Abstract
It is important that extrahepatic arteries are identified precisely at the time of graft procurement. We present a case where the accessory right hepatic artery of the liver was ligated leading to postoperative liver abscess formation in the liver graft. A forty-seven-year-old female patient diagnosed with liver cirrhosis underwent orthotopic cadaveric liver transplantation due to altered mentality. The donor graft showed a variant of the hepatic artery anatomy where an accessory right hepatic artery arose from the superior mesenteric artery. This artery was accidentally transected during procurement. Since the back bleeding test using perfusion fluid was good, the artery was ligated. Postoperative abdominal computed tomography scan revealed a 6 cm low attenuating lesion in the liver. The patient underwent conservative treatment. We believe that even small accessory arteries (1 to 2 mm) should be reconstructed whenever possible to avoid postoperative complications such as liver abscess.
Liver transplantation is the treatment of choice for patients with end-stage liver disease. During the last decade, improvements in immunosuppressive drugs, surgical techniques, and preservation fluids have achieved better short-term and long-term outcomes. It is well known that during donor hepatectomy, recognition of hepatic arterial variations is mandatory for the safety of the graft and of the recipient. The absence of an adequate hepatic arterial supply usually results in graft loss or ischemic biliary injuries. Vascular complications after liver transplantation are associated with a poor outcome for both the graft and the patient. The most common vascular complication after liver transplantation is hepatic artery thrombosis, occurring in 2 to 12% of transplants [1].
The vascular anatomy of the liver is varied. The "normal" anatomy i.e., the common hepaticartery originating from the celiac trunk and branching close to the parenchyma into the left and right hepatic arteries is seen in 55 to 80% of the cases [2-5]. Under variant patterns, the lobes may receive blood supply from the superior mesenteric artery (SMA), left gastric artery, aorta, or other visceral branches. These vessels may be accessory, occurring in addition to the normal arterial supply, or replaced, representing the primary arterial supply to the lobe. It is important that extrahepatic arteries are identified precisely at the time of graft procurement to avoid injuries that might compromise liver function. Thus, the presence of all arteries that are accessory or replaced must be demonstrated. Whether an individual vessel is accessory or replaced is not always determined, because the intrahepatic branches are not dissected. In 42% of cases of variant hepatic arterial anatomy a reconstruction was required before liver transplant [2-5]. We present a case where the accessory right hepatic artery of the liver was ligated leading to postoperative liver abscess formation in the posterior section of the liver graft.
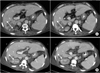
A forty-seven-year-old female patient diagnosed with cryptogenic liver cirrhosis underwent orthotopic cadaveric liver transplantation due to altered mentality. Her model for end stage liver disease score was 33. During the operation, the donor graft showed a variant of the hepatic artery anatomy where anaccessory right hepatic artery arose from the SMA presumably supplying the posterior section of the liver graft. This artery was accidentally transected during procurement. At the back table, anastomosis of the accessory artery, the size of which was 1 mm, with the gastroduodenal artery (GDA) or splenic artery was not possible due to size discrepancy. Since the back bleeding test using organ preservation fluid (Custodiol HTK solution, Dr. Franz Köhler Chemie GmbH, Bensheim, Germany) was good, the artery was ligated. Although the initial aspartateaminotransferase and alanineaminotransferase levels were 2,871 IU/L and 1,539 IU/L, respectively, they began to decrease postoperatively. The postoperative doppler sonogram demonstrated normal wave form of the right and left hepatic arteries with a resistive index of 0.6 (Fig. 1). On the tenth postoperative day, an abdominal computed tomography (CT) scan among other studies was performed due to persistent fever and positive blood cultures for enterococci. The CT scan revealed a 6 cm multilobulating low attenuating lesion in the right posterior section of the liver (Fig. 2A). With the impression of liver abscess, the patient underwent conservative treatment including antibiotic therapy using vancomycin and levofloxacin. On follow-up CT scans, the size of the lesion decreased without any draining procedure (Fig. 2B).
Michels' classic autopsy series of 200 dissections, published in 1966, defined the basic anatomic variations in hepatic arterial supply and has served as the benchmark for all subsequent contributions in this area. Variant patterns occurred in 45% of cases, and arteries could be defined as accessory or replaced because dissection was carried into the liver substance. Michels' motivation was to maximize the database for surgeons performing procedures in and around the portahepatis, to avoid injury to vascular and ductal structures [2].
Complications associated with hepatic artery reconstructions are one of the major causes of graft loss and mortality after orthotopic liver transplantation (OLT) [6]. Hepatic artery complications after OLT include hepatic artery thrombosis, hepatic artery stenosis, hepatic artery pseudoaneurysm, and hepatic artery fistula. The early complications of hepatic artery are usually caused by technical problems. The late complications of hepatic artery are usually associated with hypercoagulable state, over transfusion of platelets and fresh frozen plasma during the surgery, severe rejection, and bileleakage [6]. The hepatic artery is relatively small (3 to 6 mm in diameter in adults) and has a very fragile intima that requires a careful atraumatic manipulating technique during reconstruction [7]. The anatomical variations, diameter and length of hepatic artery, and injury to vessels including prolonged clamping of hepatic artery, kinking of a long artery, and hematoma of the artery wall from improper flushing afterclamping during operation, and the quality of recipient vessels and mismatch between donor and recipient arterial vessels should be carefully considered and managed preoperatively and intraoperatively [6,7].
