Abstract
Background
Hypoglycemia is an important complication in the treatment of patients with diabetes. We surveyed the insight by patients with diabetes into hypoglycemia, their hypoglycemia avoidance behavior, and their level of worry regarding hypoglycemia.
Methods
A survey of patients with diabetes, who had visited seven tertiary referral centers in Daegu or Gyeongsangbuk-do, Korea, between June 2014 and June 2015, was conducted. The survey contained questions about personal history, symptoms, educational experience, self-management, and attitudes about hypoglycemia.
Results
Of 758 participants, 471 (62.1%) had experienced hypoglycemia, and 250 (32.9%) had experienced hypoglycemia at least once in the month immediately preceding the study. Two hundred and forty-two (31.8%) of the participants had received hypoglycemia education at least once, but only 148 (19.4%) knew the exact definition of hypoglycemia. Hypoglycemic symptoms identified by the participants were dizziness (55.0%), sweating (53.8%), and tremor (40.8%). They mostly chose candy (62.1%), chocolate (37.7%), or juice (36.8%) as food for recovering hypoglycemia. Participants who had experienced hypoglycemia had longer duration of diabetes and a higher proportion of insulin usage. The mean scores for hypoglycemia avoidance behavior and worry about hypoglycemia were 21.2±10.71 and 23.38±13.19, respectively. These scores tended to be higher for participants with higher than 8% of glycosylated hemoglobin, insulin use, and experience of emergency room visits.
Diabetes is a chronic disease that is increasing in prevalence worldwide. Glycemic control is the main treatment for patients with diabetes, and many studies provide evidence that glycemic control prevents or delays the development of microvascular complications of diabetes [123]. However, the occurrence or fear of hypoglycemia is a barrier to achieving glycemic control. When patients encounter hypoglycemia, they are less likely to comply with drug therapy and may have additional psychiatric problems in their daily lives [45]. Moreover, severe hypoglycemia increases cardiovascular mortality in old age or in the presence of comorbidities [678]. In the Action to Control Cardiovascular Risk in Diabetes Study (ACCORD) trial, the intensive therapy group (glycosylated hemoglobin [HbA1c] <6.0%) experienced higher mortality than did the standard therapy group (HbA1c, 7.0% to 7.9%), possibly due to more severe or frequent hypoglycemic events in the intensive therapy group [9]. Following the publication of these data, recent guidelines address concerns about hypoglycemia, especially in patients with comorbidities, and emphasize that therapy should be tailored to the individual [10].
For the prevention of hypoglycemia, the 2016 American Diabetes Association guidelines recommended a chronic care model (CCM), which would improve the clinical outcome and adherence to therapy, involving a team approach (doctors, nurses, dieticians, and social workers) [10]. In addition, repeated and frequent diabetes education must be undertaken regarding self-management to improve clinical outcomes and quality of life. This can be conducted through mass media, including television, radio, and newspaper [111213]. However, there is a lack of data regarding the insight of diabetic patients into hypoglycemia in a real-world setting. Therefore, in this study, we investigated the understanding by diabetes patients of hypoglycemia, the behavior they use to avoid hypoglycemia, and their fear of hypoglycemia, by using a questionnaire.
This study was conducted with the approval of the Keimyung University Dongsan Medical Center Institutional Review Board (IRB 2014-04-083). A survey of 758 patients with diabetes, who had visited seven tertiary referral centers (Kyungpook National University, Keimyung University Dongsan Medical Center, Catholic University of Daegu, Yeungnam University College of Medicine, Soonchunhyang University Gumi Hospital, CHA Gumi Medical Center, and Daegu Fatima Hospital), in Daegu or Gyeongsangbuk-do, Korea, between June 2014 and July 2015 was conducted. Patients with gestational diabetes mellitus were excluded. Written informed consent was obtained from all participants before completing the questionnaire.
The patients were asked questions regarding their personal history, type and duration of diabetes, type of medication (divided into categories of lifestyle modification, only oral hyperglycemic agents [OHAs] and insulin with or without OHAs, occupation, history of alcohol intake, history of smoking, and frequency of meals). They were also asked whether they knew their recent HbA1c, fasting glucose, or postprandial glucose levels. To establish what the patients knew about hypoglycemia, they were asked to answer to several questions, including the definition of hypoglycemia (writing the criteria of hypoglycemia), hypoglycemic symptoms (to select all the correct answers among a list of 12 hypoglycemic symptoms), and foods to eat during hypoglycemia (to select all the correct answers among a list of 15 foods). In a question regarding hypoglycemic symptoms, 12 correct hypoglycemic symptoms were presented as answer choices; selected answers were scored by each point and these scores were added up. In a question about what to eat during hypoglycemia, five correct foods and 10 incorrect foods were presented as answer choices; the correct answer was scored 1 point and an incorrect answer was scored −1 point, and then these scores were added up.
