Abstract
The optimal dose of beta blockers after acute myocardial infarction (MI) remains uncertain. We evaluated the effectiveness of low-dose nebivolol, a beta1 blocker and a vasodilator, in patients with acute MI. A total of 625 patients with acute MI from 14 teaching hospitals in Korea were divided into 2 groups according to the dose of nebivolol (nebistol®, Elyson Pharmaceutical Co., Ltd., Seoul, Korea): low-dose group (1.25 mg daily, n=219) and usual- to high-dose group (≥2.5 mg daily, n=406). The primary endpoints were major adverse cardiac and cerebrovascular events (MACCE, composite of death from any cause, non-fatal MI, stroke, repeat revascularization, rehospitalization for unstable angina or heart failure) at 12 months. After adjustment using inverse probability of treatment weighting, the rates of MACCE were not different between the low-dose and the usual- to high-dose groups (2.8% and 3.1%, respectively; hazard ratio: 0.92, 95% confidence interval: 0.38 to 2.24, p=0.860). The low-dose nebivolol group showed higher rates of MI than the usual- to high-dose group (1.2% and 0%, p=0.008). The 2 groups had similar rates of death from any cause (1.1% and 0.3%, p=0.273), stroke (0.4% and 1.1%, p=0.384), repeat PCI (1.2% and 0.8%, p=0.428), rehospitalization for unstable angina (1.2% and 1.0%, p=0.743) and for heart failure (0.6% and 0.7%, p=0.832). In patients with acute MI, the rates of MACCE for low-dose and usual- to high-dose nebivolol were not significantly different at 12-month follow-up.
In patients with acute myocardial infarction (MI), beta blocker therapy reduces infarct size and mortality.123456 However, the optimal dosing and duration of beta blockade have not been established. In the real world, patients are often treated with lower doses of beta blockers than used in the clinical trials and the outcomes seem not different between lower and higher doses,789 which calls into question the benefit of high-dose beta blocker therapy in patients with acute MI.
Nebivolol is a selective beta1-receptor antagonist that exerts vasodilatory properties and improves endothelial function via its stimulatory effects on endothelial cell nitric oxide synthase.1011121314 In a recent observational study, treatment with vasodilating beta blockers including nebivolol was associated with better clinical outcomes after acute MI compared to conventional beta blocker therapy.15 Currently, however, there is a paucity of data on the benefits of nebivolol in patients with acute MI according to its doses.
In the present study, we sought to evaluate the clinical benefits of low-dose nebivolol in patients with acute MI, employing a multi-center, acute MI database in Korea.
In the present multi-center observational trial, Nebivolol in Acute MI Study (NAMIS), a total of 776 patients with acute MI having hypertension or heart failure who received nebivolol (nebistol®, Elyson Pharmaceutical Co., Ltd., Seoul, Korea) were enrolled from 14 teaching hospitals in Korea between July 2015 and December 2017. Inclusion criteria were: 1) consecutive patients aged ≥18 years, 2) patients with acute MI, defined as a rise and/or fall of cardiac biomarker values (troponin I/T or creatine kinase-MB with at least one value above the 99th percentile upper reference limit) with at least one of the following: symptoms of myocardial ischemia, changes on the electrocardiogram including new or presumed new significant ST-segment-T wave changes, new left bundle branch block, or pathologic Q waves in 2 contiguous leads, and imaging evidence of new loss of viable myocardium or a new regional wall motion abnormality,16 and 3) patients having at least one of the 2 following indications for nebivolol use in accordance with the Korean Ministry of Food and Drug Safety: hypertension, defined as a history of hypertension diagnosed and treated with medication, diet and/or exercise, or currently being on antihypertensive pharmacologic therapy; or heart failure, defined as a history of heart failure or left ventricular ejection fraction (LVEF) <50% or diastolic E/e′ ratio >15 on echocardiography. Exclusion criteria were patients with a history of bronchial asthma, or those with cardiogenic shock, significant bradycardia (<50 beats/min), second- or third-degree heart block, or renal dysfunction (serum creatinine >2.8 mg/dL). Patients who had received a beta blocker within the previous 2 months were also excluded.
Out of 776 patients, a total of 625 patients were divided into 2 groups according to their dose of nebivolol at discharge: low-dose group (1.25 mg daily, n=219) and usualto high-dose group (≥2.5 mg daily, n=406). A low dose was defined as less than 25% of the maximum recommended therapeutic dose (nebivolol 10 mg daily), whereas a high dose was defined as exceeding or equal to 50% of the maximum recommended therapeutic dose.717 Patients whose initial nebivolol dosing was unavailable (n=10) and those who switched between low doses and usual to high dose (n=141) were excluded.
PCI was performed according to the standard guidelines.1819 Patients received loading doses of aspirin (300 mg) and a P2Y12 inhibitor (ticagrelor 180 mg, prasugrel 60 mg, or clopidogrel 300-600 mg) before PCI. The selection of vessels treated, devices used, and adjunctive drugs administered to support PCI was left to the discretion of the treating physician. After PCI, patients received maintenance doses of either ticagrelor (90 mg twice daily), prasugrel (10 mg daily) or clopidogrel (75 mg daily). Aspirin was given at a dose of 100 mg daily. The present study was conducted according to the Declaration of Helsinki. The institutional review board of all participating centers approved the study protocol. The approval number was CNUH-2015-016 of Chonnam National University Hospital. Written informed consent was obtained from all participating patients.
