. Basic pharmacology courses were the most common curriculum that provided drug prescribing education in 17 institutions (65.4%). Ten institutions (38.5%) arranged their drug prescribing education in a clinical pharmacology course, and nine institutions prepared their drug prescribing education in block lecture courses. In 10 institutions, several hours were assigned for drug prescribing education during clinical curricula including lectures, practical exercises, or elective practice courses in senior grades.
A total of 85 instructors (median 2.5 persons) supervised drug prescribing education in 26 institutions. Among them, 75 were faculty members of the institutions; 10 were invited faculty. These instructors included 39 pharmacologists, 37 clinical pharmacologists, 7 clinicians, and 2 clinical pharmacists.
The most common educational theme was pharmacokinetics, while pharmacodynamics, the drug development process, drug interactions, pharmacogenetics, adverse drug reactions, therapeutic drug monitoring, and drug therapy in patients with renal/hepatic impairment were also common themes that was covered in more than half of the institutions. The educational themes of the drug prescribing curricula are summarized in Table 2.
The lecture was an essential class format for drug prescribing education that was adopted in all 26 institutions. Besides lecture classes, various other formats were additionally adopted in 11 institutions, such as small-group discussions (7 institutions), computer-utilized training (5 institutions), practical training in the clinical field (5 institutions), self-study with provided materials (5 institutions), problem-based learning (4 institutions), and workshops (2 institutions).
Written examination was the most commonly used tool for learning assessment in the drug prescribing education programs in 25 of 26 institutions. Learning achievement was also assessed with students' attitudes during the class (13 institutions), portfolio works (eight institutions), overall evaluation of discussions, workshops, practice, etc. (six institutions), and formative evaluation of discussions, workshops, practice, etc. (two institutions). One institution which did not apply written examination assessed learning achievement with students' attitudes during the class, portfolio works, and overall/formative evaluation.
All 244 intern doctors responded to the questionnaire for survey B. Among them, 215 intern doctors (88.1%) answered that they had learned clinical pharmacology. Most of them assessed their knowledge levels of clinical pharmacology as poor or intermediate: 2 persons (0.8%) responded at a good level, 86 persons (35.4%) at an intermediate level, and 155 persons (63.8%) at a poor level; one person did not answer (0.4%). A majority of the intern doctors felt that their undergraduate education was insufficient for safe- (75.8%) and evidence-based (68.9%) drug prescription.
Over half of the intern doctors (57.4%) reported that they had experienced some problems in drug prescribing. They reported having frequent problems when prescribing drugs for special populations such as renal/hepatic impairment, pediatric or elderly patients, or pregnant women. Drug interaction was also a common problem category in drug prescription among intern doctors. The categories of those problems are summarized in Table 3.
A majority of the intern doctors answered that, without supervision by senior doctors, they could prescribe antihistamines (58.2%), vitamins or minerals (50.8%), and antacids (49.6%), while none of them could prescribe thrombolytics or anti-Parkinson drugs (Table 4).
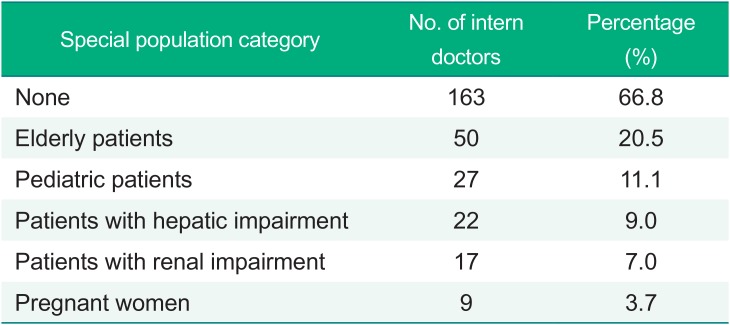
Over half of the intern doctors (66.8%) answered that they could not prescribe drugs for any special patient population mentioned above without the supervision of senior doctors. The elderly patient population (20.5%) was a relatively easier special patient population for the intern doctors to prescribe without the supervision of senior doctors. Table 5 presents those special patient populations for whom the intern doctors could prescribe drugs without the supervision of senior doctors.
The intern doctors thought that safety (79.1%) was the most important factor in prescribing drugs. Few answered that they found efficacy (16.5%) or cost-effectiveness (2.9%) as the most important factor in prescribing drugs.
When intern doctors prescribed any drug for the first time, more than half of them always (35.2%) or often (31.5%) confirmed the drug information. They obtain the drug information from internal documents (50.0%), internet sites (30.7%), consultation with colleague doctors (17.6%), and articles/books (0.8%). They usually searched these sources to check recommended regimens/dosages (24.6%), contraindications (15.2%), indications (12.9%), adverse drug reactions (9.6%), while none of them reported checking information on drug interactions (0.0%).
The intern doctors provided subjective opinions to improve drug prescribing education with a more pragmatic view. They thought that some educational themes should be strengthened such as effective methods to search for information related to drug prescription, practical prescription training on commonly prescribed drugs in the real world, dose calculation training for special patient populations, and common drug interactions. They proposed case study, group discussions, and practical training in a ward as the recommended class formats either in the senior grade of medical school or right before starting internship.
