TO THE EDITOR: The incidence of entrapment neuropathy after a trauma in individuals with hemophilia is rare. Herein, we present a young man with severe hemophilia A who developed acute carpal tunnel syndrome (CTS) after a fall. He was managed conservatively with factor replacement, and a significant improvement was observed within 1 week. This result indicates that prompt conservative management can help to prevent surgery in such cases.
The most common type of nerve damage in individuals with hemophilia is peripheral neuropathy, which mainly affects the upper and lower limbs [1]. Approximately 1.7–13.6% of patients with hemophilia present with peripheral nerve lesions [2]. In most cases, only one nerve is involved, and the simultaneous involvement of multiple nerves, e.g., the median and ulnar nerves, is rare. The most common cause of compartment syndrome is hemorrhage in the calf and anterior forearm [3]. A recent systematic review has shown that 21% of patients with acute compartment syndrome in the thigh had coagulation defects [34]. In these cases, achieving hemostasis is significantly more important than a fasciotomy [3]. CTS, which is a condition caused by median nerve entrapment, can occur in individuals with early compartment syndrome. To date, the incidence of CTS in individuals with hemophilia is low [5].
A 19-year-old man presented with prolonged bleeding after a trivial trauma since childhood. The patient was subsequently diagnosed with severe hemophilia A (FVIII level <1%) at the age of 3 years. He presented with recurrent bleeding in the joints primarily involving the knees. The left knee is the target joint. He received fresh frozen plasma transfusions or factor VIII on an on demand basis. Currently, due to the absence of inhibitors, he presented with pain and swelling of the anterior aspect of left forearm and inability to extend his fingers after falling on an outstretched hand 1 week back.
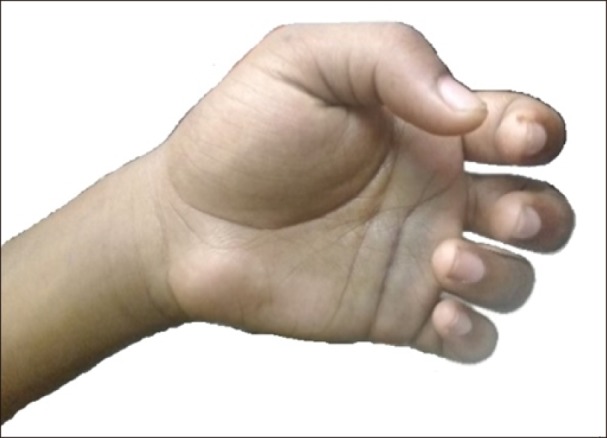
Upon examination, the swelling extended from the left elbow to the left hand with clawing of all fingers (Fig. 1). The palm was bluish in appearance. However, peripheral pulses were palpable. Sensory loss in the distribution of the ulnar and median nerves and tenderness on the flexor aspect of the wrist and forearm with pain on passive extension of the fingers were noted. Phalen's test was positive.
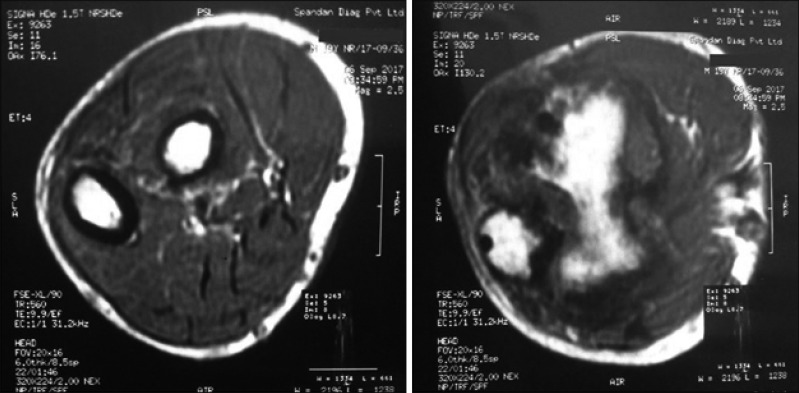
The radiograph images did not reveal any fractures. However, magnetic resonance imaging showed the presence of intra-articular collection in the wrist and neurovascular plane (Fig. 2). Thus, the administration of recombinant factor VIII twice daily was initiated (with a target of 50% correction). The opinion of an orthopedic surgeon was obtained, and conservative management was continued. On the second day of admission, there was no further worsening of the signs and symptoms. He was assessed daily within the first 10 days and weekly thereafter on a regular basis until 4 weeks. After 1 week, the swelling subsided by almost 60%. His pain reduced with transcutaneous electrical nerve stimulation (TENS), and finger extension also improved. Factor replacement via recombinant factor VIII injections twice daily was continued for 1 week. Within 2 weeks, further improvement in finger extension and diminution of swelling were observed. On the third week, the swelling almost subsided, and he can extend his fingers to almost full extent.
Active physiotherapy was started after 3 days of acute bleeding. A significant clinical improvement was observed, and movement of the small joints in the hand improved. Then, further improvements were continuously observed. He was on regular follow-up, and no residual neurological deficit was noted after 4 weeks (Fig. 3).
Acute compartment syndrome is characterized by increased pressure within a confined compartment beyond a critical level, causing a decline in the perfusion pressure to the tissues resulting in microvascular impairment. The tissues within a compartment can become ischemic due to a reduced perfusion pressure gradient below the critical level, and this may result in necrosis. Moreover, ischemic necrosis of the nerve(s) in that compartment may be observed.
In the present case, the patient sustained a fall on the outstretched hand and developed swelling from the elbow up to the left hand. Soft tissue swelling and involvement of both the ulnar and median nerves were simultaneously observed at different sites, suggesting compartment syndrome. With conservative management only, a significant clinical improvement was observed after 1 week and almost a complete resolution after 3 weeks. In our case, continuous effort to achieve an effective hemostasis led to a significant result.
In 2002, Kaymak et al. [2] have reported a similar case in which a boy with hemophilia had a minor ulnar and significant median nerve involvement due to compartment syndrome. In another study by Katz et al. [6], approximately 3.4% of admitted patients diagnosed with hemophilia presented with coexisting median and ulnar nerve compression.
Therefore, in any patient, proper history taking and physical examination are of utmost importance. During physical examination, motor and sensory loss, deep tendon reflexes, range of motion, muscle function, and peripheral pulses must be cautiously examined. The golden rule of Protection, Rest, Ice, Compression, and Elevation is as important as factor replacement. If a patient is relieved of pain (subsidence of the acute stage), physiotherapy can be started. Thus, in several cases, surgical decompression can be prevented.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download