The primary end point was major adverse cardiovascular and cerebrovascular events (MACCE), defined as a composite of death from any cause, MI, stroke, any repeat revascularization, or rehospitalization for unstable angina or heart failure. Secondary end points were individual components of the primary end point at 12 months. Target vessel revascularization was defined as a repeat PCI of any segment within the entire major coronary vessel proximal and distal to a target lesion, including the target lesion itself. Stroke was defined as focal loss of neurologic function caused by an ischemic or hemorrhagic event, with residual symptoms lasting at least 24 hours or leading to death.20
Continuous variables, expressed as mean±standard deviation or median (interquartile range), were compared using the Student t test or the Mann-Whitney U test. Categorical variables, reported as frequencies and percentages, were compared with the Chi-square test or Fisher's exact test, as appropriate.
In order to control for differences in baseline characteristics and potential confounding factors, an inverse probability of treatment weighting (IPTW) approach based on the propensity score was used.2122 The propensity score was constructed using a multiple logistic regression model that estimated the probability of receiving low-dose nebivolol conditional on 28 covariates shown in Table 1: age, sex, body mass index, smoking, hypertension, diabetes mellitus, dyslipidemia, prior history of MI, heart failure, family history of coronary artery disease, systolic blood pressure, diastolic blood pressure, heart rate, Killip class, clinical diagnosis (ST-segment elevation MI), LVEF, diastolic E/e′ ratio, serum creatinine, PCI, and use of aspirin, clopidogrel, ticagrelor, prasugrel, angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, nitrate, spironolactone, and statin. The Hosmer-Lemeshow goodness-of-fit test p value was 0.278, indicating good calibration and fit of the multivariable model that estimated the propensity score. Each patient was then weighted by the inverse probability of treatment received, and weighting was stabilized by multiplying the marginal probability of treatment.23 Baseline covariate balance between the 2 groups before and after IPTW was assessed using standardized differences. Variables were considered well balanced if the standardized difference was less than 10%.21 For comparison of clinical outcomes between the 2 groups, a weighted Cox proportional hazards model was used to estimate hazard ratios (HR) and their 95% confidence intervals (CI) for each outcome using a robust sandwich-type estimator to account for the weighted nature of the sample.24
All p values were 2-sided, with statistical significance set at a level of <0.05. Statistical analyses were conducted using Stata version 15.1 (StataCorp, College Station, TX, USA) and R version 3.5.1 (R Foundation for Statistical Computing, Vienna, Austria).
Baseline clinical characteristics of the patients are shown in Table 1. In the overall study population, patients who received low-dose nebivolol, compared to those receiving usual- to high-dose nebivolol, were more likely to have a prior history of heart failure, lower systolic and diastolic blood pressures and heart rate at admission, higher Killip class, and were more likely to have received prasugrel. Patients who received usual- to high-dose nebivolol were more likely to have hypertension, family history of coronary artery disease, and to receive angiotensin-converting enzyme inhibitors and nitrates. After IPTW adjustment, there were no differences between the 2 groups in the baseline clinical characteristics and medical treatment at hospital discharge (Table 1). Between discharge and 12 months, 95.7% of patients remained on the same daily dose (low dose 35.0%). Among patients who had a dose change, 1.6% had a reduction in dose and 2.7% had an increase in dose (Fig. 1).
In the overall patients, low-dose and usual- to high-dose groups had similar systolic blood pressure (124.7±14.9 mmHg and 125.1±13.4 mmHg, p=0.846), diastolic blood pressure (73.4±9.7 mmHg and 74.7±9.3 mmHg, p=0.331), and heart rate (62.6±22.0 beats/min and 59.1±28.5 beats/min, p=0.352) at 12 months. After IPTW adjustment, there were no differences between the 2 groups in the systolic blood pressure (124.7±14.5 mmHg and 125.5±13.1 mmHg, p=0.708), diastolic blood pressure (73.7±9.9 mmHg and 74.7±8.7 mmHg, p=0.488), and heart rate (64.0±21.8 beats/min and 60.6±26.7 beats/min, p=0.332).
Unadjusted and adjusted clinical outcomes at 12 months are shown in Table 2. In the IPTW-adjusted sample, patients who received low-dose nebivolol, compared with those receiving usual- to high-dose nebivolol, had a similar incidence of MACCE (2.8% and 3.1%, hazard ratio: 0.92, 95% confidence interval: 0.38 to 2.24, p=0.860, Fig. 2). The low-dose group showed a higher rate of MI than the usual- to high-dose group (1.2% and 0%, p=0.008). The 2 groups had similar rates of death from any cause (1.1% and 0.3%, p=0.273), stroke (0.4% and 1.1%, p=0.384), repeat PCI (1.2% and 0.8%, p=0.428), rehospitalization for unstable angina (1.2% and 1.0%, p=0.743) and for heart failure (0.6% and 0.7%, p=0.832).
