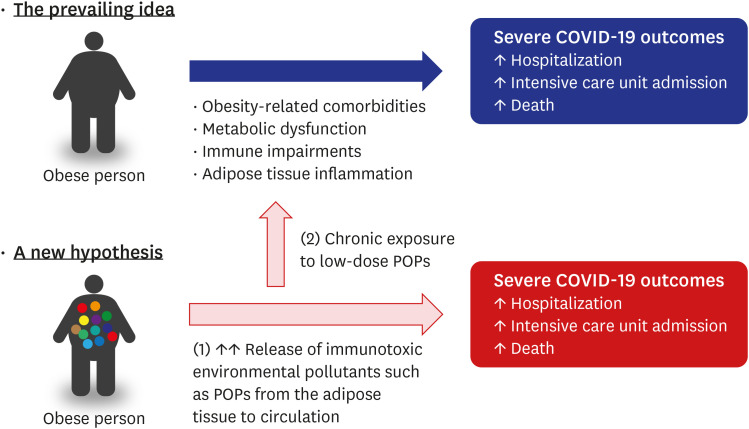
A recent meta-analysis reported that individuals with obesity have a greater risk of hospitalization, intensive care unit admission, and death from COVID-19.1 Particularly, obesity is a strong risk factor for hospitalization and death among adults aged < 65 years.2 Obesity has also been identified as an independent risk factor for severe morbidity and mortality during the H1N1 influenza3 and Middle East respiratory syndrome epidemics.4 Several mechanisms, such as obesity-related comorbidities, metabolic dysfunction, immune impairments, and adipose tissue inflammation, have been proposed to explain the link of obesity with COVID-19 and other respiratory infectious diseases.1
In this article, environmental pollutants are proposed as another possible mechanism to explain the higher risk of severe COVID-19 in obese individuals. Although it is largely unknown to researchers and clinicians, human adipose tissue is extensively contaminated with various environmental pollutants.56 Typical examples of environmental pollutants stored in the adipose tissue are persistent organic pollutants (POPs).
POPs are a group of organic compounds with common features, such as strong lipophilicity, high persistence in the environment due to resistance to degradation, bioaccumulation in the adipose tissue of living organisms, and prolonged half-lives reaching several years to decades in humans.7 Specific compounds include organochlorine pesticides, polychlorinated biphenyls, dioxins, and polybrominated diphenyl ethers. Many other chemicals that are not traditionally classified as POPs are also commonly detected in human adipose tissue.89
The immune system is one of the targets of xenobiotic-induced toxicity.10 Early epidemiological and toxicological studies have shown that various environmental chemicals, including POPs, impair the immune system at high doses.1112 Exposure to 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) induces several immunotoxic effects on both innate and adaptive immune responses through aryl hydrocarbon receptors.1314 In a previous study, TCDD administration to laboratory animals resulted in decreased resistance to numerous bacteria, viruses, and parasites.15 In addition to TCDD, other POPs, classified as organochlorine pesticides, polychlorinated biphenyls, and polybrominated diphenyl ethers, have also demonstrated immunotoxicity in many in vitro and in vivo studies.161718
Early toxicological studies have focused on the immunotoxicity of high doses of individual chemicals; however, recent studies have highlighted the effect of chronic exposure to low-dose environmental pollutants on the immune system.1920 In contemporary society, humans are chronically exposed to a tremendous number of low-dose environmental pollutants. Although many POPs were banned several decades ago, humans are still exposed to them in the form of lipophilic chemical mixtures because they have widely contaminated the food chain on earth.21
Studies on marine mammals have suggested that immunotoxicity may occur due to chronic exposure to low-dose environmental pollutants, because a wide array of environmental pollutants modulate the immune system.22 In addition, a recent human study demonstrated that chronic exposure to low-dose POPs was linked to T cell immunosenescence, which is a hallmark of an aging immune system.23 An aging immune system is directly related to the risk of increased susceptibility to infectious diseases.24
Currently, the most important source of exposure to POPs is inside the body—human adipose tissue. Once POPs enter the body through external sources, they are primarily stored in adipose tissue and are very slowly released into the circulation through lipolysis.25 Therefore, serum concentrations of POPs in humans, which are commonly used to assess the POP exposure status in epidemiological studies, reflect the quantity of POPs released from the adipose tissue into the circulation and are not directly related to the level of exposure to external sources of POPs. The accumulation of POPs in adipose tissue occurs throughout the lifetime—from the fetal stage to death. Therefore, although external sources of exposure to POPs would have been eliminated, POPs in adipose tissue still play a role as an internal exposure source and affect human health.
