Abstract
Backgrounds/Aims
Hepatic hemangioma is a common non-epithelial neoplasm of the liver. Presence of symptoms and uncertainty in diagnosis are the most common indications for surgery.
Methods
Eighteen patients with hepatic hemangioma, operated on from January 2011 to December 2016 at the Hepato-pancreato-biliary surgical unit of Tata Memorial Hospital, were retrospectively analyzed.
Results
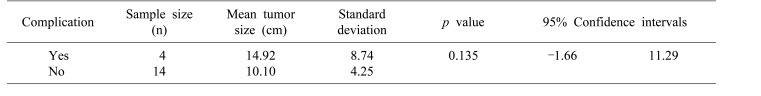
Main indications for operation were presence of symptoms, the most common being pain and diagnostic uncertainty. The median size of hemangioma was 9.9 cm (range 3.2 to 24 cm). All patients underwent extra-capsular excision of hemangioma. The median operating time was 180 minutes (range 75 to 460 minutes) and median blood loss was 950 ml (range 100 to 3,500 ml). Median post-operative stay was 5.5 days (range 3 to 10 days). One (5.6%) patient required re-exploration for post-operative hemorrhage, Clavien Dindo (CD) grade IIIb, and one (5.6%) had postoperative purulent intra-abdominal collection requiring percutaneous cutaneous drainage CD grade IIIa. There was no postoperative mortality. Postoperative day 3 liver function tests were within normal limits. Size of the tumor did not correlate significantly with postoperative complications (p=0.135).
Conclusions
Surgical treatment of hemangioma should be guided by presence of symptoms or by the presence of diagnostic uncertainty, not by size alone. The size had no correlation with perioperative complications. The technique of extra-capsular excision is safe and technically feasible in most of the hemangiomas. This technique preserves maximum liver parenchyma, resulting in early postoperative recovery with minimal morbidity.
Hepatic hemangioma is a common non-epithelial neoplasm of the liver with a wide range of incidence, ranging from 1% to, 20%.1 It is usually asymptomatic and incidentally detected but prompts a flurry of investigations and lot of anxiety for the patient, because metastasis is the most common differential diagnosis.2 Though current recommendations are in favor of observation, even for large hemangiomas, the diagnostic dilemma leading to anxiety, coupled with symptomatology (related to pressure/capsular stretch), leads to consideration of surgery for these neoplasms. The surgical procedure of choice, whether enucleation or liver resection, is still debatable. Major hemodynamic changes can occur during surgery, especially massive blood loss. Postoperative complications, including bile leaks, have been reported to occur more frequently with liver resections than with enucleation.34
We analyzed eighteen patients with hepatic hemangioma who were operated on from January 2011 to December 2016 at the Hepato-pancreato-biliary surgical unit of Tata Memorial Hospital. Preoperative demographic parameters, imaging findings, and indication for surgery were recorded. A detailed record of intraoperative parameters, such as operative time, intra-operative blood loss, and blood transfusions required, was maintained. Post-operative parameters, such as liver function tests on post-operative days 1, 3, and 7 (or earlier if clinically indicated) and postoperative hospital stay was noted. Postoperative complications were classified according to the Clavien Dindo (CD) grades.8 A survey of patient symptoms after operation was done by telephone 3 months after the date of surgery.
Data collection and statistical analysis were done using SPSS (ver. 21.0) and a Mann-Whitney test for continuous variables. A p value <0.05 was considered to be statistically significant. Spearman coefficient (rho) was used to correlate the size of the lesion with various intraopertaive and postoperative parameters to assess their bearing on surgical outcomes.