The present study showed that in patients with acute MI, nebivolol both at low and usual to high doses resulted in comparable clinical outcomes at 12-month follow-up.
In patients with acute MI, beta blocker therapy is recommended as it reduces infarct size and mortality.123456 However, the optimal use of a beta blocker including its dose and duration remains uncertain. In the real world, patients are frequently treated with lower doses of beta blockers than used in the randomized clinical trials.789 Outcomes of Beta blocker Therapy After Myocardial Infarction study, an observational multicenter trial, evaluated the association between dose and survival in 6,682 patients with acute MI discharged on beta blocker treatment.7 Most patients were discharged on a low-dose beta blocker, with a mean dose at 38.1% of the target dose without significant difference in 2-year mortality compared to patients receiving a high-dose beta blocker. In a recent observational study in 11,909 post-MI patients from the Korea Acute Myocardial Infarction Registry, 69% of the patients received low doses of beta blockers and the use of beta blockers was associated with lower mortality compared with no use of beta blocker therapy.8 However, there was no significant difference between low-dose and high-dose beta blocker cohorts in 1-year cardiac mortality. Another retrospective study from the Intermountain Heart Collaborative Study Registry including 5,287 patients with acute coronary syndrome showed that 87% were discharged on low-dose beta blockers and low-dose beta-blocker therapy had a decreased risk of MI during the first 6 months. However, the rates of composite major adverse cardiac events during the 6 to 24 months were similar between low and high doses.9 These findings question the role of high-dose beta blocker therapy in patients with acute MI, raising the possibility that doses lower than used in clinical trials may produce similar or more favorable outcomes.
The evidence supporting beta blocker therapy after acute MI is based on randomized studies performed before the advent of reperfusion therapy such as fibrinolysis or PCI.25262728 A meta-analysis of these trials showed a 25% mortality reduction at one year with the use of propranolol, metoprolol, or atenolol.1 Hence, the benefit of beta blockers might have been diluted by the effect of PCI, dual antiplatelet therapy, and statins that are currently the standard treatment for acute MI, highlighting the need for further investigation for optimal does of beta blocker therapy after acute MI in contemporary practice.
Nebivolol is a third-generation selective beta1-receptor antagonist that exerts vasodilatory properties and improves endothelial function via its stimulatory effects on endothelial cell nitric oxide synthase as well as providing anti-atherosclerotic activity via its inhibitory effects on oxidative stress and vascular smooth muscle proliferation.1011121314 In mouse models of acute MI, nebivolol improved left ventricular dysfunction and survival.29 In the Study of the Effects of Nebivolol Intervention on Outcomes and Rehospitalisation in Seniors with Heart Failure, nebivolol proved to be effective and well-tolerated in elderly patients with heart failure.17 In addition, a recent observational study revealed that treatment with vasodilating beta blockers including nebivolol was associated with a lower risk of cardiac mortality and better clinical outcomes in patients with acute MI compared to conventional beta blocker therapy.15
Currently, however, there is a paucity of data on the benefits of nebivolol in patients with acute MI according to its doses. The results of the present study are in line with the preceding studies,789 showing similar incidence of MACCE at 12 months with low-dose nebivolol, compared to usual- to high-dose nebivolol. The incidence of MI was higher in the low-dose group but this needs to be assessed in further large-scale randomized study, given that the sample size of the present study was relatively small and the baseline profiles were worse with the low-dose group.
The present study has several limitations. First, this study is limited because of its retrospective nature and is therefore subject to the limitations inherent in this type of clinical investigation. Patients receiving low-dose nebivolol were at higher risk at baseline with worse hemodynamic parameters and higher Killip class. Although adjustment was made using propensity score analysis for confounding variables, unmeasured factors may still exist and the possible role of unmeasured residual confounding cannot be ruled out. Second, due to the relatively small sample size, this study might have been underpowered for clinical outcomes. Thirdly, specific information on PCI characteristics and dose-related adverse reactions were not available from our registry database. Finally, independent statistical analysis was not performed. Data analysis was undertaken by the first author and reviewed by the co-authors.
In conclusion, the present observational study in patients with acute MI showed that the rates of MACCE for low-dose and usual- to high-dose nebivolol were not significantly different at 12-month follow-up. Further investigation is warranted to determine the optimal nebivolol dosing following acute MI.
Figures and Tables
FIG. 1
Distribution of nebivolol dosing at 12 months stratified by whether the dose was decreased (n=10), remained the same (n=598), or increased (n=17) since hospital discharge.