Under normal physiological conditions, adipose tissue lipolysis is tightly regulated by hormonal signals, depending on the caloric needs.26 Unlike lean healthy persons, in obese individuals POPs are released into the circulation more easily through uncontrolled lipolysis, which is a feature of hypertrophic dysfunctional adipocytes.27 Uncontrolled lipolysis is further enhanced by insulin resistance.28 Therefore, it is highly plausible that obese individuals show higher serum concentrations of POPs with immunotoxicity. This may be a possible mechanism for the relationship between obesity and the increased risk of morbidity and mortality in COVID-19.
It is worth noting that low-dose POPs have recently emerged as a risk factor for many metabolic diseases, including type-2 diabetes,729 which is another risk factor for increased morbidity and mortality in COVID-19. Also, low-dose POPs can induce pro-inflammatory change in adipose tissue regardless of obesity.3031 Therefore, chronic exposure to low-dose POPs can be a more fundamental factor to explain the higher risk of severe morbidity and mortality in patients with COVID-19 (Fig. 1).
Weight management is crucial for individuals who are overweight or obese. However, inadequate consideration of the dynamics of POPs during weight loss may lead to unexpected consequences.25 Intentional weight loss improves short-term clinical profiles, but a long-term consequence is the increased amount of POPs released from the adipose tissue into the circulation due to the shrinkage of the storage sites.32
This mechanism may explain the unexpected finding from a large randomized controlled study on intensive weight loss among overweight or obese patients with type 2 diabetes. In this clinical trial, the intensive weight loss group failed to attain any benefit on the development of cardiovascular diseases compared to the control group, despite an improvement in many known risk factors for cardiovascular diseases.33 Therefore, the ideal strategy of weight management should consider both fat mass and the dynamics of POPs.
With regards to the amount of adipose tissue mass, obesity and weight loss are opposites; obesity is the status of having a significant fat mass, while weight loss is the process of losing fat mass. However, both increase the release of POPs from adipose tissue into the circulation. The difference is that in obese patients small amounts of POPs are continuously released into circulation for a long period of time, but weight loss releases relatively large amounts of POPs during the period of weight loss.
POPs in circulation would be more harmful than POPs in the adipose tissue because of their easy access to critical organs. Therefore, dealing with POPs in circulation in everyday life is very important for both obese persons and those who want to lose weight. In fact, a healthy lifestyle consisting of proper diet and exercise has been suggested as a practical method to increase the elimination of POPs from the circulation and mitigate their possible harmful effects at the cellular level.333435363738 In addition, slow and steady weight loss is better than rapid weight loss because the increase in POPs in circulation during weight loss is proportional to the magnitude of weight loss.32
The dynamics of POPs accumulated in adipose tissue can be a possible mechanism to explain the relationship between obesity and severe COVID-19. Low-dose lipophilic chemical mixtures, such as POPs, add another challenge to weight management and emphasize the importance of preventing obesity. In this context, it is unfortunate that the containment strategy to combat the COVID-19 pandemic has worsened the obesity epidemic because social distancing and stay-at-home policies have hindered weight management.39 The relationship between obesity and environmental pollutants warrants further investigation by researchers, clinicians, and public health officials.
Notes
References
1. Popkin BM, Du S, Green WD, Beck MA, Algaith T, Herbst CH, et al. Individuals with obesity and COVID-19: a global perspective on the epidemiology and biological relationships. Obes Rev. 2020; 21(11):e13128. PMID: 32845580.

