Abstract
Purpose
Ultrasonographic (US) criteria on malignant thyroid bed mass have been suggested, including taller than wide shape, loss of echogenic hilum, abnormal vascularity, and microcalcification. The relationship between fine-needle aspiration (FNA) cytology findings and US findings on thyroid bed mass is unknown. We have retrospectively assessed the malignant thyroid bed mass after total thyroidectomy due to papillary thyroid carcinoma (PTC).
Methods
We retrospectively evaluated 2,048 patients who underwent total thyroidectomy due to PTC. FNA was performed in 97 patients on the thyroid bed under US surveillance. The 97 suspicious thyroid bed masses were divided into two groups: metastatic thyroid bed group (n = 34) and nonmetastatic group (n = 63). The groups were evaluated according to various clinical, serologic, and US findings.
Results
Within a median 47.0 months of follow-up, the proportion of malignant thyroid bed mass was high in large tumor size (1.37 cm vs. 1.03 cm), isthmic position (10.3% vs. 3.9%), and previous N1a (55.9% vs. 34.9%). US findings revealed that the presence of microcalcification or macrocalcification (47.1% vs. 19.0%) and thyroid bed mass height (5.4 mm vs. 3.9 mm) were the only discriminable criteria for central compartment recurrence. But, degree of echogenicity, loss of hilum, and irregularity of margin failed to discriminate malignant thyroid bed mass.
According to the revised American Thyroid Association thyroid cancer guidelines [1], neck ultrasonography to evaluate the thyroid bed, and the central and lateral cervical nodal compartments should be performed 6-12 months after initial surgery and then periodically, depending on the patient's risk for recurrence and thyroglobulin (TG) status. Locoregional recurrence of papillary thyroid cancer (PTC) with reported rates of 15-25% occur in either cervical lymph nodes or in the thyroid bed [2,3], and careful structural evaluation of the neck is a key component of the follow-up surveillance.
In addition to identifying normal and abnormal cervical lymph nodes, ultrasonography often detect small discrete nodules in the postoperative thyroid bed. Most are benign lesions such as postoperative scar or suture granulomas. However, some represent persistent thyroid cancer on the thyroid bed. The ultrasonographic (US) appearance of lateral cervical lymphadenopathy is useful in distinguishing benign from malignant cervical lymph nodes (cystic changes, taller than wide shape, abnormal vascularity, loss of echogenic hilum, and microcalcification or macrocalcification) [4-10]. However, these sonographic findings may not accurately predict small malignant thyroid bed mass [11-14].
Many studies have attempted to identify the characteristics of malignant thyroid bed mass and cervical lymphadenopathy. US criteria have been suggested, including taller than wide shape, loss of echogenic hilum, abnormal vascularity, and microcalcification. The relationship between fine-needle aspiration (FNA) cytology findings and US findings on thyroid bed mass is unknown. So, we addressed this shortcoming by evaluating various US findings on malignant thyroid bed mass detected after total thyroidectomy.
Between May 2004 and April 2008, 2,048 patients underwent total thyroidectomy due to thyroid malignancy Gwangju and Hwasoon Chonnam National University Hospital. Of these, 98 patients (4.56%) developed central or lateral neck recurrence. After obtaining approval from our Institutional Review Board, we retrospectively reviewed these patients' records and US data, and investigated the US report. FNA was attempted in 97 patients on the thyroid bed and in 119 patients on the lateral neck under US surveillance. Suspicious thyroid bed masses were divided into two groups (metastatic thyroid bed group, n = 34; nonmetastatic group, n = 63) and the various clinical, serologic, and US findings were evaluated.
To be eligible, patients had to have at least one aspiration or surgically confirmed thyroid bed mass after surgery. Patients were excluded from the study for the following reasons: not enough data on follow-up or US, pediatric patients, medullary or follicular thyroid cancer patients, patients with other abnormal findings on lateral cervical lymph nodes such as previous lymphoma or other cancer history, and previous history of pulmonary or visceral tuberculosis.