FIG. 2
IPTW-adjusted cumulative incidence of MACCE at 12 months according to study group. IPTW: inverse probability of treatment weighting, MACCE: major adverse cardiovascular and cerebrovascular events.
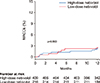
TABLE 1
Baseline clinical characteristics

Values are n (%), mean±SD, or median (interquartile range). ACEI: Angiotensin-converting enzyme inhibitor, ARB: angiotensin receptor blocker, CABG: coronary artery bypass graft surgery, CAD: coronary artery disease, LVEF: left ventricular ejection fraction, MI: myocardial infarction, PCI: percutaneous coronary intervention.
ACKNOWLEDGEMENTS
This research was supported by a fund (2016-ER6304-01) by Research of Korea Centers for Disease Control and Prevention and Elyson Pharmaceutical Co., Ltd., Seoul, Republic of Korea.
References
1. Randomised trial of intravenous atenolol among 16 027 cases of suspected acute myocardial infarction: ISIS-1. First International Study of Infarct Survival Collaborative Group. Lancet. 1986; 2:57–66.

2. Yusuf S, Peto R, Lewis J, Collins R, Sleight P. Beta blockade during and after myocardial infarction: an overview of the randomized trials. Prog Cardiovasc Dis. 1985; 27:335–371.


3. Kernis SJ, Harjai KJ, Stone GW, Grines LL, Boura JA, O'Neill WW, et al. Does beta-blocker therapy improve clinical outcomes of acute myocardial infarction after successful primary angioplasty? J Am Coll Cardiol. 2004; 43:1773–1779.


4. Nakatani D, Sakata Y, Suna S, Usami M, Matsumoto S, Shimizu M, et al. Osaka Acute Coronary Insufficiency Study (OACIS) Investigators. Impact of beta blockade therapy on long-term mortality after ST-segment elevation acute myocardial infarction in the percutaneous coronary intervention era. Am J Cardiol. 2013; 111:457–464.


5. Ozasa N, Kimura T, Morimoto T, Hou H, Tamura T, Shizuta S, et al. j-Cypher Registry Investigators. Lack of effect of oral beta-blocker therapy at discharge on long-term clinical outcomes of ST-segment elevation acute myocardial infarction after primary percutaneous coronary intervention. Am J Cardiol. 2010; 106:1225–1233.


6. Yang JH, Hahn JY, Song YB, Choi SH, Choi JH, Lee SH, et al. Association of beta-blocker therapy at discharge with clinical outcomes in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. JACC Cardiovasc Interv. 2014; 7:592–601.