Patients were also asked where and how often they had received education regarding self-management of their diabetes. Further questions regarded their experience and frequency of hypoglycemia in the past month and what they did first during a hypoglycemic event. In addition, they were asked how often they checked their blood glucose, and they were surveyed about their behaviors and anxiety, using Hypoglycemia Fear Survey II behavior and worry subscales [1415]. The behavior subscale concerns 15 behaviors aimed at avoiding hypoglycemia, whereas the worry subscale includes 18 items about the daily life and work of the patients and how this correlates with hypoglycemia. All questions were scored 1 to 5 according to their frequency (never, rare, often, sometimes, always). Finally, patients were asked whether they informed their care team about hypoglycemic events when they visited their clinic.
Descriptive statistics were used to assess patient demographics, disease characteristics, and patient-reported outcomes. Differences between patients who had experienced recent hypoglycemic symptoms and those who had not were assessed using Student t-test for continuous variables and a chi-square test for categorical variables. Statistical significance was set a priori at P<0.05. All statistical analyses were performed using the SPSS version 22.0 (IBM Co., Armonk, NY, USA).
Of the 758 participants enrolled, 62.1% reported experience of hypoglycemia in the past, and 32.9% of participants recalled a hypoglycemic event at least once in the previous month. The average age of the participants was 56.3±13.7 years, and 51.5% were male (Table 1); 63.9% had type 2 diabetes mellitus, and a mean duration of diabetes of 11.8±9.7 years was reported. Therapy consisted of lifestyle modification for 4.2%, OHAs for 46.2%, and insulin for 47.1% of the participants; 20.5% of patients lived alone, and 60.4% reported consuming a normal diet. Among the participants who worked, 21.5% did so at night.
The participants were divided into two groups according to their experience of hypoglycemia. There were no differences between the two groups in age, sex, or body mass index. However, the group that had already experienced hypoglycemia had a longer duration of diabetes (13.9±9.8 years vs. 8.2±8.5 years, P=0.002) and higher rates of using insulin (57.7% vs. 29.4%, P<0.001) than the other group. In addition, the HbA1c of the hypoglycemia group was higher than that in the other group, although the difference was not statistically significant (8.5%±2.3% vs. 8.0%±2.1%, P=0.270).
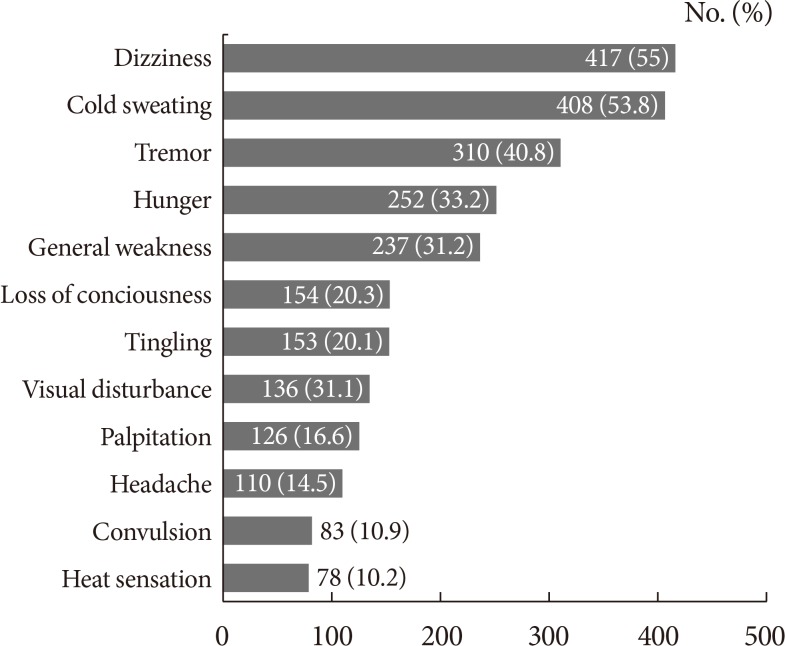
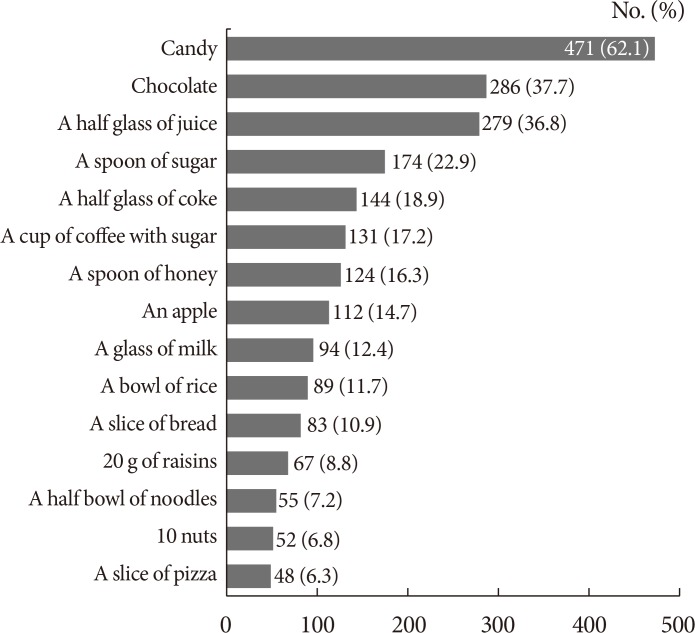
Of the participants, 77.4% had heard about hypoglycemia, and 31.9% recalled being personally educated about hypoglycemia (Table 2). Of these, 69.8% had received information in a clinic, 26.4% in a group, 2.8% in the public health system, and 10.7% through mass media, such as television or the Internet. The participants were also asked whether they knew the definition of hypoglycemia, and only 19.4% could accurately define hypoglycemia (<70 mg/dL); 23.5% of the participants undertook self-monitoring of blood glucose 2 to 3 times/day, but 23.8% only did this 2 to 3 times/week. A medical alert card was held by 10.9% of the participants. Of the 12 correct hypoglycemic symptoms listed in the questionnaire, dizziness (55.0%), sweating (53.8%), tremor (40.8%), hunger (33.2%), and general weakness (31.2%) were identified most frequently (Fig. 1). The mean score of choosing the correct hypoglycemic symptom was 3.3. When choosing foods to aid recovery from hypoglycemia, most patients selected the intake of candy (62.1%), chocolate (37.7%), or fruit juice (36.8%), but others also answered that they ate pizza (6.3%), raisins (8.8%), or nuts (6.8%) (Fig. 2). The mean total score of choosing food was 0.2.
Of the 758 participants, 471 participants (62.1%) experienced hypoglycemia (Table 3). In the previous month, 32.9% of participants had experienced hypoglycemia at least once, and 6.2% had experienced it more than four times. As expected, patients treated with insulin had a higher frequency of hypoglycemia than those without insulin (1.2±1.8 vs. 0.6±2.0, P<0.001). They reported hypoglycemia in the fasting state (at dawn) (39.4%), before a meal (35%), or during exercise (18%). When they felt the onset of hypoglycemia, many of the participants (49.1%) ate foods first, whereas 14.4% checked their blood glucose before eating, and 17.3% ate foods and then checked their blood glucose (Table 3).