US features of thyroid bed masses that underwent US-guided FNA included height and width, echogenicity, marginal status, abnormal vascularity, and presence of microcalcifications or macrocalcifications of thyroid bed nodules and cervical lymph nodes. Images of biopsied nodules were obtained with one image in the transverse plane and one image in the longitudinal plane. Thyroid bed masses were classified as suspicious and biopsy was done when one or more of the aforementioned malignant suspicious US findings were evident. Echogenicity was characterized relative to strap muscles. Microcalcifications or macrocalcifications were defined as multiple punctate bright echoes with or without acoustic shadowing. Thyroid bed nodules considered to have increased vascularity included those with either peripheral or intranodular vascular flow. Hypoechogenicity, internal vascular flow, and microcalcifications in thyroid bed nodules were classified as suspicious sonographic features, as previously reported [12]. All of the suspicious thyroid bed masses were needle aspirated under US-guided targeting. US-FNA was performed with a 27-gauze needle attached to a disposable 10 mL syringe using a free-hand technique. Each lesion was aspirated at least three times.
We used the t-test to compare continuous variables between each group and the chi-square test for categorical variables. Receiver operating characteristic (ROC) curve analysis was also used to compare diagnostic performance. The diagnostic performance of each of the criteria were reported as sensitivity, specificity, positive predictive value, negative predictive value, accuracy, and area under the ROC curve with 95% confidence intervals. Binary logistic regression test was used for multivariate analysis of statistically significant variables from the univariate analysis. Statistical significance was indicated by a P-value < 0.05. Results were analyzed using PASW ver. 18.0 (IBM Co., Armonk, NY, USA).
Within a median 47.0 months of follow-up, 216 patients (10.6%) had FNA cytology on suspicious lesions in 97 central and 119 lateral necks. Of these patients, 34 (35.1%) and 63 (53.7%) were confirmed with central or lateral neck recurrence. Thus, the positive predictive value on thyroid bed mass was significantly lower than that on lateral cervical nodes. Among the enrolled 97 thyroid bed masses, 34 had malignant cytology results, but 49 (50.5%) had benign results. Of the patients proven to have a nonmalignant thyroid bed mass, there were 30 (61.2%) reactive hyperplasia of lymph nodes, seven (14.3%) remaining thyroid or thyroiditis, four (8.2%) postoperative scar tissue containing histiocytes and neutrophils, two (4.1%) parathyroid glands, and two (4.1%) suture granulomas. Four patients were nondiagnostic due to bloody smear. Fourteen (14.4 %) were observed without FNA cytology and disappeared on follow-up US or diagnostic scans, or have been serologically negative to date.
Clinicopathologic features of the 97 patients with thyroid bed masses detected on routine follow-up neck US after total thyroidectomy are presented in Table 1. Median age was 46.0 years. Central and lateral neck node dissection was done in 70 (72.2%) and 15 patients (15.5%), respectively, and 58.6% had central neck metastases. Hemostasis was done with absorbable tie material in 22 patients (22.7%) and with nonabsorbable silk tie material in 70 patients (77.3%). Postoperative radioactive iodine ablation was done in 46 patients (47.9%) and the mean dose was 122.6 mCi. Median time for FNA was 22 months (range, 2 to 81 months) after thyroid surgery.
Patients were divided into two groups: metastatic thyroid bed group (n = 34) and nonmetastatic (n = 63) group. Age, sex, and body mass index were not significantly different between the two groups. The proportion of metastatic thyroid bed mass was high in patients with large primary tumor size (1.37 cm vs. 1.03 cm, respectively; P = 0.001), isthmic position (10.3% vs. 3.9%, respectively; P = 0.037), and previous central metastasis (55.9% vs. 34.9%, respectively; P = 0.046). As for other primary tumor characteristics, bilaterality, marginal positivity, lymphovascular invasion, and extrathyroidal extension were not significantly different in multiplicity. Use of nonabsorbable silk tie material was not different in both groups (73.5% vs. 79.4%, respectively; P = 0.513), and larger dose (84.7 mCi vs. 45.2 mCi, respectively; P = 0.001) of radioactive iodine ablation after total thyroidectomy were related to metastatic groups. Follow-up period and the times of FNA were not significantly different (Table 2).
