This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Remifentanil infusion is commonly used for general anesthesia but reflex cough can occur after an intravenous (IV) infusion. This study was designed to examine the effect of IV-dexamethasone on remifentanil-induced cough (RIC).
Methods
One hundred thirty patients scheduled for elective surgery were randomly assigned into two groups that received by either 2 ml of IV 0.9% saline (Group C, n = 68) or 10 mg of dexamethasone (Group D, n = 62) 5 min before administration of remifentanil at a target effect-site concentration of 5 ng/ml. The incidence and severity of coughs of each patient were recorded.
Results
The overall incidence of cough was 6.5% (4/62 patients) in Group D and 26.5% (18/68 patients) in the Group C (P = 0.002). The severity of cough observed was significantly different by dexamethasone pretreatment (P = 0.02) but there were no significant hemodynamic changes.
Conclusions
Pretreatment with dexamethasone after IV administration was effective in suppressing the reflex cough induced by remifentanil infusion.
Keywords: Cough, Dexamethasone, Remifentanil
Introduction
Remifentanil is a fentanlyl derivative and a µ-opioid receptor agonist with a very short reaction time. It has been shown that during induction of general anesthesia, and tracheal intubation, opioids suppress the cough reflex. Similar to fentanyl, the injection of remifentanil induces cough (i.e. remifentanil-induced cough, RIC), and the incidence has been reported to be approximately 27-28% [
1,
2].
Cough induced during the induction of general anesthesia sometimes, elevates cerebral, ocular or abdominal pressure, and thus it may become threatening to the patients. Tweed and Dakin [
3]. have reported the cases requiring immediate tracheal intubation for excessive coughs prior to the induction of general anesthesia.
Until now, efforts have been made to reduce the cough reflex induced by opioids agonists, -and it has been reported that the selective β-2 agonist turbutaline or salbutamol, lidocaine, and ketamine were effective on reducing fentanyl-induced cough (FIC) or RIC [
1,
2,
4-
6]. In addition, Lim et al. [
7] have reported that a split-dose intravenous injection of - remifentanil reduced the incidence of cough, and Lin et al. [
8] have reported that the pretreatment with dexamethasone reduced FIC effectively.
There are no studies on the incidence or severity of RIC in cases when patients are pretreated with the intravenous injection of dexamethasone.
Therefore, in our study, the incidence and severity of RIC was examined when patients were pretreated with 10 mg of dexamethasone, IV prior to the injection of remifentanil.
Materials and Methods
This study was approved by the Institutional Review Board. The purpose and methods of the study were explained sufficiently to patients and their guardians and then, consent was obtained for the study.
The study was conducted on 140 patients between the age of 18 years and 70 years with an Anesthesiologists Physical Status I and II.
Patients with a past history of smoking, chronic obstructive lung diseases, asthma or upper respiratory infection, a history of angiotensin converting enzyme inhibitor, bronchodilators, or steroid uses, or the history of allergy to drugs were excluded from our study. The patients fasted for 8 hours prior to surgery. A 20 G cannula was installed on the dorsum manus prior to the arrival in the operation rooms, and a T-connector was connected for drug injection. Midazolam (2 mg) and glycopyrrolate (0.2 mg) were injected intramuscularly 30 minutes prior to the induction of anesthesia.
For all patients arriving in the operating room, an electrocardiomyogram, non-invasive blood pressure, and pulse oximetery were performde and the vital signs of patients were measured. A total of 140 patients were considered, but 10 patients dropped out and, 130 patients were then randomly assigned to either the control group (Group C) or the dexamethasone group (Group D). Five minutes prior to the injection of remifentanil, 10 mg of dexamethasone (in 2 ml total volume) was injected into patients in D group, and the same volume of 0.9% saline was injected into patients in group C.
Remifentanil was injected until the concentration reached the target concentration of 5 ng/ml using a Target- controlled infusion device (TCI) [Orchestra® with Base Primea, Fresenius-Kabi, France]). Another anesthesiologist who does not know the type of drugs injected recorded whether or not cough developed as well as the frequency of cough from the time of the injection of remifentanil to 2 minutes after reaching the target concentration 5 ng/ml. Blood pressure of patient, pulse, and oxygen saturation levels were recorded immediately after arrival at operation room (T0), immediately after remifentanil reached the target concentration (T1), and after the injection of propofol (T2). The interval between T0 and T1 varied depending on the preparation process and the time to reach the target concentration for each patient: this time, was approximately 5-10 minutes, and thus T2 was measured 5 minutes after the measurement of T1.