Hypoglycemia avoidance behavior and the frequency with which participants worried about hypoglycemia were assessed using the Hypoglycemia Fear Survey II behavior and worry subscales (Table 4). The mean scores for hypoglycemia avoidance behavior and fear were 21.2±10.7 and 23.4±13.2, respectively. These scores were higher in patients who had experienced hypoglycemia, but were not statistically significant. However, the group using insulin and those patients with poor glycemic control (HbA1c ≥8%) and who had visited the emergency room (ER) had significantly higher scores for hypoglycemia avoidance behavior and fear.
Patients with diabetes were also asked whether they told their physician about their hypoglycemic episodes (Table 5). This questionnaire was added during the survey and had a total of 499 participants. A majority of participants (76.9%) confirmed that their doctors asked them about hypoglycemia, but 23.0% said that they did not. Furthermore, 51.5% of participants did not report hypoglycemic events to their physician during a routine appointment.
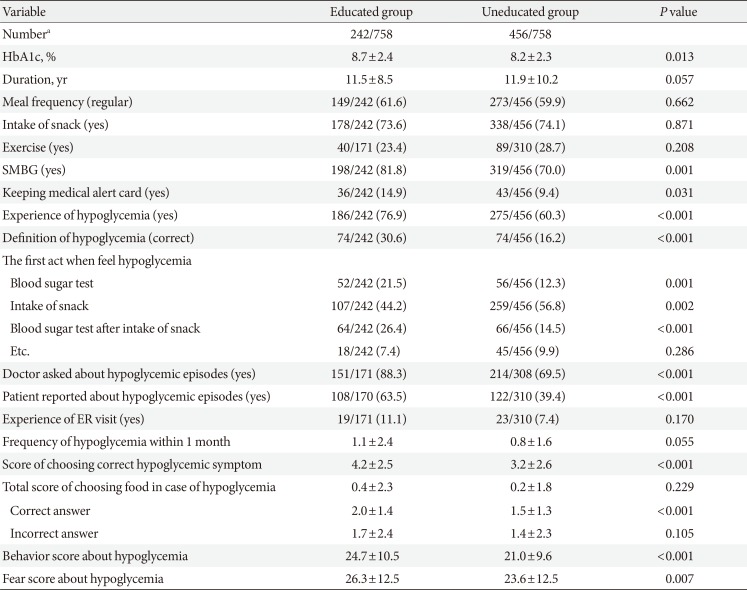
We evaluated whether there were differences of perspective of hypoglycemia according to education experience (Table 6). The educated group was better aware of hypoglycemia, including the definition of hypoglycemia (30.6% vs. 16.2%, P<0.001), symptoms that can appear in hypoglycemia (4.2±2.5 vs. 3.2±2.6, P<0.001), action to deal with hypoglycemia (21.5% vs. 12.3%, P=0.001), and communication with the doctor about hypoglycemia (doctor asked: 88.3% vs. 69.5%, P<0.001; patient reported: 63.5% vs. 39.4%, P<0.001). In addition, they had kept a medical alert card and checked their blood glucose level more than the other group (14.9% vs. 9.4%, P=0.031; 81.8% vs. 70.0%, P=0.001, respectively). There were no differences between the two groups in improving lifestyle habits (regular diet, exercise, restriction of snacks), experience visiting the ER due to hypoglycemia, knowledge of foods to eat during hypoglycemia, frequency of hypoglycemia within the past month. In addition, the educated group had higher HbA1c and higher behavior and fear scores.
In this study, about 60% of participants reported experiencing hypoglycemia, but many subjects could not identify symptoms of hypoglycemia or what they should do after detecting them. Participants who had poor glucose control (HbA1c ≥8%), were treated with insulin, and had visited the ER yielded higher scores for both hypoglycemia avoidance behavior and fear of hypoglycemia. However, many participants did not report hypoglycemic events to their doctor before they were asked.
Hypoglycemia is defined as a blood glucose of <70 mg/dL, accompanied by sweating, dizziness, and other symptoms [1617]. Mild hypoglycemia can usually be self-treated, whereas severe hypoglycemia is defined by a requirement for external assistance [1016]. Hypoglycemia is especially common in older patients or in those with comorbidities, in whom it affects compliance with medical therapy, lifestyle, and mortality. Recent guidelines emphasize that therapeutic regimens should be tailored to the needs of specific patients, rather than being aimed purely at achieving glycemic control within a near-normal range [10]. This is because hypoglycemia can cause very serious consequences, sometimes resulting in the death of patients with cardiovascular disease [6789]. The incidence of hypoglycemia varies according to the type of diabetes, therapeutic regimen, and age of diabetic patients. In a review of 46 studies (n=532,542) of hypoglycemia, the prevalence of hypoglycemia was 45% for mild/moderate events and 6% for severe events. The incidences of mild/moderate and severe hypoglycemic episodes per person-year were 19 (95% CI, 0.00 to 51.08) and 0.80 (95% CI, 0.00 to 2.15), respectively [18]. In this study, about 60% of participants reported experiencing hypoglycemia, but many participants could not identify the symptoms of hypoglycemia or what they should do after detecting them. In addition, a third of participants could not define hypoglycemia at the time of the study.
Diabetes self-management education (DSME) is an important element of diabetes care, in particular in the prevention or delay of the development of diabetic complications [1319202122]. Patients should learn about their optimal daily care and how to act under various circumstances. For effective education, it is important to know how well-informed each patient is. In the present survey, only 19.4% of patients could define hypoglycemia correctly (<70 mg/dL), and from the list of 12 correct hypoglycemic symptoms, participants could identify only a mean of 3.3. Most patients did not know that symptoms such as headache, perspiration, and seizure can occur during hypoglycemia. Although many participants chose candy as an immediate treatment for hypoglycemia, others chose chocolate, rice, or nuts. In addition, many consumed candy without checking their blood glucose beforehand. Finally, only 10.9% of patients had kept their medical alert cards. Even though the groups of patients who received hypoglycemia education were segregated, the results were not much different. The educated group showed better results in some of questions. However, they had a lower proportion of correct answers in these questions, Moreover, they showed no significant difference or worse results compared to the uneducated group in other questions. These results show that many patients with diabetes are not well-informed regarding hypoglycemia, even though they have received some education.