This is the second report on the status of undergraduate education of clinical pharmacology and the first report on the prescribing ability of intern doctors in South Korea. The present study conducted two surveys focused on drug prescribing education for intern doctors as well as faculty members in medical schools, while a previous report by Lim et al. in 2002 had conducted a survey focused on clinical pharmacology education for faculty members only. According to a previous report by Lim et al. in 2002,[8] 10 of 36 medical educational institutions (27.8%) in South Korea had independently taught courses on clinical pharmacology in their undergraduate curriculum. The present survey shows that 10 of 26 institutions (38.4%) had independently provided a course on clinical pharmacology in 2015. The number of institutions having independent clinical pharmacology curriculum has not changed, and its percentage has increased since 2002 due to lower response rate of the present study.
Half of the institutions covered drug prescribing education with various types of curricula over two years. Basic pharmacology and block lectures were covered in the junior grade, while clinical pharmacology, clinical curriculums were taught in the senior grades. As the formats of the classes and learning achievement assessments were diversified by the institutions, sharing the strengths and weaknesses of these formats among the institutions might be helpful to upgrade the quality of drug prescribing education.
Among the respondents, 88% answered that they have learned clinical pharmacology. This far exceeds the percentage of institutions that independently provided a course on clinical pharmacology. There might be selection bias that intern doctors working at large hospitals in metropolitan areas responded more frequently. Only 0.8% of the intern doctors judged their knowledge levels of clinical pharmacology as good, a much lower percentage (8%) than the British doctors from the previous report by McLay et al.[10] However, this result does not directly mean that the knowledge levels of clinical pharmacology of Korean intern doctors were poorer than those of British, because this difference seems to be related to the number of levels of questionnaire. The question of McLay's study had five levels of choice items (very poor, poor, average, good, and excellent), while the question of the present study had three levels of choice items (poor, average, good).
Prescribing drugs in special patient populations was the most difficult problem for the intern doctors in the present survey. Similar to the British doctors,[10] the intern doctors felt most uncomfortable when prescribing drugs to the special population of pregnant women without the supervision of senior doctors (Table 5). The intern doctors in this survey and the British doctors in McLay's survey reported the lowest confidence, in common, in prescribing anti-Parkinson drugs and thrombolytics.[10] However, only 0.8% of Korean intern doctors in this survey reported to have confidence when prescribing digoxin, while 36% of British doctors had confidence in prescribing this drug. The intern doctors gave their opinion that prescribing education should be conducted in a case-based practical training or group discussion class concurrently or after the clerkship in the senior grade of medical schools or right before starting internship training with some core prescription drugs. In addition, they thought that education on effective ways to search for information related to drug prescription is necessary for undergraduate curricula. Their opinions for the improvement of drug prescribing education had a lot in common with the recommendations of Ross et al.[11]
The present study has some limitations because of the small number of non-randomized responders. Therefore, the responders in the present study did not represent all medical educational institutions and intern doctors in South Korea. Nevertheless, the results of this study provide valuable data that will help to improve the quality of national medical care. In particular, care could be improved if the instructors who supervise the prescribing education programs in institutions would actively communicate their experiences and ideas with each other through regular domestic meetings. In the United Kingdom, Baker et al. suggested developing a core drug list in the interest of improving prescribing education and reducing errors, and Maxwell et al. proposed a dynamic interactive electronic drug formulary for medical students.[1213] We propose a domestic medical educator meeting or forum to develop a core drug list, drug formulary, or other educational materials that fit the clinical circumstances of South Korea. In the meeting, faculty members should share their various experiences of prescribing education and openly discuss their ideas for the effective education program including proper themes, timing, class format, and qualification of faculty members, etc. These continuous efforts for the close communication might be helpful for upgrading undergraduate drug prescribing education.
References
1. Maxwell SR. An agenda for UK clinical pharmacology: How should teaching of undergraduates in clinical pharmacology and therapeutics be delivered and assessed? Br J Clin Pharmacol. 2012; 73:893–899. DOI: 10.1111/j.1365-2125.2012.04232.x. PMID: 22360965.