7. Goldberger JJ, Bonow RO, Cuffe M, Liu L, Rosenberg Y, Shah PK, et al. OBTAIN Investigators. Effect of beta-blocker dose on survival after acute myocardial infarction. J Am Coll Cardiol. 2015; 66:1431–1441.



8. Hwang D, Lee JM, Kim HK, Choi KH, Rhee TM, Park J, et al. KAMIR Investigators. Prognostic impact of β-blocker dose after acute myocardial infarction. Circ J. 2019; 83:410–417.


9. Allen JE, Knight S, McCubrey RO, Bair T, Muhlestein JB, Goldberger JJ, et al. β-blocker dosage and outcomes after acute coronary syndrome. Am Heart J. 2017; 184:26–36.

10. DiNicolantonio JJ, Fares H, Niazi AK, Chatterjee S, D'Ascenzo F, Cerrato E, et al. β-blockers in hypertension, diabetes, heart failure and acute myocardial infarction: a review of the literature. Open Heart. 2015; 2:e000230.

11. Ripley TL, Saseen JJ. β-blockers: a review of their pharmacological and physiological diversity in hypertension. Ann Pharmacother. 2014; 48:723–733.

12. Mrdovic IB, Savic LZ, Perunicic JP, Asanin MR, Lasica RM, Jelena MM, et al. Randomized active-controlled study comparing effects of treatment with carvedilol versus metoprolol in patients with left ventricular dysfunction after acute myocardial infarction. Am Heart J. 2007; 154:116–122.


13. Weiss R. Nebivolol: a novel beta-blocker with nitric oxide-induced vasodilatation. Vasc Health Risk Manag. 2006; 2:303–308.



14. Münzel T, Gori T. Nebivolol: the somewhat-different beta-adrenergic receptor blocker. J Am Coll Cardiol. 2009; 54:1491–1499.

15. Chung J, Han JK, Kim YJ, Kim CJ, Ahn Y, Chan Cho M, et al. investigators for Korea Acute Myocardial Infarction Registry (KAMIR). Benefit of vasodilating β-blockers in patients with acute myocardial infarction after percutaneous coronary intervention: nationwide multicenter cohort study. J Am Heart Assoc. 2017; 6:e007063.

16. Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. ESC Scientific Document Group. Fourth universal definition of myocardial infarction (2018). Eur Heart J. 2019; 40:237–269.

17. Flather MD, Shibata MC, Coats AJ, Van Veldhuisen DJ, Parkhomenko A, Borbola J, et al. SENIORS Investigators. Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS). Eur Heart J. 2005; 26:215–225.


18. O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013; 61:e78–e140.
19. Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2014; 64:e139–e228.
20. Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, et al. PLATO Investigators. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009; 361:1045–1057.


21. Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015; 34:3661–3679.



22. Lunceford JK, Davidian M. Stratification and weighting via the propensity score in estimation of causal treatment effects: a comparative study. Stat Med. 2004; 23:2937–2960.


23. Cole SR, Hernán MA. Constructing inverse probability weights for marginal structural models. Am J Epidemiol. 2008; 168:656–664.



24. Austin PC. The use of propensity score methods with survival or time-to-event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med. 2014; 33:1242–1258.


25. Norwegian Multicenter Study Group. Timolol-induced reduction in mortality and reinfarction in patients surviving acute myocardial infarction. N Engl J Med. 1981; 304:801–807.

26. Hjalmarson A, Herlitz J, Holmberg S, Rydén L, Swedberg K, Vedin A, et al. The Göteborg metoprolol trial. Effects on mortality and morbidity in acute myocardial infarction. Circulation. 1983; 67(6 Pt 2):I26–I32.
27. Chadda K, Goldstein S, Byington R, Curb JD. Effect of propranolol after acute myocardial infarction in patients with congestive heart failure. Circulation. 1986; 73:503–510.


28. Metoprolol in acute myocardial infarction (MIAMI). A randomized placebo-controlled international trial. The MIAMI Trial Research Group. Eur Heart J. 1985; 6:199–226.

29. Sorrentino SA, Doerries C, Manes C, Speer T, Dessy C, Lobysheva I, et al. Nebivolol exerts beneficial effects on endothelial function, early endothelial progenitor cells, myocardial neovascularization, and left ventricular dysfunction early after myocardial infarction beyond conventional β1-blockade. J Am Coll Cardiol. 2011; 57:601–611.






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download