2. Kompaniyets L, Goodman AB, Belay B, Freedman DS, Sucosky MS, Lange SJ, et al. Body mass index and risk for COVID-19-related hospitalization, intensive care unit admission, invasive mechanical ventilation, and death - United States, March–December 2020. MMWR Morb Mortal Wkly Rep. 2021; 70(10):355–361. PMID: 33705371.

3. Louie JK, Acosta M, Samuel MC, Schechter R, Vugia DJ, Harriman K, et al. A novel risk factor for a novel virus: obesity and 2009 pandemic influenza A (H1N1). Clin Infect Dis. 2011; 52(3):301–312. PMID: 21208911.

4. Al-Tawfiq JA, Hinedi K, Ghandour J, Khairalla H, Musleh S, Ujayli A, et al. Middle East respiratory syndrome coronavirus: a case-control study of hospitalized patients. Clin Infect Dis. 2014; 59(2):160–165. PMID: 24723278.

5. Kim KS, Lee YM, Kim SG, Lee IK, Lee HJ, Kim JH, et al. Associations of organochlorine pesticides and polychlorinated biphenyls in visceral vs. subcutaneous adipose tissue with type 2 diabetes and insulin resistance. Chemosphere. 2014; 94:151–157. PMID: 24161582.

6. Moon HB, Lee DH, Lee YS, Choi M, Choi HG, Kannan K. Polybrominated diphenyl ethers, polychlorinated biphenyls, and organochlorine pesticides in adipose tissues of Korean women. Arch Environ Contam Toxicol. 2012; 62(1):176–184. PMID: 21594673.

7. Lee DH, Porta M, Jacobs DR Jr, Vandenberg LN. Chlorinated persistent organic pollutants, obesity, and type 2 diabetes. Endocr Rev. 2014; 35(4):557–601. PMID: 24483949.

8. Geens T, Neels H, Covaci A. Distribution of bisphenol-A, triclosan and n-nonylphenol in human adipose tissue, liver and brain. Chemosphere. 2012; 87(7):796–802. PMID: 22277880.

9. Moon HB, Lee DH, Lee YS, Kannan K. Occurrence and accumulation patterns of polycyclic aromatic hydrocarbons and synthetic musk compounds in adipose tissues of Korean females. Chemosphere. 2012; 86(5):485–490. PMID: 22055311.

10. De Jong WH, Van Loveren H. Screening of xenobiotics for direct immunotoxicity in an animal study. Methods. 2007; 41(1):3–8. PMID: 17161297.

11. Luster MI. A historical perspective of immunotoxicology. J Immunotoxicol. 2014; 11(3):197–202. PMID: 24083808.

12. Luster MI, Portier C, Pait DG, Germolec DR. Use of animal studies in risk assessment for immunotoxicology. Toxicology. 1994; 92(1-3):229–243. PMID: 7940563.

13. Pang C, Zhu C, Zhang Y, Ge Y, Li S, Huo S, et al. 2,3,7,8-Tetrachloodibenzo-p-dioxin affects the differentiation of CD4 helper T cell. Toxicol Lett. 2019; 311:49–57. PMID: 31014974.

14. Rothhammer V, Quintana FJ. The aryl hydrocarbon receptor: an environmental sensor integrating immune responses in health and disease. Nat Rev Immunol. 2019; 19(3):184–197. PMID: 30718831.

15. Holsapple MP, Snyder NK, Wood SC, Morris DL. A review of 2,3,7,8-tetrachlorodibenzo-p-dioxin-induced changes in immunocompetence: 1991 update. Toxicology. 1991; 69(3):219–255. PMID: 1949050.

16. Tryphonas H. Immunotoxicity of polychlorinated biphenyls: present status and future considerations. Exp Clin Immunogenet. 1994; 11(2-3):149–162. PMID: 7826664.

17. Voccia I, Blakley B, Brousseau P, Fournier M. Immunotoxicity of pesticides: a review. Toxicol Ind Health. 1999; 15(1-2):119–132. PMID: 10188195.

18. Lv QY, Wan B, Guo LH, Zhao L, Yang Y. In vitro immune toxicity of polybrominated diphenyl ethers on murine peritoneal macrophages: apoptosis and immune cell dysfunction. Chemosphere. 2015; 120:621–630. PMID: 25462306.

19. Germolec D, Luebke R, Rooney A, Shipkowski K, Vandebriel R, van Loveren H. Immunotoxicology: a brief history, current status and strategies for future immunotoxicity assessment. Curr Opin Toxicol. 2017; 5:55–59. PMID: 28989989.

20. Inadera H. The immune system as a target for environmental chemicals: Xenoestrogens and other compounds. Toxicol Lett. 2006; 164(3):191–206. PMID: 16697129.