The occurrence of hypoglycemia limits daily activities and lowers quality of life [2324252627]. According to surveys of the fear associated with hypoglycemia in type 1 diabetes mellitus, patients prefer to try to keep their blood glucose higher than recommended, limit activities such as visiting friends, display emotional deficits, such as low confidence, and can also suffer psychiatric problems, such as panic attack or agoraphobia [28]. In addition, patients who experienced hypoglycemia had poorer health and were more likely to be depressed than those who did not experience hypoglycemic events [4].
Chronic untreated hypoglycemia can result in cerebral maladaptation, causing impaired awareness of hypoglycemia, which is termed “hypoglycemic unawareness” [29], and increases the fear of hypoglycemia [30]. Some studies reported a positive correlation between this fear and HbA1c, but this result was inconsistent [2531]. In addition, it was shown that a single episode of hypoglycemia can trigger anxiety, resulting in the development of avoidance behavior aimed at maintaining higher than recommended blood glucose levels [243132]. Similar to the results of other studies, the group using insulin and those patients with an HbA1c of >8.0% had significantly higher scores for avoidance behavior and worry about hypoglycemia. In addition, the group that had already experienced visits to the ER due to hypoglycemia tended to have higher avoidance behavior and fear scores than the group without ER visits due to hypoglycemia.
Patients who worry about hypoglycemia tend to eat more to avoid it, and, as their HbA1c increases, their doctors may add additional medication to control hyperglycemia without talking about hypoglycemia. Therefore, if communication is insufficient to identify this problem, patients may enter a vicious cycle of overmedication. Recently, the CCM was introduced, which is a well-rounded approach to restructuring medical care that involves partnerships between health systems and communities in U.S. primary care settings [10]. For this, physicians are trained to deliver evidence-based care, support decision making, and offer DSME through personal or group sessions. The design of the delivery system incorporates diabetes days, which facilitates communication between patients and diabetes educators. In this patient-centered approach, patients and diabetes educators create patient records collaboratively and can discuss treatment in more detail. Studies using CCM showed that it improved not only metabolic parameters, such as HbA1c and high density lipoprotein, but also psychosocial parameters, such as diabetes knowledge and empowerment scores [333435].
Surprisingly, Ostenson et al. [36] reported that almost half of patients rarely or never informed their general practitioner or specialist of a hypoglycemic event, despite over half of them had experienced such events. Similarly, in the present study, only half of the patients informed their physician of a hypoglycemic event before they were asked. These results show that improved communication between physicians and patients is important to provide better treatment.
This study has a few limitations. Data were collected using questionnaires, the accuracy of which depended on the memory of the patients. Patient recall is typically subjective, and here it did not correlate with the extent of the education provided by the respective care teams. The participants in the survey had a higher proportion of insulin treatment than general patients, so the possibility of selection bias must be considered. However, our data are made more relevant because they identify the level of patient knowledge regarding hypoglycemia in a real-world clinical care situation. Taken together, our results indicate that many patients have a lower degree of knowledge about hypoglycemia than was expected, and a greater level of worry. Furthermore, many patients did not tell their doctor about hypoglycemic events that they had experienced. Therefore, to ensure optimal treatment of diabetes and fewer hypoglycemic events, an improved system of communication between patients and their care teams should be established, including a better education program regarding diabetes self-management.
ACKNOWLEDGMENTS
We gratefully acknowledge the dietitians and medical social workers who helped conduct the survey. We would also like to thank the support of the Daegyeong Diabetes Endocrine Society.
References
1. Diabetes Control and Complications Trial Research Group. Nathan DM, Genuth S, Lachin J, Cleary P, Crofford O, Davis M, Rand L, Siebert C. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993; 329:977–986. PMID: 8366922.

2. Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med. 2008; 358:580–591. PMID: 18256393.

3. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998; 352:837–853. PMID: 9742976.
4. Green AJ, Fox KM, Grandy S. SHIELD Study Group. Self-reported hypoglycemia and impact on quality of life and depression among adults with type 2 diabetes mellitus. Diabetes Res Clin Pract. 2012; 96:313–318. PMID: 22296853.

5. Williams SA, Pollack MF, Dibonaventura M. Effects of hypoglycemia on health-related quality of life, treatment satisfaction and healthcare resource utilization in patients with type 2 diabetes mellitus. Diabetes Res Clin Pract. 2011; 91:363–370. PMID: 21251725.

6. Zhao Y, Campbell CR, Fonseca V, Shi L. Impact of hypoglycemia associated with antihyperglycemic medications on vascular risks in veterans with type 2 diabetes. Diabetes Care. 2012; 35:1126–1132. PMID: 22432106.

7. Zoungas S, Patel A, Chalmers J, de Galan BE, Li Q, Billot L, Woodward M, Ninomiya T, Neal B, MacMahon S, Grobbee DE, Kengne AP, Marre M, Heller S. ADVANCE Collaborative Group. Severe hypoglycemia and risks of vascular events and death. N Engl J Med. 2010; 363:1410–1418. PMID: 20925543.

8. Hsu PF, Sung SH, Cheng HM, Yeh JS, Liu WL, Chan WL, Chen CH, Chou P, Chuang SY. Association of clinical symptomatic hypoglycemia with cardiovascular events and total mortality in type 2 diabetes: a nationwide population-based study. Diabetes Care. 2013; 36:894–900. PMID: 23223349.
9. Action to Control Cardiovascular Risk in Diabetes Study Group. Gerstein HC, Miller ME, Byington RP, Goff DC Jr, Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm RH Jr, Probstfield JL, Simons-Morton DG, Friedewald WT. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008; 358:2545–2559. PMID: 18539917.
10. Standards of medical care in diabetes-2016: summary of revisions. Diabetes Care. 2016; 39(Suppl 1):S4–S5. PMID: 26696680.
11. Cooke D, Bond R, Lawton J, Rankin D, Heller S, Clark M, Speight J. U.K. NIHR DAFNE Study Group. Structured type 1 diabetes education delivered within routine care: impact on glycemic control and diabetes-specific quality of life. Diabetes Care. 2013; 36:270–272. PMID: 23139374.
12. Cochran J, Conn VS. Meta-analysis of quality of life outcomes following diabetes self-management training. Diabetes Educ. 2008; 34:815–823. PMID: 18832286.

13. Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002; 25:1159–1171. PMID: 12087014.
14. Gonder-Frederick LA, Schmidt KM, Vajda KA, Greear ML, Singh H, Shepard JA, Cox DJ. Psychometric properties of the hypoglycemia fear survey-II for adults with type 1 diabetes. Diabetes Care. 2011; 34:801–806. PMID: 21346182.

15. Cox DJ, Irvine A, Gonder-Frederick L, Nowacek G, Butterfield J. Fear of hypoglycemia: quantification, validation, and utilization. Diabetes Care. 1987; 10:617–621. PMID: 3677982.

16. Zammitt NN, Frier BM. Hypoglycemia in type 2 diabetes: pathophysiology, frequency, and effects of different treatment modalities. Diabetes Care. 2005; 28:2948–2961. PMID: 16306561.
18. Edridge CL, Dunkley AJ, Bodicoat DH, Rose TC, Gray LJ, Davies MJ, Khunti K. Prevalence and incidence of hypoglycaemia in 532,542 people with type 2 diabetes on oral therapies and insulin: a systematic review and meta-analysis of population based studies. PLoS One. 2015; 10:e0126427. PMID: 26061690.