Height of the thyroid bed mass was significantly larger in the metastatic group (5.4 mm) vs. the nonmetastatic group (3.9 mm) (P = 0.003). Other dimensions such as width or taller-than-wide shape were not different. We assumed echogenicity, marginal irregularity, abnormal vascularity, and loss of hilum to be factors for metastatic thyroid bed mass, as is in other studies [4-10]. But, only microcalcification or macrocalcification findings were observed statistically more frequently (52.9% vs. 31.7%, respectively; P = 0.041). TG levels at suspicious findings on US were usually helpful for making decision for FNA. The proportion of elevated TG was greater but was not statistically significant (1.1 IU/mL vs. 0.1 IU/mL, respectively; P = 0.223) (Table 3).
The cut-off values of various continuous variables in relation to malignant thyroid bed mass were analyzed through ROC curve and the area under curve (AUC). Primary tumor size over 1.0 cm (AUC, 0.715), thyroid bed mass height over 0.4 cm (AUC, 0.713), width over 0.7 cm (AUC, 0.600), and TG levels at the time of suspicious findings was 0.3 IU/mL (AUC, 0.677). Sensitivity and specificity of cutoff values of these variables proved to be good predictors (Table 4).
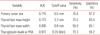
The risk of thyroid bed metastasis in relation to primary tumor and nodal status, US findings, and TG levels at the time of suspicious findings was analyzed with categorical values. The proportion of thyroid bed metastasis in the biopsied nodules was higher in primary tumor sizes over 1.0 cm (75.9% vs. 32.8%, respectively), previous central metastasis (55.9% vs. 34.9%, respectively), thyroid bed mass height over 0.4 cm (58.8% vs. 31.7%, respectively), microcalcification or macrocalcification (47.1% vs. 19.0%, respectively), and TG >0.3 IU/mL were significant (Table 5). In multivariate analysis, primary tumor size over 1.0 cm (P = 0.000), thyroid bed mass height over 0.4 cm (P = 0.013), and microcalcifications or macrocalcifications (P = 0.008) were significant. Also, in Cox analysis, the risk of thyroid bed metastasis was significantly higher in those with primary tumor size over 1.0 cm (odds ratio [OR], 3.372), thyroid bed mass height over 0.4 cm (OR, 2.844), and microcalcification or macrocalcification (OR, 4.935) (Table 6). These were independent predictive factors of thyroid bed metastasis. Diagnostic accuracy of various variables on prediction of malignant thyroid bed mass was calculated. Of these factors, thyroid bed mass height over 0.4 cm and microcalcification or macrocalcification findings exhibited an accuracy of 84.0% and 76.0% for the prediction of malignant thyroid bed mass, and negative predictive value of primary tumor size over 1.0 cm was 85.4% (Table 7). The risk of thyroid bed metastasis was better indicated by US rather than by primary tumor status or laboratory findings. Surprisingly, echogenicity, loss of hilum, and marginal irregularity poorly discriminated the malignant thyroid bed mass.
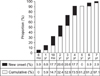
We recommended routine US surveillance at 6 months and 1 year after surgery, then once or twice a year thereafter. Most new onset thyroid bed metastasis was observed by 2 years (53% of patients) and 91.2% of the metastases has occurred by 4 years. In the subsequent year, metastases developed in 8.8% of patients (Fig. 1).
US findings of metastatic lymph nodes have been well-reported [15-18]. However, thyroid bed recurrence is less clear [19,20]. Until now, diagnostic criteria for selecting the thyroidectomy bed lesions to biopsy have not been clearly established [20]. Also, prediction of malignancy cannot be made on the basis of the sonographic findings without FNA cytology [12]. In our study, positive predictive values of US-guided FNA on central or thyroid bed mass were significantly lower than that on lateral cervical nodes (35.1% vs. 53.7%). So, we evaluated the various clinical and US findings on malignant thyroid bed mass on thyroid bed mass, rather than lateral cervical nodes.
