Dear Editor,
To our knowledge, there has been no report of limbic encephalitis (LE) caused by rhematoid arthritis (RA).1 Herein, we describe a patient with concurrent LE and RA.
A 79-year-old, previously healthy, elementary school dropout woman presented to the hospital with the complaint of short-term memory impairment for the past 20 days. On examination, she was alert with relatively good cognitive function. Both proximal interphalangeal (PIP) joints, and both knee joints were swollen and tender. There were no other focal neurologic deficits or signs of infection.
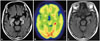
On neuropsychologic examination, she scored 26/30 on Korean-Mini Mental Status Examination; and on Seoul Verbal Learning Test, she remembered 2, 1, 3 words of 12 on immediate recall and none on delayed recall. Other test items on Seoul Neuropsychologic Screening Battery were normal. The levels of complete blood counts, electrolytes, renal indices, liver enzymes and thyroid hormones were within the normal ranges. Cerebrospinal fluid (CSF) examination was normal. Polymerase chain reaction for Herpes Simplex Virus and Varicella Zoster Virus were negative. Electroencephalography findings were normal. Fluid-attenuated inversion recovery imaging of the brain revealed high signal intensity lesions on bilateral medial temporal lobes (Fig. 1A). 18 fluoro-deoxy-glucose positron emission tomography showed accentuated hypermetabolism in left medial temporal lobe indicating LE (Fig. 1B).
An extensive search for underlying systemic autoimmune disease and paraneoplastic disorder were implemented. Laboratory blood tests showed an elevated C-reactive protein (CRP) level (23.52 mg/dL), erythrocyte sedimentation rate (ESR) (78 mm/hr) and RA factor (182.00 IU/mL). Anti-cyclic citrullinated peptide antibody (anti-CCP), anti-beta 2 GP1 IgG and anti-beta 2 GP1 IgM were positive. Both serum and CSF tests for Anti-Hu, Anti-Yo, Anti-Ri, CV2/CRMP5, NMDAR, AMPA1, AMPA2, LG1, GABA-B, and Caspr2 antibodies were negative. Neoplastic serum markers (carcinoembryonic antigen, alpha-feto protein, CA125, CA19-9) were negative. A chest and abdominal CT scan showed no signs of malignancy.
We made a diagnosis of non-paraneoplastic LE without detectable antineuronal antibodies. Also, clinical feature of swollen PIP and knee joints with abnormal acute-reactants (CRP and ESR) and positive serology (RF and anti-CCP) was consistent with RA. She was treated with a course of high dose steroids. Her memory impairment was improved after 10 days. Two weeks later, a follow-up brain MRI demonstrated the disappearance of high signal intensities in bilateral medial temporal lobes (Fig. 1C). For RA, she was prescribed 7.5 mg/week of methotrexate, 1 mg/day of folic acid and 400 mg/day of hydroxychloroquine.
Herein, we described a patient with non-paraneoplastic LE accompanied by RA. Reports of LE combined with various connective tissue diseases are rare. We only found some reports on LE combined with Sjogren's syndrome, and LE following immunotherapy for RA.234 It is possible that the immunologic mechanism of RA contributed to the pathogenesis of LE in our patient. However, associated biological mechanism between RA and LE remains unclear. Additional reports of similar cases will clarify the link between the two diseases.
Figures and Tables
Fig. 1
Radiologic findings of the patient. Fluid-attenuated inversion recovery image (A) shows high signal intensity lesions on bilateral medial temporal lobes. 18 fluoro-deoxyglucose positron emission tomography image (B) shows accentuated hypermetabolism in left medial temporal lobe. Follow-up fluid-attenuated inversion recovery image after two weeks of admission (C) demonstrates the disappearance of high signal intensities in bilateral medial temporal lobes.
References
1. Bougea A, Anagnostou E, Konstantinos G, George P, Triantafyllou N, Kararizou E. A Systematic Review of Peripheral and Central Nervous System Involvement of Rheumatoid Arthritis, Systemic Lupus Erythematosus, Primary Sjögren's Syndrome, and Associated Immunological Profiles. Int J Chronic Dis. 2015; 2015:910352.

2. Collison K, Rees J. Asymmetric cerebellar ataxia and limbic encephalitis as a presenting feature of primary Sjögren's syndrome. J Neurol. 2007; 254:1609–1611.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download