19. Brown SA. Interventions to promote diabetes self-management: state of the science. Diabetes Educ. 1999; 25(6 Suppl):52–61. PMID: 10711085.

20. Gary TL, Genkinger JM, Guallar E, Peyrot M, Brancati FL. Meta-analysis of randomized educational and behavioral interventions in type 2 diabetes. Diabetes Educ. 2003; 29:488–501. PMID: 12854339.

21. Deakin T, McShane CE, Cade JE, Williams RD. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2005; (2):CD003417. PMID: 15846663.

22. Renders CM, Valk GD, Griffin SJ, Wagner EH, Eijk Van JT, Assendelft WJ. Interventions to improve the management of diabetes in primary care, outpatient, and community settings: a systematic review. Diabetes Care. 2001; 24:1821–1833. PMID: 11574449.
23. Brod M, Christensen T, Thomsen TL, Bushnell DM. The impact of non-severe hypoglycemic events on work productivity and diabetes management. Value Health. 2011; 14:665–671. PMID: 21839404.

24. Wild D, von Maltzahn R, Brohan E, Christensen T, Clauson P, Gonder-Frederick L. A critical review of the literature on fear of hypoglycemia in diabetes: implications for diabetes management and patient education. Patient Educ Couns. 2007; 68:10–15. PMID: 17582726.

25. Cox DJ, Gonder-Frederick L, Antoun B, Clarke W, Cryer P. Psychobehavioral metabolic parameters of severe hypoglycemic episodes. Diabetes Care. 1990; 13:458–459. PMID: 2318112.

26. Shiu AT, Wong RY. Fear of hypoglycaemia among insulin-treated Hong Kong Chinese patients: implications for diabetes patient education. Patient Educ Couns. 2000; 41:251–261. PMID: 11042428.

27. Marrett E, Radican L, Davies MJ, Zhang Q. Assessment of severity and frequency of self-reported hypoglycemia on quality of life in patients with type 2 diabetes treated with oral antihyperglycemic agents: a survey study. BMC Res Notes. 2011; 4:251. PMID: 21777428.

28. Green L, Feher M, Catalan J. Fears and phobias in people with diabetes. Diabetes Metab Res Rev. 2000; 16:287–293. PMID: 10934458.

29. Vignesh JP, Mohan V. Hypoglycaemia unawareness. J Assoc Physicians India. 2004; 52:727–732. PMID: 15839452.
30. Polonsky WH, Davis CL, Jacobson AM, Anderson BJ. Correlates of hypoglycemic fear in type I and type II diabetes mellitus. Health Psychol. 1992; 11:199–202. PMID: 1618174.

31. Irvine AA, Cox D, Gonder-Frederick L. Fear of hypoglycemia: relationship to physical and psychological symptoms in patients with insulin-dependent diabetes mellitus. Health Psychol. 1992; 11:135–138. PMID: 1582382.

32. Gold AE, Frier BM, MacLeod KM, Deary IJ. A structural equation model for predictors of severe hypoglycaemia in patients with insulin-dependent diabetes mellitus. Diabet Med. 1997; 14:309–315. PMID: 9113485.

33. Piatt GA, Orchard TJ, Emerson S, Simmons D, Songer TJ, Brooks MM, Korytkowski M, Siminerio LM, Ahmad U, Zgibor JC. Translating the chronic care model into the community: results from a randomized controlled trial of a multifaceted diabetes care intervention. Diabetes Care. 2006; 29:811–817. PMID: 16567820.

34. Piatt GA, Anderson RM, Brooks MM, Songer T, Siminerio LM, Korytkowski MM, Zgibor JC. 3-Year follow-up of clinical and behavioral improvements following a multifaceted diabetes care intervention: results of a randomized controlled trial. Diabetes Educ. 2010; 36:301–309. PMID: 20200284.
35. Stellefson M, Dipnarine K, Stopka C. The chronic care model and diabetes management in US primary care settings: a systematic review. Prev Chronic Dis. 2013; 10:E26. PMID: 23428085.