2. Heaton A, Webb DJ, Maxwell SR. Undergraduate preparation for prescribing: the views of 2413 UK medical students and recent graduates. Br J Clin Pharmacol. 2008; 66:128–134. DOI: 10.1111/j.1365-2125.2008.03197.x. PMID: 18492128.

3. Denison Davies E, Schneider F, Childs S, Hucker T, Krikos D, Peh J, et al. A prevalence study of errors in opioid prescribing in a large teaching hospital. Int J Clin Pract. 2011; 65:923–929. DOI: 10.1111/j.1742-1241.2011.02705.x. PMID: 21752165.

4. Franklin BD, Reynolds M, Shebl NA, Burnett S, Jacklin A. Prescribing errors in hospital inpatients: a three-centre study of their prevalence, types and causes. Postgrad Med J. 2011; 87:739–745. DOI: 10.1136/pgmj.2011.117879. PMID: 21757461.

5. Gray J. The state of clinical pharmacology today. Clin Pharmacol Ther. 2013; 93:231–232. DOI: 10.1038/clpt.2012.231. PMID: 23419488.

6. Gray JD, Danoff D, Shepherd AM. Clinical pharmacology education: looking into the future. Clin Pharmacol Ther. 2007; 81:305–308. PMID: 17259956.

7. O'Shaughnessy L, Haq I, Maxwell S, Llewelyn M. Teaching of clinical pharmacology and therapeutics in UK medical schools: current status in 2009. Br J Clin Pharmacol. 2010; 70:143–148. DOI: 10.1111/j.1365-2125.2010.03665.x. PMID: 20642558.
8. Lim YC, Shon JH, Yoon YR, Shin JG, Roh HK, Sohn DR, Shin SG, et al. A survey on the current status of clinical pharmacology education in Korean medical schools. Transl Clin Pharmacol. 2002; 10:24–33.

9. Oshikoya KA, Senbanjo IO, Amole OO. Interns' knowledge of clinical pharmacology and therapeutics after undergraduate and on-going internship training in Nigeria: a pilot study. BMC Med Educ. 2009; 9:50. DOI: 10.1186/1472-6920-9-50. PMID: 19638199.

10. Tobaiqy M, McLay J, Ross S. Foundation year 1 doctors and clinical pharmacology and therapeutics teaching. A retrospective view in light of experience. Br J Clin Pharmacol. 2007; 64:363–372. PMID: 17506779.

11. Ross S, Maxwell S. Prescribing and the core curriculum for tomorrow's doctors: BPS curriculum in clinical pharmacology and prescribing for medical students. Br J Clin Pharmacol. 2012; 74:644–661. DOI: 10.1111/j.1365-2125.2012.04186.x. PMID: 22288524.

12. Baker E, Roberts AP, Wilde K, Walton H, Suri S, Rull G, et al. Development of a core drug list towards improving prescribing education and reducing errors in the UK. Br J Clin Pharmacol. 2011; 71:190–198. DOI: 10.1111/j.1365-2125.2010.03823.x. PMID: 21219399.

13. Maxwell SR, McQueen DS, Ellaway R. eDrug: a dynamic interactive electronic drug formulary for medical students. Br J Clin Pharmacol. 2006; 62:673–681. PMID: 17054667.

