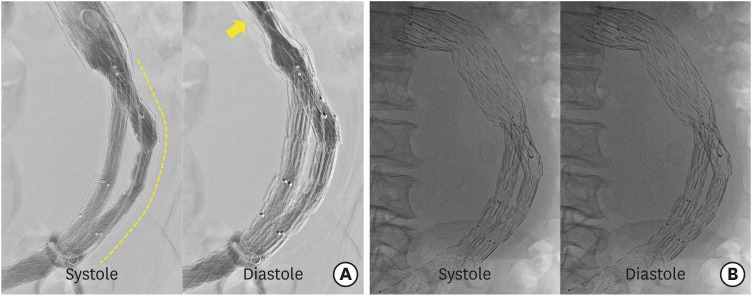
An 80-year-old male patient presented with abdominal pain. Nine years ago, he underwent endovascular repair for an abdominal aortic aneurysm. Since then, re-interventions for endoleaks had been performed thrice (Figure 1A and B). Five years ago, he presented with syncope and computed tomography (CT) aortography showed a retroperitoneal hematoma and increased size of aneurysmal sac with a type Ib endoleak. Both iliac limbs were then extended using SEAL stent grafts (S&G Biotech Inc., Seongnam, Korea). Three years ago, a type Ib endoleak has recurred from the right iliac limb and an Endurant iliac extension stent graft (Medtronic Vascular, Santa Rosa, CA, USA) was implanted into the right external iliac artery. Two years ago, he presented with abdominal pain. The CT angiography findings revealed that an aneurysmal sac increased in size and the left contralateral limb of stent graft was disconnected from the bifurcated main body, resulting in a type IIIa endoleak. An AFX stent graft (Endologix, Inc., Irvine, CA, USA) was additionally placed at the disconnected left limb. At this time, the CT showed that an aneurysm increased with a diameter of 12×16 cm and a contrast leakage was observed in front of the left limb of stent-graft, suggesting type Ib or type III endoleak (Figure 1C). The fluoroscopy showed a pulsatile compression of the stent-graft, which could imply that the intra-aneurysmal pressure might be above the diastolic blood pressure (Figure 2, Supplementary Video 1). The overlapping stent-graft which was previously implanted was distally displaced, causing type III endoleak. The patient refused surgery. We placed grafts at the site of a modular dehiscence, but the pulsatile compression of stent-graft was continuously observed (Figure 3A, Supplementary Video 2). After 7 days, the pulsatile compression of the stent-graft disappeared (Figure 3B, Supplementary Video 3). The intra-aneurysmal pressure might have gradually decreased with the improvement of the endoleak.
Our case demonstrated that type III endoleaks repeatedly increased the intra-aneurysmal pressure, leading to the pulsatile compression of the stent-graft. This may indicate an extremely high risk of aortic rupture. This case also showed that the larger the aneurysm, the higher the intra-aneurysmal pressure and risk of subsequent rupture. Finally, fluoroscopy may be helpful to identify the alignment of stent-graft and investigate the type of endoleak.
The patient’s informed consent has been waived by Institutional Review Board (IRB) approval (Gachon Medical Center IRB, GAIRB2022-083).
Notes
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Data Sharing Statement: The data generated in this study is available from the corresponding author upon reasonable request.
Author Contributions:
Conceptualization: Kang WC.
Data curation: Oh PC, Jang AY.
Formal analysis: Jang AY.
Investigation: Kang WC.
Methodology: Kang WC.
Project administration: Kang WC.
Software: Jang AY.
Supervision: Kang WC.
Validation: Jang AY.
Visualization: Oh PC.
Writing - original draft: Oh PC.
Writing - review & editing: Kang WC.
Figure 1
The CT images. (A and B) The CT angiography (performed 2 months ago) showed no endoleak and no interval change of the aneurysmal sac size (10×16 cm). (C) In this presentation, an increase in aneurysmal sac size (12×16 cm) and contrast leakage (arrow) in front of the left limb of the stent-graft were observed.
CT = computed tomography.
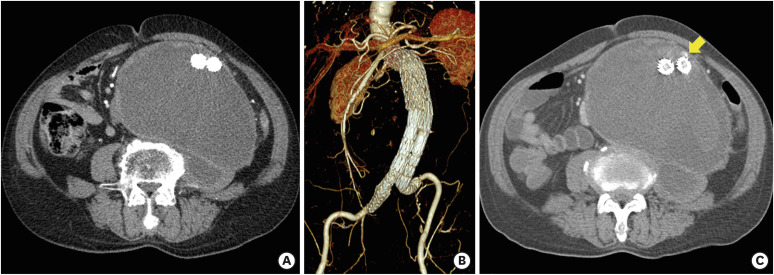
Figure 2
The fluoroscopic and aortographic images. (A) The fluoroscopy showed a diastolic compression of the main body of stent-graft. (B) The aortography showed that the left limb extension (implanted 2 years ago) for type IIIa endoleak was focally bulged at the systolic phase (arrow), which was considered an active-seal phenomenon of the AFX device (Endologix, Inc., Irvine, CA, USA). Another focal bulging at the connection part of the modular components was also observed (arrowhead), indicating a suspicious type IIIa endoleak.
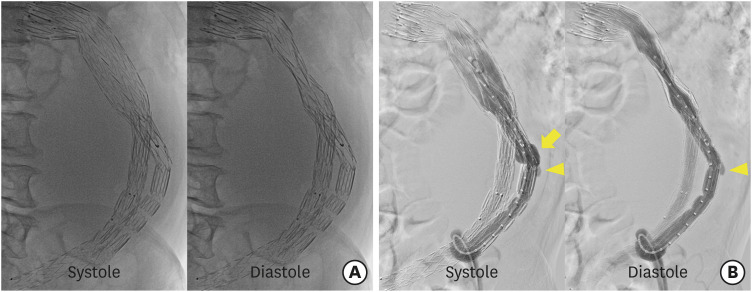
Figure 3
The completion aortographic and fluoroscopic images. (A) The completion aortography showed that the focal bulging of left limb disappeared after the additional placement of a stent-graft (dashed line), but the pulsatile compression of the main body persisted (arrow). (B) After 7 days, the fluoroscopy revealed that the pulsatile compression of the stent-graft completely disappeared.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download