Abstract
Purpose
Although adjuvant chemotherapy reduces the risk of disease recurrence in stage III colon cancer patients, published guidelines do not specify when it should be initiated. This study aimed to assess the effect of adjuvant chemotherapy initiation time on disease recurrence and survival in stage III colon cancer patients undergoing curative surgical resection.
Methods
The medical records of stage III colon cancer patients undergoing curative resection between February 2004 and December 2009 were reviewed.
Results
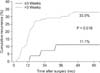
Of the 133 enrolled patients, 27 (20.3%) began adjuvant chemotherapy within 3 weeks of surgery, whereas 106 (79.7%) did after 3 weeks following surgery. Patients receiving chemotherapy within 3 weeks of surgery were less likely to experience recurrences than those beginning treatment later (11.1% vs. 33%, P = 0.018). The mean disease-free survival of patients receiving adjuvant therapy earlier was 54.6 months, whereas that of patients with later treatment was 43.5 months (P = 0.014). However, no significant differences in overall survival were observed between the 2 groups.
Surgical resection is the primary treatment in the clinical management of stage III colon cancer, but given the high risk of recurrence, adjuvant chemotherapy has become part of the standard of care. Adjuvant chemotherapy has been shown to offer a risk reduction of 33% and 40% in mortality and disease recurrence, respectively, compared to surgery alone [1]. In particular, it reportedly benefits patients with curatively resected stage III colon cancer in terms of their tumor relapse and overall survival [23].
Adjuvant chemotherapy may ideally be initiated shortly after recovery from surgery, but its optimal timing remains debatable. The interval between resection and chemotherapy may provide opportunities for micrometastases to proliferate. However, delay in adjuvant chemotherapy initiation might be inevitable owing to patients' health factors or surgical complications [456789]. Published guidelines do not explicitly specify a time interval within which adjuvant chemotherapy should be initiated. The European Society for Medical Oncology guideline does not describe the time interval between resection and chemotherapy [10]. National Comprehensive Cancer Network guideline only shows both a meta-analysis advocating early initiation of the adjuvant chemotherapy and criticisms about the analysis, instead of specifying the timing of adjuvant chemotherapy [11]. Therefore, this study aimed to assess the effect adjuvant chemotherapy timing on disease recurrence and survival in patients with stage III colon cancer who underwent curative surgical resection.
Between February 2004 and December 2009, 172 patients underwent curative resection for stage III colon cancer. Disease staging was based on the American Joint Committee on Cancer (AJCC) Cancer Staging Manual (7th edition) [12]. Thirty-nine patients who did not receive adjuvant chemotherapy owing to fear of chemotherapy-related side effects, poor general condition, or multiple comorbidities were excluded. Thus, this study enrolled a total of 133 patients. Adjuvant chemotherapy was initiated when a patient recovered completely from surgery. Chemotherapy regimens were selected according to patient preference of oral versus intravenous administration, comorbidities, and expected drug toxicities.
The enrolled patients were divided into 2 groups: those receiving chemotherapy within 3 weeks of surgery (group A) and those who after 3 weeks following surgery (group B). The patients usually stayed in our hospital for about 7 days after colon cancer surgery. The first postoperative check-up was scheduled in 1 week after discharge. If the patient's condition was suitable for receiving chemotherapy, chemotherapy was initiated within 1 week following the postoperative check-up. The shortest time interval between resection and chemotherapy was 3 weeks in our hospital. Hence, we divided the patients into 2 groups based on a 3-week period.
Patient data were collected retrospectively from electronic medical records, including patient demographics, cancer characteristics, treatment, and survival. We obtained survival data of the patients from Division of Cancer Registration & Surveillance, National Cancer Control Institute of Korea.
The 2 groups were compared with respect to patient demographics, surgery, and oncologic outcomes including cancer recurrence, disease-free survival, and overall survival.
Demographic data and clinicopathological results were evaluated using the Pearson chi-square test and Student t-test. The Kaplan-Meier method was used to analyze survival. Differences in survival between groups were compared using the log-rank test. A P-value of less than 0.05 was considered statistically significant. Data were analyzed using the PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA).