The severity of cough was graded depending on the frequency of cough, and was recorded as mild (1-2 times), moderate (3-4 times), or severe (more than 5 times). A preliminary study was performed on 30 patients, and it was found that the cough reflex developed from the infusion of remifentanil to within 2 minutes after reaching the target concentration 5 ng/ml). Based on this, 2 minutes after reaching the target concentration was determined as the time for the injection of propofol.
During the injection of remifentanil, if oxygen saturation level decreased to lower than 90%, mask ventilation support using 100% oxygen was initiated immediately, and the development of apnea, stiffness of chest muscles, or neuropsychological symptoms were recorded. Apnea was defined as the respiration arrest period of longer than 20 seconds. Neuropsychological symptoms were defined as a the feeling of the dissociation phenomenon (i.e. as if the body is floating), impairment of alertness including drowsiness, changes of tastes, and changes of sensation such as numbness, hot, cold, etc.
In preliminary studies, the incidence of cough in the dexamethasone group was reduced by approximately 20% when compared to the saline injected control group. Using these data,, the number of samples to obtain 80% statistical power at the 95% significance level was calculated as minimal 59 patients per group. Considering a drop out rate of approximately 10%, studies were attemped to be performed with a total sample number of 140 patients. For statistical analysis, SPSS 13.0 (SPSS Inc, Chicago, IL, USA) was used. All results were presented as a mean ± standard deviation. Comparison of age, height, weight, total amount of remifentanil, and hemodynamic measurements were analyzed by t-test. The comparison of the gender of the two groups, ASA class, with or without development of cough, and the severity of cough were analyzed by chi-square test. In all cases, a P value less than 0.05 was considered statistically significant.
Results
Out of 140 patients; that entered the study, 10 patients; had blockage of the intravenous line and thus were excluded from the study. Hence, a total 130 patients were enrolled as study patients and 68 patients wererandomized in group C and , and the 62 patients were randomized into group D. In any patient during the injection of remifenils, there was never a development of the stiffness of chest muscles or neuropsychological symptoms and oxygen saturation level during the injection never decreased below 90%.
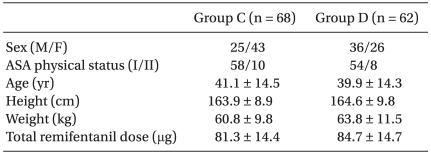
When comparing demographic data of the patients in both groups, age, gender, height, weight and ASA class were not different. Similarly, the total injection volume of remifentanil to reach the target concentration of 5 ng/ml in the two groups was not different (
Table 1).
The vital signs assessed at the three designated time points (T0; immediately after arriving at operation room, T1; immediately after reaching the target concentration of remifentanil, T2; after the injection of propofol) of the two groups were also not different.
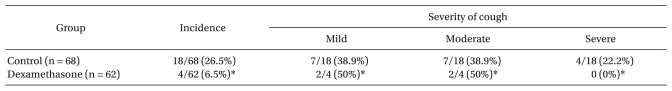
The development of cough observed from the time of the injection of remifentanil in Group C occurred in 18 patients (26.5%). Among them, 7 patients (38.9%) were classified as mild (1-2 times), 7 patients (38.9%) were moderate (3-4 times), and 4 patients (22.2%) were severe (more than 5 times). In Group D, cough developed in 4 patients (6.5%). Among them, 2 patients (50%) were mild, 2 patients (50%) were moderate, severe cough was not observed. When compared to Group C, the incidence of cough in Group D was significantly lower, and similarly, the severity of cough was also significantly different (p < 0.05,
Table 2).
Discussion
In our study, IV pretreatment with 10 mg of dexamethasone prior to the injection of the targetconcentration of remifentanil; 5 ng/ml; reduced the incidence of RIC from 26.5% to 6.5% (P < 0.05). In addition, in the group pretreated with 10 mg of dexamethasone, only mild or moderate levels of cough were noted, thereby significantly reducing the severity of cough when compared to Group C (p < 0.05).