36. Ostenson CG, Geelhoed-Duijvestijn P, Lahtela J, Weitgasser R, Markert Jensen M, Pedersen-Bjergaard U. Self-reported non-severe hypoglycaemic events in Europe. Diabet Med. 2014; 31:92–101. PMID: 23796113.
Table 1
Basic characteristics of participants
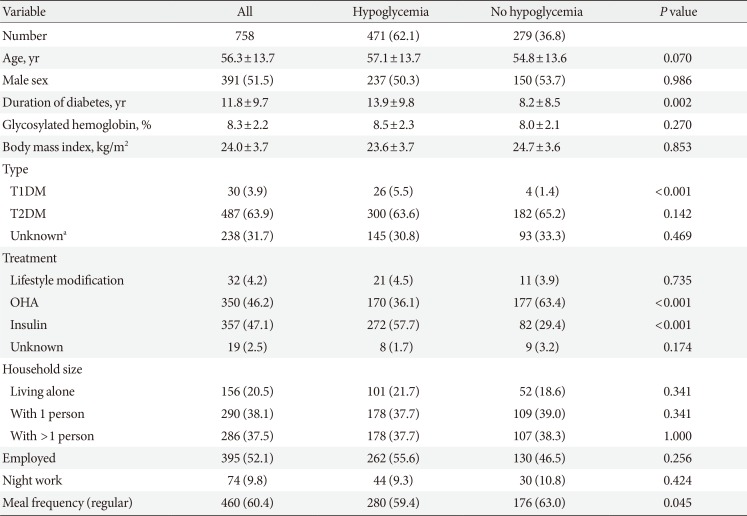
Table 2
Knowledge of patients regarding hypoglycemia
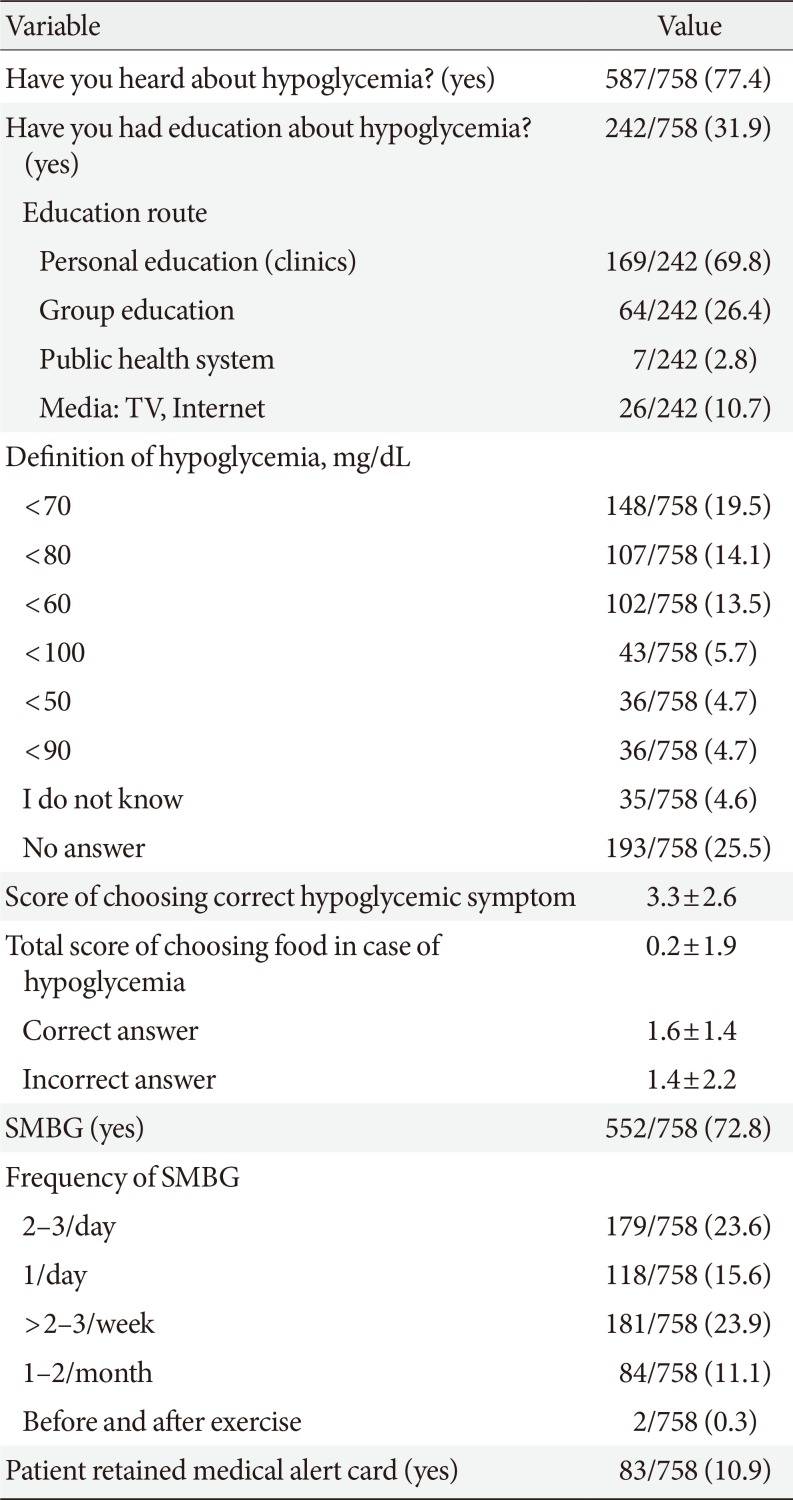
Table 3
Experience of patients with hypoglycemia
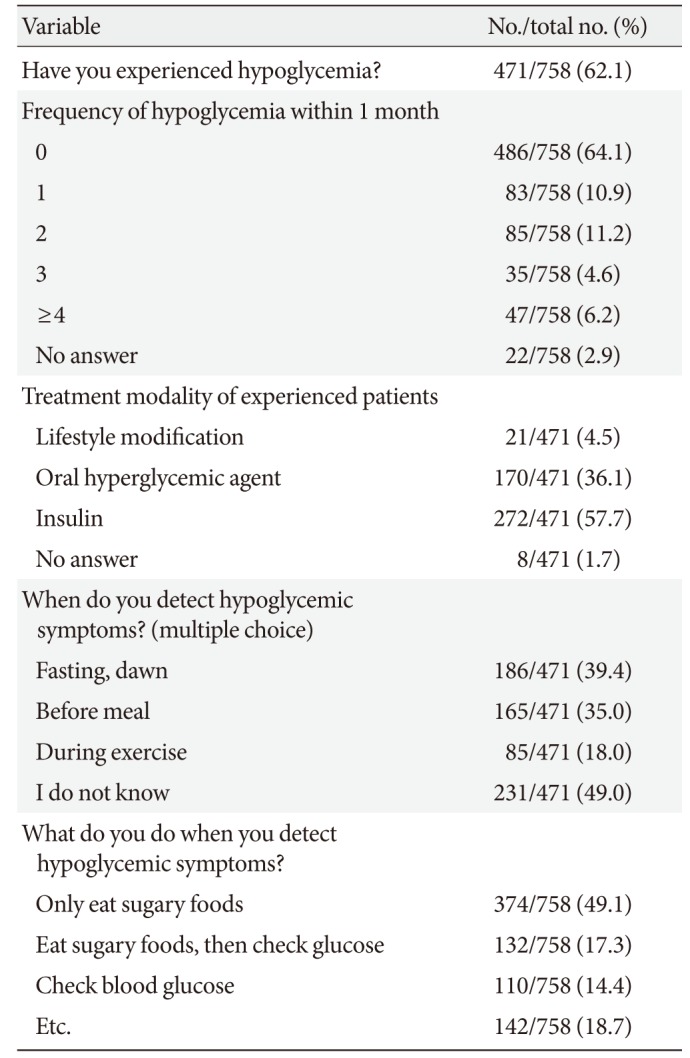
Table 4
Measures of behavior and worry about hypoglycemia