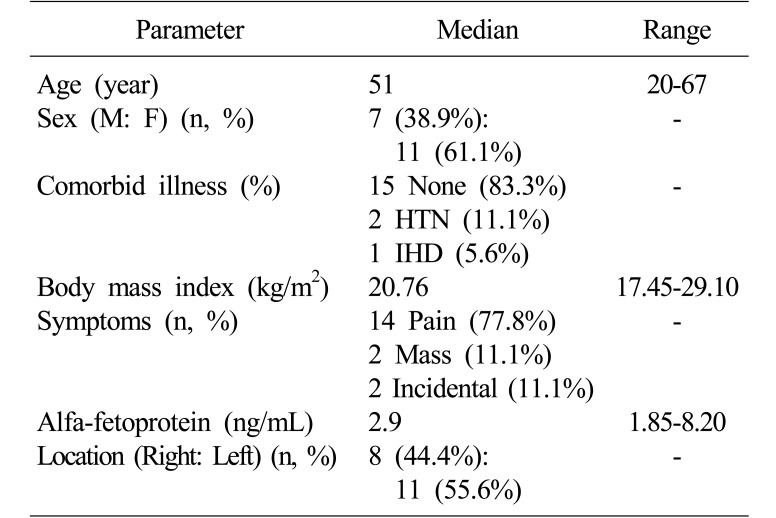
Of the 440 liver resections performed at Tata Memorial Hospital in the study period, 18 were done for suspected hemangiomas (4.09%). Basic demographic and clinical profiles of the patients are elaborated in Table 1. None of the patients had a background of cirrhosis on biochemical or radiological evaluation. All patients had a normal hematological evaluation, with no evidence of consumptive coagulopathy.
Six out of 18 (33.3%) patients had atypical imaging characteristics that led to diagnostic uncertainty. Of these 6 patients, 3 (16.7%) underwent a preoperative biopsy, 2 (11.1%) of which were inconclusive, whereas 1 (5.6%) was suggestive of hemangioma.
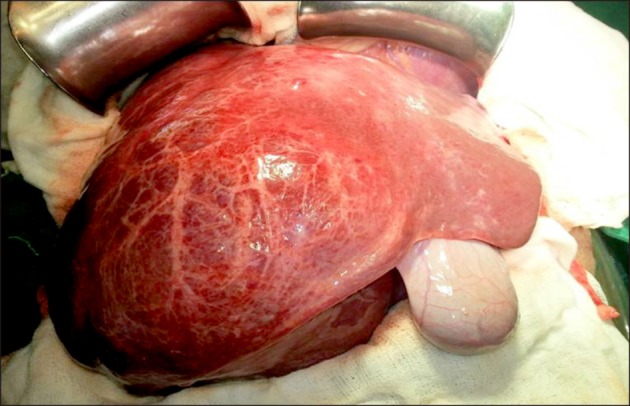
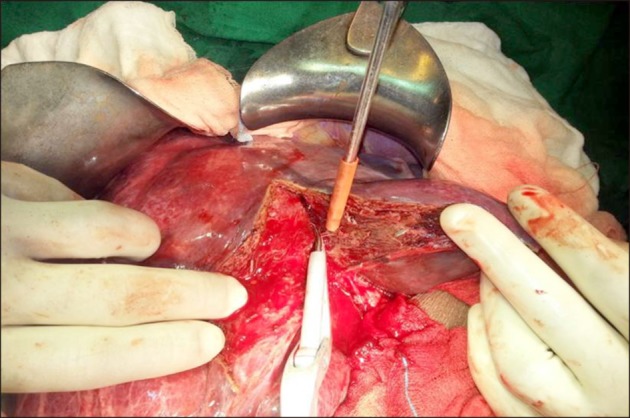
All patients underwent extra-capsular excision of the tumor (Figs. 1, 2). The median operating time was 180 minutes, (range 75 to 460 minutes). Median blood loss was 950 ml (range 100 to 3,500 ml). Six (33.3%) patients required intra-operative transfusion. Median post-operative stay was 5.5 days (range 3 to 10 days).
Fourteen (77.8%) had no post-operative complications. The major complications included one (5.6%) patient who required re-exploration for postoperative hemorrhage (CD grade IIIb) and one (5.6%) who had postoperative purulent intra-abdominal collection requiring per-cutaneous drainage (CD grade IIIa). There was no post-operative mortality. Postoperative day-3 liver function tests were within normal limits.