21. Kelly BC, Ikonomou MG, Blair JD, Morin AE, Gobas FA. Food web-specific biomagnification of persistent organic pollutants. Science. 2007; 317(5835):236–239. PMID: 17626882.

22. Desforges JP, Sonne C, Levin M, Siebert U, De Guise S, Dietz R. Immunotoxic effects of environmental pollutants in marine mammals. Environ Int. 2016; 86:126–139. PMID: 26590481.

23. Ryu DH, Yu HT, Kim SA, Lee YM, Hong SH, Yoon YR, et al. Is chronic exposure to low-dose organochlorine pesticides a new risk factor of T-cell immunosenescence? Cancer Epidemiol Biomarkers Prev. 2018; 27(10):1159–1167. PMID: 29991517.

24. Pawelec G. T-cell immunity in the aging human. Haematologica. 2014; 99(5):795–797. PMID: 24790056.

25. Lee YM, Kim KS, Jacobs DR Jr, Lee DH. Persistent organic pollutants in adipose tissue should be considered in obesity research. Obes Rev. 2017; 18(2):129–139. PMID: 27911986.

26. Langin D. Control of fatty acid and glycerol release in adipose tissue lipolysis. C R Biol. 2006; 329(8):598–607. PMID: 16860278.

27. Saponaro C, Gaggini M, Carli F, Gastaldelli A. The subtle balance between lipolysis and lipogenesis: a critical point in metabolic homeostasis. Nutrients. 2015; 7(11):9453–9474. PMID: 26580649.

28. Morigny P, Houssier M, Mouisel E, Langin D. Adipocyte lipolysis and insulin resistance. Biochimie. 2016; 125:259–266. PMID: 26542285.

29. Lee YM, Jacobs DR Jr, Lee DH. Persistent organic pollutants and type 2 diabetes: a critical review of review articles. Front Endocrinol (Lausanne). 2018; 9:712. PMID: 30542326.

30. Ibrahim MM, Fjære E, Lock EJ, Naville D, Amlund H, Meugnier E, et al. Chronic consumption of farmed salmon containing persistent organic pollutants causes insulin resistance and obesity in mice. PLoS One. 2011; 6(9):e25170. PMID: 21966444.

31. Ruzzin J, Petersen R, Meugnier E, Madsen L, Lock EJ, Lillefosse H, et al. Persistent organic pollutant exposure leads to insulin resistance syndrome. Environ Health Perspect. 2010; 118(4):465–471. PMID: 20064776.

32. Jansen A, Lyche JL, Polder A, Aaseth J, Skaug MA. Increased blood levels of persistent organic pollutants (POP) in obese individuals after weight loss-A review. J Toxicol Environ Health B Crit Rev. 2017; 20(1):22–37. PMID: 28051929.

33. Lee DH, Jacobs DR Jr, Lind L, Lind PM. Lipophilic environmental chemical mixtures released during weight-loss: the need to consider dynamics. BioEssays. 2020; 42(6):e1900237. PMID: 32363609.

34. Lee DH, Jacobs DR Jr. New approaches to cope with possible harms of low-dose environmental chemicals. J Epidemiol Community Health. 2019; 73(3):193–197. PMID: 30635437.

35. Lee YM, Shin JY, Kim SA, Jacobs DR Jr, Lee DH. Can habitual exercise help reduce serum concentrations of lipophilic chemical mixtures? Association between physical activity and persistent organic pollutants. Diabetes Metab J. 2020; 44(5):764–774. PMID: 32174058.

36. Lee YM, Heo S, Kim SA, Lee DH. Is dietary macronutrient intake associated with serum concentrations of organochlorine pesticides in humans? Environ Pollut. 2020; 259:113819. PMID: 31887593.

37. Lee YM, Lee DH. Mitochondrial toxins and healthy lifestyle meet at the crossroad of hormesis. Diabetes Metab J. 2019; 43(5):568–577. PMID: 31694079.

38. Kim SA, Lee YM, Choi JY, Jacobs DR Jr, Lee DH. Evolutionarily adapted hormesis-inducing stressors can be a practical solution to mitigate harmful effects of chronic exposure to low dose chemical mixtures. Environ Pollut. 2018; 233:725–734. PMID: 29126094.

39. Senthilingam M. COVID-19 has made the obesity epidemic worse, but failed to ignite enough action. BMJ. 2021; 372(411):n411. PMID: 33664084.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download