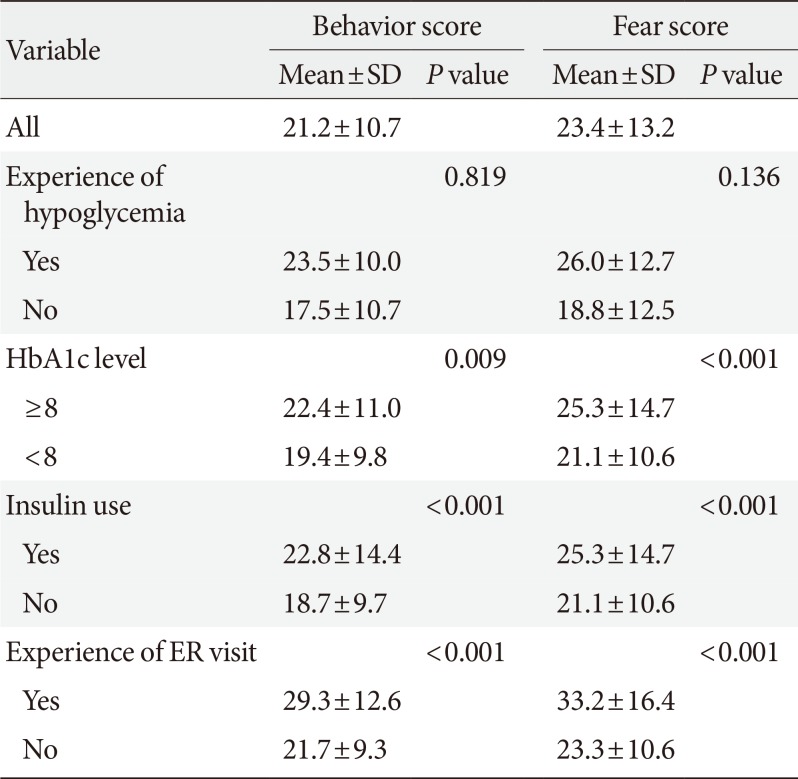
Table 5
Communication between physicians and patients with diabetes
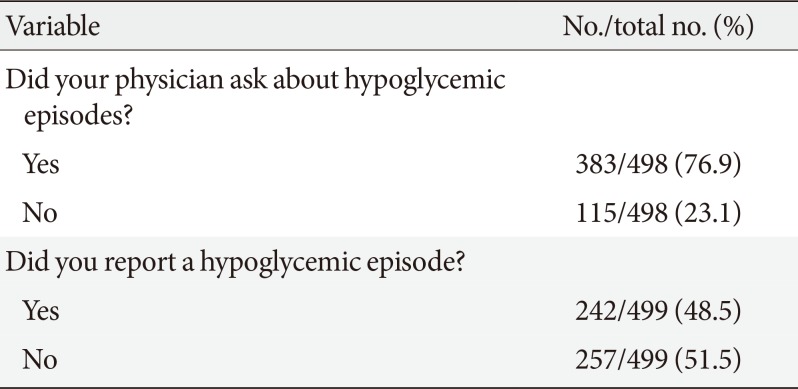
| Variable | No./total no. (%) |
|---|---|
| Did your physician ask about hypoglycemic episodes? | |
| Yes | 383/498 (76.9) |
| No | 115/498 (23.1) |
| Did you report a hypoglycemic episode? | |
| Yes | 242/499 (48.5) |
| No | 257/499 (51.5) |
Table 6
The difference between groups according to hypoglycemia education




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download