The mean age of all enrolled patients was 65.8 years (range, 37-87 years). There were more women (71, 53.4%) than men in the cohort. Sigmoid colon was the most common cancer location (77, 57.9%), followed by ascending colon (38, 28.6%). Anterior resection was the most commonly performed surgery (73, 54.1%), followed by right hemicolectomy (46, 34.6%). The AJCC T classification was T1 (2, 1.5%), T2 (10, 7.5%), T3 (110, 82.7%), or T4 (11, 8.3%), whereas the N classification was N1a (42, 31.6%), N1b (40, 30.1%), N2a (23, 17.3%), or N2b (28, 21.1%). Patient demographic and clinicopathologic characteristics are summarized in Table 1.
Of the 133 patients, 27 (20.3%) began adjuvant chemotherapy within 3 weeks of surgery (group A; median, 18 days; range, 13-21 days) and 106 (79.7%) did after 3 weeks following surgery (group B; median, 30 days; range, 22-76 days).
No statistically significant differences in age, sex, American Society of Anesthesiologists score, tumor location, surgery, T stage, N stage, AJCC stage, tumor differentiation, lymphovascular invasion, and adjuvant chemotherapy regimen were observed between the 2 groups.
Additionally, no dose reduction or chemotherapy cessation owing to adverse effects of chemotherapy on intestinal anastomosis or surgical wound was required in either group.
During a median follow-up period of 27 months (range, 4-76 months), group A patients (3/27, 11.1%) were less likely to experience disease recurrence than those in group B (35/106, 33%; P = 0.018) (Fig. 1). Systemic recurrence occurred in 3 patients in group A and in 32 patients in group B. Local recurrence occurred in 3 patients in group B (Table 2).
The Kaplan-Meier method was employed to compare diseasefree survival rates. Multivariate analysis was performed using the Cox proportional hazards model. In univariate analysis (Table 3), potential factors for disease-free survival included N stage and chemotherapy timing. By multivariate analysis (Table 4), the most important independent factors affecting diseasefree survival were chemotherapy timing (95% confidence interval, 1.103-11.740; hazard ratio, 3.598) followed by N stage (95% confidence interval, 1.579-5.861; hazard ratio, 3.042).
The time interval between resection and chemotherapy may provide a window of opportunities for micrometastases to proliferate. Studies in animal models suggest that surgery may increase the number of circulating tumor cells and potentiate the growth of metastatic deposits. Such an increase in metastatic growth is thought to correlate with a reduction in angiogenesis inhibitors, such as angiostatin, following removal of the primary tumor [13141516]. Surgery has also been shown to enhance production of oncogenic growth factors, such as transforming growth factor alpha, which could escalate tumor growth. Furthermore, a classic mathematical model predicted that the probability of mutations leading to drug resistance increased over time, dependent on mutation rate and tumor size [17].
Published guidelines have not explicitly specified a time interval within which adjuvant chemotherapy should be initiated. A previous study suggested a reduced rate of cancer recurrence if patients with stage III colon cancer received adjuvant chemotherapy within 27 days after curative resection [18]. Chau et al. [19] found a significant survival advantage for patients whose adjuvant chemotherapy was initiated within eight weeks after curative resection of stages II and III colorectal cancer. Glimelius et al. [20] reported in a study of patients with stage III colon cancer that adjuvant chemotherapy initiated more than 8 weeks after surgery conferred worse survival than when administration was started within 8 weeks. A systematic review and meta-analysis demonstrated that a 4-week delay of adjuvant chemotherapy was associated with a 14% decrease in both overall and disease-free survival [21]. These studies indicated that early initiation of adjuvant chemotherapy could result in better survival. In present study, patients who received adjuvant chemotherapy within 3 weeks after resection of colon cancer also had better disease-free survival, which was consistent with previously published results.