Large tumor size, previous lymph node metastasis, and the isthmic position of tumor were associated with thyroid bed recurrences. Height and microcalcification or macrocalcification findings of thyroid bed mass were significant predictors. Width, echogenicity, marginal status, loss of nodal hilum, and, especially, taller-than-wide shape of thyroid bed mass were not significant.
In a recent study, taller-than-wide shape in malignant thyroid nodules and the reverse situation in benign nodules were related to the ability of the probe to compress the thyroid nodule during the US examination. Since benign nodules and cystic nodules are softer and infiltrate less into the surrounding tissue, benign nodules are more easily compressed than malignant nodules [21]. We assumed that the compressibility on malignant thyroid bed mass would disappear due to lack of the thyroid gland after thyroidectomy.
Thyroid bed masses are commonly seen in the routine follow-up after total thyroidectomy. Although the revised American Thyroid Association guidelines allow for observation without FNA cytology of small abnormal cervical lymph nodes [1], there are no specific recommendations regarding the management of small thyroid bed nodules. This is significantly higher than those who have thyroid bed mass height over 0.4 cm (accuracy, 84.0%), those who have microcalcification or macrocalcifications on sonographic surveillance (accuracy, 76.0%), and those who have primary tumor size over 1.0 cm (negative predictive value, 85.4%). These were independent predictive factors of malignant thyroid bed metastasis. Unfortunately, echogenicity, loss of hilum, and marginal irregularity poorly discriminated the malignant thyroid bed mass, although these were good predictors for lateral metastatic nodes.
Ultrasound is more sensitive than serum TG levels and radioactive iodine scans for detection of recurrence, and ultrasound should be indicated, even in low-risk thyroid cancer patients [19]. In our study, TG levels at suspicious findings did not achieve as high accuracy (only 56%) as could have been expected. Regular US evaluations seem to be a very reasonable approach to management. The absence of suspicious sonographic findings combined with the absence of other abnormal cervical lymph nodes and rising serum TG can provide clinicians with a strong predictor for clinical quiescence over several years of follow-up.
This study is limited by its retrospective nature and thyroid bed masses without definite cytological results were included. Neck ultrasonography on nondiagnostic or nonaspirated thyroid bed mass was followed until the end of this study, but all were followed without any evidence of clinical, serologic, and other diagnostic scan or positron emission tomography. Secondly, the diagnosis of thyroid bed mass and recommendation for US-guided FNA is usually based on the combination of suspicious features of radiologic findings and serologic criteria such as TG over 1.0 mIU/mL, and included hot uptake on previous diagnostic scans. But, we had a large number of negative lesions on FNA cytology. The relatively large number of negative results suggests that the diagnostic criteria used to determine whether a lesion should be biopsied were based on traditional US findings on lymph nodes.
In our study, US findings on malignant thyroid bed mass were different from previously reported general criteria on lateral metastatic nodes. Additional FNA cytology should be performed on patients presenting with these findings, even low-risk patients. Postoperative follow-up could be guided more easily by using the US criteria as well as the clinical and serologic monitoring.
Figures and Tables
Table 5
Metastasis in the thyroid bed according to the fine-needle aspiration cytology by preoperative tumor status and ultrasonographic findings and thyroglobulin levels at that time

References
1. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009; 19:1167–1214.
2. Mazzaferri EL, Kloos RT. Clinical review 128: current approaches to primary therapy for papillary and follicular thyroid cancer. J Clin Endocrinol Metab. 2001; 86:1447–1463.
3. Hay ID, Thompson GB, Grant CS, Bergstralh EJ, Dvorak CE, Gorman CA, et al. Papillary thyroid carcinoma managed at the Mayo Clinic during six decades (1940-1999): temporal trends in initial therapy and long-term outcome in 2444 consecutively treated patients. World J Surg. 2002; 26:879–885.
4. Fish SA, Langer JE, Mandel SJ. Sonographic imaging of thyroid nodules and cervical lymph nodes. Endocrinol Metab Clin North Am. 2008; 37:401–417.
5. Rosario PW, de Faria S, Bicalho L, Alves MF, Borges MA, Purisch S, et al. Ultrasonographic differentiation between metastatic and benign lymph nodes in patients with papillary thyroid carcinoma. J Ultrasound Med. 2005; 24:1385–1389.