Histopathological evaluation of all 18 patients showed presence of cavernous hemangioma. Fifteen patients (83.3%) had a single lesion, whereas 3 (16.6%) had >1 lesions. Median size of hemangiomas was 9.9 cm (range 3.2 to 24 cm). Sizes of tumor and outcomes are shown in Table 2 and 3.
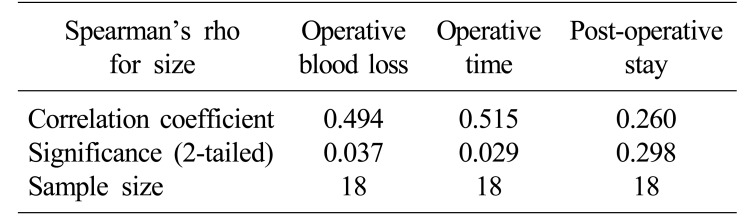
On correlating the size of the tumor with the duration of surgery, operative blood loss, and postoperative stay, the Spearman coefficient was found to be 0.515, 0.494, and 0.260 respectively; duration of surgery and operative blood loss showed significant correlation (p<0.05), indicating that the size of the hemangioma affected intraoperative parameters. The size of the tumor did no correlate significantly with postoperative complications (p=0.135; 95% CI=−1.66 to 11.29)
Hepatic hemangioma accounts for almost 75% of benign liver tumors, with a frequency of 0.4%to 7.3% at autopsy.9 These tumors are more commonly found in women, with a female: male ratio of up to 5:1.10 A female predisposition was seen in our experience (female: male ratio of 1.57:1), though not to the same extent.
Most authors label the hemangioma ‘giant’ if it is more than 10 cm.561112 However, it has been proved in multiple studies that size has no direct correlation with the extent of pain, and small lesions can also continue to have severe pain.3 A study by Etemadi et al.3 reported that 58% of the patients had abdominal pain at presentation, and in 50% of cases this pain was the reason for referral, which led to the diagnosis of liver hemangioma. However, in only 12.6% of the cases could the pain be attributed to the hemangioma. Pain most commonly results from the tumor stretching the liver capsule or compressing adjacent organs. Rarely has it been reported to be caused by infarction and necrosis of the tumor. In our series of 18 hemangiomas undergoing surgical resection, we found that 88.9% of patients were symptomatic with abdominal pain or mass per abdomen.
Uncommon complications of hemangioma include spontaneous rupture and malignant transformation, both of which are very rare.3 Until now, less than 50 cases of spontaneous rupture have been reported, and malignant transformation is practically nonexistent.
The ideal indication for surgery remains strictly related to symptoms and complications. The size of the tumor alone doesn't justify treatment. Yoon et al.7 evaluated 115 patients and found that the most common indication for surgery was the presence of symptoms (60%), with the other 40% being increasing size, large size, and uncertainty in diagnosis. In our study, 6 (33.3%) patients had atypical imaging characteristics, leading to diagnostic uncertainty; hence a surgical resection was considered for these patients.
Liver resection and enucleation are the two most common modalities of surgical management and have been the subject of multiple studies. Zimmermann and Baer4 described the well-formed tumor-liver interface and its surgical application. The space between the liver and the hemangioma is avascular, consisting of only liver tissue compressed by the growing hemangioma. No bile ducts and only a few blood vessels traverse the capsule, and these are easily controlled. By identifying this layer between the capsule of the hemangioma and the liver, one can remove the tumor with minimal risk of bleeding and postoperative bile leak. The amount of normal-functioning liver parenchyma removed is also minimal. This is, however, not possible for formal liver resections, because it entails transecting through the normal liver, with chances of increased blood loss and higher incidence of post-operative bile leaks. Singh et al.13 have found lesser blood loss with enucleation than with resections (400 ml vs. 1,300 ml) and shorter hospital stay (5 vs. 10 days). Resection remains the choice for multiple hemangiomas of the liver and for deep-seated hemangiomas where enucleation is not possible. In our study, all 18 patients underwent surgical excision of hemangioma by extra-capsular excision. It is safe and technically feasible in superficial as well as in large tumors with deep parenchymal extension. Excision of the hemangioma in the extra-capsular avascular plane minimizes the bleeding and bile leak. This procedure also allows excision of large hemangiomas without any parenchymal loss, post-operative liver functions are well preserved, and complications are minimized.