Despite oncologic benefits of early adjuvant chemotherapy initiation, treatment is usually delayed for several weeks. One of the major reasons for such a delay is the risk of anastomotic leakage due to the unfavorable effects of chemotherapeutic agents on normal healing process. The proliferative phase of the wound healing process occurs approximately from day 4 through 12 after tissue injury to re-establish tissue continuity. In this phase, collagen is synthesized by smooth muscle cells and fibroblasts in the submucosal layer and lysed by collagenase activity. As collagen lysis contributes to low anastomotic strength, the risk for anastomotic leakage is high during the first 3 to 10 days after intestinal anastomosis [22]. Perioperative chemotherapy may result in further wound healing delay and consequently compromise anastomotic integrity and increase the risk of anastomotic leakage [23]. In an animal study, perioperative administration of capecitabine did not exert a negative impact on colonic anastomosis [24]. In contrast, another study reported that early postoperative 5-fluorouracil administration had a negative impact on the bursting strength of colonic anastomosis [25]. In this study, there was no wound dehiscence or anastomotic leakage caused by adjuvant chemotherapy, even in patients receiving chemotherapy within 3 weeks following surgery. Additionally, no dose reduction or chemotherapy cessation due to adverse effects of chemotherapy on intestinal anastomosis or surgical wound was required in either the early or late initiation group.
Slow recovery from surgery may result in delayed initiation of adjuvant chemotherapy. Patients with later adjuvant chemotherapy initiation are expected to experience more comorbidities than those with early treatment. In this study, the early initiation group showed better disease-free survival rate than the late group. However, no significant differences in overall survival were observed between the 2 groups. Although early initiation of adjuvant chemotherapy might offer an oncologic benefit, starting of chemotherapy should only be considered when a patient completely recovers from surgery.
The patients usually stayed in our hospital for about seven days after colon cancer surgery, unless there were severe postoperative complications. One week after discharge, the patients visited outpatient clinics for a postoperative check-up. If the patient's condition was suitable for receiving chemotherapy, chemotherapy was initiated within one week following the first postoperative check-up. The patients with good postoperative health status could start adjuvant chemotherapy within 3 weeks after surgery in our hospital. If the patient's condition is amenable to receive adjuvant chemotherapy, initiation of chemotherapy in the immediate postoperative period after surgery may be possible. However, only 2 patients received chemotherapy within 2 weeks of surgery in present study. Each patient started chemotherapy on 13th and 14th day after surgery. That is the reason why we divided the patients into 2 groups based on a 3-week period.
We, also, evaluated disease free and overall survival rate according to other chemotherapy initiation time periods (4-week and an 8-week periods).
The mean disease-free survival of patients receiving adjuvant therapy within 4 weeks was 50.7 months, whereas that of patients receiving after four weeks was 41.1 months (P = 0.030). However, no statistically significant differences in overall survival were observed between the 2 groups (58.6 months vs. 70.1 months, P = 0.885). When the patients were divided into 2 groups based on eight weeks, disease-free and overall survival were different significantly between 2 groups (48.2 months vs. 26.8 months, P = 0.011; 68.3 months vs. 58.2 months, P = 0.046, respectively). Overall survival was significantly different only when dividing patients based on an 8-week period. Diseasefree survival, however, was significantly shorter in all early chemotherapy initiation groups, irrespective of chemotherapy initiation period. Disease-free survival was getting shorter as a time period of chemotherapy initiation was longer (within 3 weeks, 54.6 months; within four weeks, 50.7 months; within eight weeks, 48.2 months).
In univariate analysis, potential factors for disease-free survival included N stage and chemotherapy timing. In multivariate analysis of prognostic factors for disease-free survival, the most important independent factors were chemotherapy timing followed by N stage.
The recurrence rate of patients receiving adjuvant therapy earlier was significantly lower than that of patients with later treatment. However, no statistically significant differences in overall survival were observed. Most patients with recurrent colon cancer were treated with chemotherapy or surgery, which could lead to the reduction of the difference of oncology conditions between the 2 groups. This might eventually result in comparable rates of overall survival between the 2 groups.