Table 1
Types of curricula that contain drug prescribing education in each institution (Survey A)
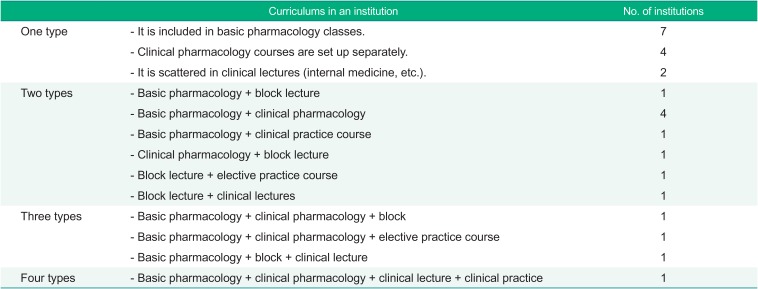
Table 2
Educational themes of the curricula for drug prescribing (Survey A)
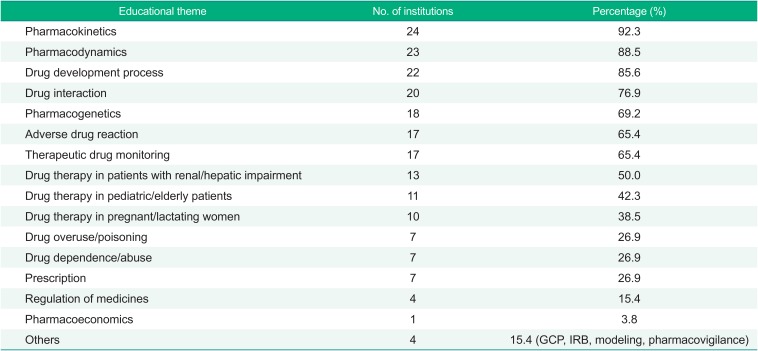
Table 3
Summary of drug prescription-related problems of intern doctors (Survey B)
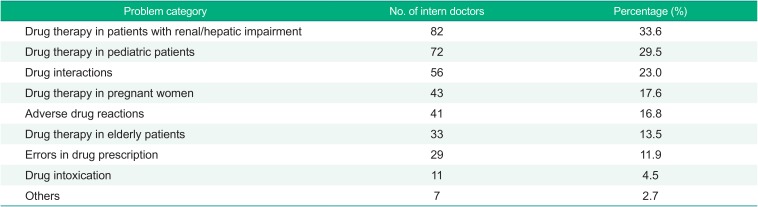
Table 4
Medications that intern doctors could prescribe without the supervision of senior doctors (Survey B)
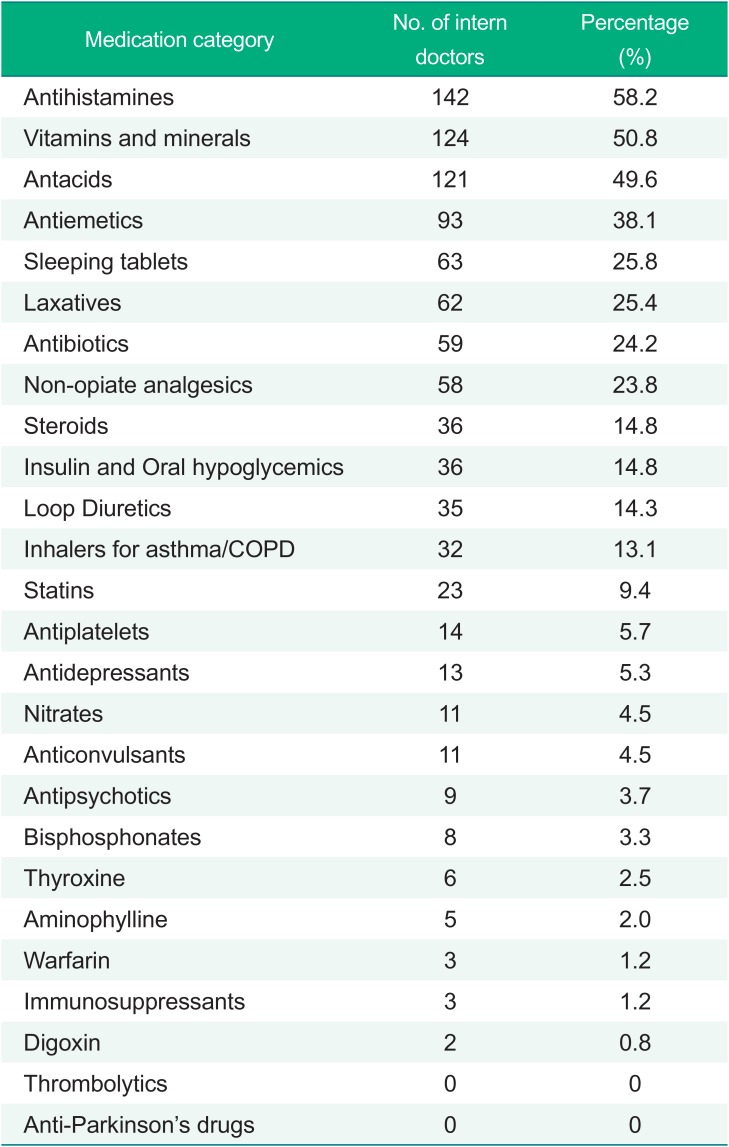
Table 5
Special populations that intern doctors could comfortably prescribe drugs without the supervision of senior doctors (Survey B)




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download