In our study, we also found that the larger is the tumor, the longer is the operative time and the greater is operative blood loss. Size of tumor, however, did not have any negative effect on perioperative complications.
The limitation of our study was the small sample size of eighteen patients analyzed retrospectively. However, hemangiomas are rarely treated by surgery; hence this analysis throws light on important parameters that guide decisions in management of these tumors, as well as on the technique of extra-capsular excision, which is a safe and effective approach that preserves maximal liver parenchyma with resultant early post-operative recovery.
In conclusion, surgical treatment of hemangiomas should be guided by the presence of symptoms or of diagnostic uncertainty, not by size alone. The size had no correlation with perioperative complications. The technique of extra-capsular excision is safe and technically feasible for most of the hemangiomas. This technique preserves maximal liver parenchyma, resulting in early post-operative recovery with minimal morbidity.
References
1. Semelka RC, Sofka CM. Hepatic hemangiomas. Magn Reson Imaging Clin N Am. 1997; 5:241–253. PMID: 9113674.

3. Etemadi A, Golozar A, Ghassabian A, Zarei M, Hashemi Taheri AP, Dawsey SM, et al. Cavernous hemangioma of the liver: factors affecting disease progression in general hepatology practice. Eur J Gastroenterol Hepatol. 2011; 23:354–358. PMID: 21383624.
4. Zimmermann A, Baer HU. Fibrous tumor-liver interface in large hepatic neoplasms: its significance for tumor resection and enucleation. Liver Transpl Surg. 1996; 2:192–199. PMID: 9346648.

5. van Tilborg AA, Nielsen K, Scheffer HJ, van den Tol P, van Waesberghe JH, Sietses C, et al. Bipolar radiofrequency ablation for symptomatic giant (>10 cm) hepatic cavernous haemangiomas: initial clinical experience. Clin Radiol. 2013; 68:e9–e14. PMID: 23146554.
6. Toro A, Mahfouz AE, Ardiri A, Malaguarnera M, Malaguarnera G, Loria F, et al. What is changing in indications and treatment of hepatic hemangiomas. A review. Ann Hepatol. 2014; 13:327–339.

7. Yoon SS, Charny CK, Fong Y, Jarnagin WR, Schwartz LH, Blumgart LH, et al. Diagnosis, management, and outcomes of 115 patients with hepatic hemangioma. J Am Coll Surg. 2003; 197:392–402. PMID: 12946794.

8. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213. PMID: 15273542.
9. Ishak KG, Rabin L. Benign tumors of the liver. Med Clin North Am. 1975; 59:995–1013. PMID: 167242.

10. Reddy KR, Kligerman S, Levi J, Livingstone A, Molina E, Franceschi D, et al. Benign and solid tumors of the liver: relationship to sex, age, size of tumors, and outcome. Am Surg. 2001; 67:173–178. PMID: 11243545.
11. Adam YG, Huvos AG, Fortner JG. Giant hemangiomas of the liver. Ann Surg. 1970; 172:239–245. PMID: 5433290.

12. Grieco MB, Miscall BG. Giant hemangiomas of the liver. Surg Gynecol Obstet. 1978; 147:783–787. PMID: 362577.
13. Singh RK, Kapoor S, Sahni P, Chattopadhyay TK. Giant haemangioma of the liver: is enucleation better than resection? Ann R Coll Surg Engl. 2007; 89:490–493. PMID: 17688721.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download