To the best of our knowledge, this is the first study to investigate the association between adjuvant chemotherapy initiation (within 3 weeks versus more than 3 weeks after surgery) and disease recurrence and survival. However, the study is subject to some limitations. First, it was not a randomized controlled study, which would cause potential selection bias.
Additionally, the sample size (133 patients) of this study was not estimated. Since patients were retrospectively enrolled in this study, sample size estimation could not be performed. The number of patients in group A was relatively small compared to that of group B. These limitations are potential weaknesses of this study.
In conclusion, our findings suggest that adjuvant chemotherapy could be initiated as soon as a patient's clinical condition is amendable to the treatment. Patients with stage III colon cancer may benefit from adjuvant chemotherapy initiation within 3 weeks after surgery. This retrospective study had statistical limitation due to small number of enrolled patients. Further large prospective, multicenter, randomized studies are warranted to confirm the true benefit of early initiation of adjuvant chemotherapy.
Figures and Tables
Fig. 2
Disease-free survival rates of both groups. Group A, patients receiving chemotherapy within 3 weeks of surgery; group B, patients receiving chemotherapy after 3 weeks of surgery.
Fig. 3
Overall survival rates of both groups. Group A, patients receiving chemotherapy within 3 weeks of surgery; group B, patients receiving chemotherapy after 3 weeks of surgery.

Table 1
Comparison of demographic and clinicopathologic characteristics between the 2 groups

Values are presented as mean ± standard deviation or number (%).
Group A, patients receiving chemotherapy within 3 weeks of surgery; group B, patients receiving chemotherapy after 3 weeks of surgery; ASA, American Society of Anesthesiologists; AJCC, American Joint Committee on Cancer; 5-FU, 5-fluorouracil; IV, intravenous; LV, leucovorin; FOLFOX, 5-fluorouracil, leucovorin, and oxaliplatin.
a)Pearson chi-square test. b)Student t-test
References
1. Moertel CG, Fleming TR, Macdonald JS, Haller DG, Laurie JA, Goodman PJ, et al. Levamisole and fluorouracil for adjuvant therapy of resected colon carcinoma. N Engl J Med. 1990; 322:352–358.
2. Wolmark N, Rockette H, Fisher B, Wickerham DL, Redmond C, Fisher ER, et al. The benefit of leucovorin-modulated fluorouracil as postoperative adjuvant therapy for primary colon cancer: results from National Surgical Adjuvant Breast and Bowel Project protocol C-03. J Clin Oncol. 1993; 11:1879–1887.
3. Bleiberg H. Adjuvant therapy in highrisk colon cancer. Semin Oncol. 2000; 27:5 Suppl 10. 48–59.
4. Hershman D, Hall MJ, Wang X, Jacobson JS, McBride R, Grann VR, et al. Timing of adjuvant chemotherapy initiation after surgery for stage III colon cancer. Cancer. 2006; 107:2581–2588.
5. Cree M, Tonita J, Turner D, Nugent Z, Alvi R, Barss R, et al. Comparison of treatment received versus long-standing guidelines for stage III colon and stage II/III rectal cancer patients diagnosed in Alberta, Saskatchewan, and Manitoba in 2004. Clin Colorectal Cancer. 2009; 8:141–145.
6. Winget M, Hossain S, Yasui Y, Scarfe A. Characteristics of patients with stage III colon adenocarcinoma who fail to receive guideline-recommended treatment. Cancer. 2010; 116:4849–4856.
7. Schrag D, Cramer LD, Bach PB, Begg CB. Age and adjuvant chemotherapy use after surgery for stage III colon cancer. J Natl Cancer Inst. 2001; 93:850–857.
8. Jessup JM, Stewart A, Greene FL, Minsky BD. Adjuvant chemotherapy for stage III colon cancer: implications of race/ethnicity, age, and differentiation. JAMA. 2005; 294:2703–2711.