The detection of accessory hepatic arteries is an important issue during liver harvesting procedures [3,8]. The most frequent is the presence of an accessory artery supplying the left hepatic lobe from the left gastric artery [2]. This variation is not by itself an indication for vascular reconstruction [3,8]. What is important is the detection of an additional vessel supplying the right liver lobe from the SMA, which is also one of the most common anatomic variations of the donor hepatic artery in liver transplantation [2,3,8]. Most typically, this artery runs backward from the head of the pancreas to the rear portion of the hepatoduodenal ligament. This topographic pattern mayoften be difficult to diagnose; it is frequently responsible for inadvertent damage to the arterial system during the harvesting procedure [3,8]. Several methods for reconstruction have been described [6-8]. In a report by Di Benedetto et al. [8], after preserving the SMA stump (with the right hepatic artery branching from the SMA) originating from the aorta during donor procurement, they proposed a method in which the recipient common hepatic artery is anastomosed to the distal end of the donor SMA, and the proximal end of the donor SMA is anastomosed to the donor proper hepatic artery. Since the accessory right hepatic artery was inadvertently transected away from the origin of the SMA during procurement, in addition to size discrepancy between the accessory right hepatic artery and GDA or splenic artery, reconstruction using the above methods was not possible.
In a study by Ikegami et al. [9], during living-related liver transplantation (LRLT), where multiple graft arteries were present, both were anastomosed when the largest two were almost the same in diameter. When differences in diameter were noted among the graft arteries, the thickest one was reconstructed first. When pulsatile blood flowed from the stumps that had not been anastomosed the remaining arteries were not anastomosed. When pulsatile bleeding from the nonanastomosed stumps was not observed after rearterialization of the largest artery, all were anastomosed to the recipient hepatic arteries. They concluded that although several hepatic arteries may supply the potential allograft in LRLT, it is not always necessary to reconstruct all of them [9]. In the present case, back bleeding was tested using perfusion fluid. We believe that back bleeding might have been more accurately evaluated after reconstruction of the main hepatic artery.
However, Yanaga et al. [10] reported the clinical course of five patients with partial dearterialization of their hepatic allografts. One patient died and three others suffered serious morbidity as a direct or indirect result of this complication. They concluded that partial dearterialization of the liver allograft results in a serious and potentially life-threatening complication for which preservation of the complete hepatic arterial supply is important, even if this requires reconstruction of the aberrant vessels [10]. In addition, hepatic artery ligation can lead to liver infarction and subsequent liver abscess [10].
In conclusion, although the liver abscess subsided in our patient, since whether an individual vessel is accessory or replaced is not always determined, we believe that even small accessory arteries (1 to 2 mm) should be reconstructed whenever possible even if good back bleeding exists to avoid postoperative complications such as liver abscess.
Figures and Tables
Notes
References
1. Tzakis AG, Gordon RD, Shaw BW Jr, Iwatsuki S, Starzl TE. Clinical presentation of hepatic artery thrombosis after liver transplantation in the cyclosporine era. Transplantation. 1985. 40:667–671.
2. Michels NA. Newer anatomy of the liver and its variant blood supply and collateral circulation. Am J Surg. 1966. 112:337–347.
3. Nelson TM, Pollak R, Herand OJ. Anatomic variants of the celiac, superior mesenteric, and inferior mesenteric arteries and their clinical relevance. Clin Anat. 1988. 1:75–91.
4. Hiatt JR, Gabbay J, Busuttil RW. Surgical anatomy of the hepatic arteries in 1000 cases. Ann Surg. 1994. 220:50–52.
5. Yang SH, Yin YH, Jang JY, Lee SE, Chung JW, Suh KS, et al. Establishment of a guideline for the safe management of anatomical hepatic artery variations while performing major hepato-pancreatico-biliary surgery. J Korean Surg Soc. 2009. 76:100–108.
6. Proposito D, Loinaz Segurola C, Garcia Garcia I, Jimenez C, Gonzales Pinto I, Gomez Sanz R, et al. Role of anatomic variations and methods of hepatic artery reconstruction in the incidence of thrombosis following liver transplantation. Ann Ital Chir. 2001. 72:303–314.
7. Jones RM, Hardy KJ. The hepatic artery: a reminder of surgical anatomy. J R Coll Surg Edinb. 2001. 46:168–170.
8. Di Benedetto F, Cautero N, De Ruvo N, Masetti M, Montalti R, Gerunda GE, et al. A new reconstruction of the accessory donor right hepatic artery with interposition of the SMA in liver transplantation. Surgery. 2006. 140:835.
9. Ikegami T, Kawasaki S, Matsunami H, Hashikura Y, Nakazawa Y, Miyagawa S, et al. Should all hepatic arterial branches be reconstructed in living-related liver transplantation? Surgery. 1996. 119:431–436.
10. Yanaga K, Tzakis AG, Starzl TE. Partial dearterialization of the liver allograft. Transpl Int. 1990. 3:185–188.




 ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download