6. Takashima S, Sone S, Nomura N, Tomiyama N, Kobayashi T, Nakamura H. Nonpalpable lymph nodes of the neck: assessment with US and US-guided fine-needle aspiration biopsy. J Clin Ultrasound. 1997; 25:283–292.
7. Ying M, Ahuja A, Metreweli C. Diagnostic accuracy of sonographic criteria for evaluation of cervical lymphadenopathy. J Ultrasound Med. 1998; 17:437–445.
8. Lyshchik A, Higashi T, Asato R, Tanaka S, Ito J, Hiraoka M, et al. Cervical lymph node metastases: diagnosis at sonoelastography: initial experience. Radiology. 2007; 243:258–267.
9. Kuna SK, Bracic I, Tesic V, Kuna K, Herceg GH, Dodig D. Ultrasonographic differentiation of benign from malignant neck lymphadenopathy in thyroid cancer. J Ultrasound Med. 2006; 25:1531–1537.
10. Leboulleux S, Girard E, Rose M, Travagli JP, Sabbah N, Caillou B, et al. Ultrasound criteria of malignancy for cervical lymph nodes in patients followed up for differentiated thyroid cancer. J Clin Endocrinol Metab. 2007; 92:3590–3594.
11. Kim JH, Lee JH, Shong YK, Hong SJ, Ko MS, Lee DH, et al. Ultrasound features of suture granulomas in the thyroid bed after thyroidectomy for papillary thyroid carcinoma with an emphasis on their differentiation from locally recurrent thyroid carcinomas. Ultrasound Med Biol. 2009; 35:1452–1457.
12. Shin JH, Han BK, Ko EY, Kang SS. Sonographic findings in the surgical bed after thyroidectomy: comparison of recurrent tumors and nonrecurrent lesions. J Ultrasound Med. 2007; 26:1359–1366.
13. Lee JH, Lee HK, Lee DH, Choi CG, Gong G, Shong YK, et al. Ultrasonographic findings of a newly detected nodule on the thyroid bed in postoperative patients for thyroid carcinoma: correlation with the results of ultrasonography-guided fine-needle aspiration biopsy. Clin Imaging. 2007; 31:109–113.
14. Frates MC. Ultrasound in recurrent thyroid disease. Otolaryngol Clin North Am. 2008; 41:1107–1116.
15. Sohn YM, Kwak JY, Kim EK, Moon HJ, Kim SJ, Kim MJ. Diagnostic approach for evaluation of lymph node metastasis from thyroid cancer using ultrasound and fine-needle aspiration biopsy. AJR Am J Roentgenol. 2010; 194:38–43.
16. Ahuja AT, Chow L, Chick W, King W, Metreweli C. Metastatic cervical nodes in papillary carcinoma of the thyroid: ultrasound and histological correlation. Clin Radiol. 1995; 50:229–231.
17. Ahuja AT, Ying M, Yuen HY, Metreweli C. Power Doppler sonography of metastatic nodes from papillary carcinoma of the thyroid. Clin Radiol. 2001; 56:284–288.
18. Antonelli A, Miccoli P, Ferdeghini M, Di Coscio G, Alberti B, Iacconi P, et al. Role of neck ultrasonography in the follow-up of patients operated on for thyroid cancer. Thyroid. 1995; 5:25–28.
19. Frasoldati A, Pesenti M, Gallo M, Caroggio A, Salvo D, Valcavi R. Diagnosis of neck recurrences in patients with differentiated thyroid carcinoma. Cancer. 2003; 97:90–96.
20. Kamaya A, Gross M, Akatsu H, Jeffrey RB. Recurrence in the thyroidectomy bed: sonographic findings. AJR Am J Roentgenol. 2011; 196:66–70.
21. Yoon SJ, Yoon DY, Chang SK, Seo YL, Yun EJ, Choi CS, et al. "Taller-than-wide sign" of thyroid malignancy: comparison between ultrasound and CT. AJR Am J Roentgenol. 2010; 194:W420–W424.




 ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download