In comparison with fentanyl, the starting time for remifentanil after induction of general anesthesia is fast and regardless of the injection time of each -opioid agonists, their half-lives are short (approximately 3-5 minutes), and they rapidly reach steady state. If remifentanil is injected continuously in the induction of general anesthesia, reduced doses of propofol may be used.
This could prevent the rapid decrease of blood pressure induced by propofol, avoid the rapid increase in blood pressure after response to stress such as tracheal intubation, therefore vital signs of patients could be more stable while induicing of general anehsthesia [
9].
It has been shown that cough develops in response to the administration of opioids, but the exact mechanisms have not been elucidated. However, opioid agents block the central sympathetic nervous system, activate the parasympathetic nervous system, and thus induce cough and the reflex contraction of the bronchus.
Reports that the administration of bronchodilators suppressed FIC support this possibility [
4,
5]. In addition, as another possible mechanism, the chemical reflex of the respiratory system mediated by fast acting irritant receptors located adjacent to the blood vessels in the respiratory system or vagal C-fibers receptors is also possible explanation [
9]. Futher, it has been also reported that opioids contract tracheal smooth muscles resulting in the irritation of the stimulatory receptor in the mucosa of the upper respiratory tract [
10,
11].
Kim et al. [
1] have reported that to prevent RIC, a target remifentanil concentration of 4 ng/ml must be injected using a target infusion concentration device. When 0.5 mg/kg of lidocaine was injected prior to the injection, the incidence of cough was reduced from 27.6% to 15.2%. Kim et al. [
2] have reported that when a target concentration of remifentanil was 5 ng/ml, a prior injection of, 0.1 mg/kg of ketamine resulted in reduction in the development of cough from 27.9% to 11.5%.
In addition, Lim et al. [
7] -have reported when a split -dose remifentanil was injected, the development of cough was reduced from 34% to 12%. Similarly, in our study, when remifentanil was injected in the control group, the development of cough was 26.5%, with comparable in incidence to the previous reports. In the group pretreated with 10 mg of dexamethasone, the development of cough was greatly reduced to 6.5%, and the severity of cough was also significantly lowered.
Dexamethasone has been used as a mast cell stabilizer. Murlas et al. [
12] have reported that in guinea pigs, dexamethasone improves bronchoconstriction mediated by tachykinin.
Tachykinin is released after the activation of C-fibers in the airway and directly induces the contraction of smooth muscle in the airway [
13]. Indirectly, it induces the release of histamine from mast cell in the airway and thus facilitates the excitation of receptors where histamine rapidly acts [
14].
In addition, it has been reported that dexamethasone enhances the activation of neutral endopeptidase which reverses the enhanced airway reactivity of airway epithelial cells [
15,
16]. Further, corticosteroids have been reported to increase beta adrenergic receptors on lung cells [
17].
It has been reported that dexamethasone injected once prior to surgery cough could prevent nausea and vomiting that may be developed after surgery [
18], was effective on the amelioration of pain after surgery [
19] and could reduce cough, which was the aim of this study. In addition, it has been reported that steroids reduce postoperative edema in numerous types of surgery. For example, Weber and Griffin [
20] have reported that in patients scheduled for maxillofacial surgery, dexamethasone injected prior to surgery significantly reduced post-operative edema. On the other hand, long-term administration of steroid mediates immune suppressive effects, and thus it can increase the possibility of postsurgical infection, weaken the skin thus inducing iatrogenic Cushing's syndrome, and decreases bone density [
21]. Studies on the side effects of dexamethasone administered prior to surgery have not yet been reported.
Henzi et al. [
22] have reported that in healthy patients, adverse effects of the injection of 8-10 mg of dexamethasone once for the prevention of nausea and vomiting prior to surgery was not proven. The dose of dexamethasone frequently used to prevent nausea and vomiting associated with surgery is 5-10 mg for adults. In our study, 10 mg of dexamethasone was administered.
A limitation of our study was that 10 mg of dexamethasone was administered regardless of the weight of patient, and thus studies on a more exact dose (i.e. based on mg/kg) of individual patients are required.
In conclusion, pretreatment with 10 mg of dexamethasone prior to the injection of remifentanil suppressed the development and severity of cough induced by remifentanil without significant adverse effects.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download