9. Ayanian JZ, Zaslavsky AM, Fuchs CS, Guadagnoli E, Creech CM, Cress RD, et al. Use of adjuvant chemotherapy and radiation therapy for colorectal cancer in a population-based cohort. J Clin Oncol. 2003; 21:1293–1300.
10. Labianca R, Nordlinger B, Beretta GD, Brouquet A, Cervantes A. ESMO Guidelines Working Group. Primary colon cancer: ESMO Clinical Practice Guidelines for diagnosis, adjuvant treatment and followup. Ann Oncol. 2010; 21:Suppl 5. v70–v77.
11. National Comprehensive Cancer Network clinical practice guidelines in oncology (NCCN Guidelines): Colon/rectal cancer. ver. 1. 2010 [Internet]. Fort Wathington: National Comprehensive Cancer Network;c2015. cited 2015 Feb 16. Available from: http://www.nccn.org/professionals/physician_gls/pdf/colon.pdf.
12. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. AJCC cancer staging manual. 7th ed. New York: Springer;2010.
13. McCulloch P, Choy A. Effect of menstrual phase on surgical treatment of breast cancer. Lancet. 1994; 344:402–403.
14. Fidler IJ, Ellis LM. The implications of angiogenesis for the biology and therapy of cancer metastasis. Cell. 1994; 79:185–188.
15. Folkman J. What is the evidence that tumors are angiogenesis dependent? J Natl Cancer Inst. 1990; 82:4–6.
16. Gunduz N, Fisher B, Saffer EA. Effect of surgical removal on the growth and kinetics of residual tumor. Cancer Res. 1979; 39:3861–3865.
17. Goldie JH, Coldman AJ. A mathematic model for relating the drug sensitivity of tumors to their spontaneous mutation rate. Cancer Treat Rep. 1979; 63:1727–1733.
18. Arkenau HT, Bermann A, Rettig K, Strohmeyer G, Porschen R. Arbeitsgemeinschaft Gastrointestinale Onkologie. 5-Fluorouracil plus leucovorin is an effective adjuvant chemotherapy in curatively resected stage III colon cancer: long-term follow-up results of the adjCCA-01 trial. Ann Oncol. 2003; 14:395–399.
19. Chau I, Norman AR, Cunningham D, Tait D, Ross PJ, Iveson T, et al. A randomised comparison between 6 months of bolus fluorouracil/leucovorin and 12 weeks of protracted venous infusion fluorouracil as adjuvant treatment in colorectal cancer. Ann Oncol. 2005; 16:549–557.
20. Glimelius B, Dahl O, Cedermark B, Jakobsen A, Bentzen SM, Starkhammar H, et al. Adjuvant chemotherapy in colorectal cancer: a joint analysis of randomised trials by the Nordic Gastrointestinal Tumour Adjuvant Therapy Group. Acta Oncol. 2005; 44:904–912.
21. Biagi JJ, Raphael MJ, Mackillop WJ, Kong W, King WD, Booth CM. Association between time to initiation of adjuvant chemotherapy and survival in colorectal cancer: a systematic review and metaanalysis. JAMA. 2011; 305:2335–2342.
22. Munireddy S, Kavalukas SL, Barbul A. Intra-abdominal healing: gastrointestinal tract and adhesions. Surg Clin North Am. 2010; 90:1227–1236.
23. van der Kolk BM, de Man BM, Wobbes T, Hendriks T. Is early post-operative treatment with 5-fluorouracil possible without affecting anastomotic strength in the intestine? Br J Cancer. 1999; 79:545–550.
24. Konstantinidis HD, Slavakis AP, Ballas KD, Sioga AC, Economou LD, Demertzidis CI, et al. The effect of capecitabine on the healing of colonic anastomoses in rats. Dis Colon Rectum. 2007; 50:89–96.
25. Graf W, Weiber S, Glimelius B, Jiborn H, Påhlman L, Zederfeldt B. Influence of 5-fluorouracil and folinic acid on colonic healing: an experimental study in the rat. Br J Surg. 1992; 79:825–828.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download