Abstract
Purpose
To determine the risk factors of delayed recanalization of isolated calf vein thrombosis (CVT).
Methods
One hundred fifty limbs of 110 patients with CVT between September 2007 and April 2010 were enrolled. We used ultrasonography for the diagnosis and follow-up examinations of CVT. We calculated recanalization rates at 1 and 3 months after initial diagnosis and analyzed the risk factors associated with delayed recanalization of CVT.
Results
CVTs were located in the muscular calf vein in 110 (73.3%), in the deep calf vein in 18 (12%), and in both in 22 cases (14.7%). Among all CVTs, 94 limbs (63%) were symptomatic. Major risk factors for CVT were orthopedic surgery (87.3%), malignancy (21.3%), and immobilization (15.3%). Sixty-seven patients (60.9%) were treated with oral anticoagulation therapy, while 43 patients by low molecular weight heparin (n = 19) or by conservative methods including elastic compression stockings and ambulation (n = 21). The cumulative recanalization rate at 1 and 3 months was 23% and 82% and it was significantly higher in patients who underwent oral anticoagulation therapy compared with patients without oral anticoagulation therapy (84% vs. 65%, P = 0.008 by log-rank test). Malignancy (odds ratio [OR], 2.789; P = 0.043) and immobilization (OR, 4.191; P = 0.029) were independent risk factors for delayed recanalization of CVT and oral anticoagulation (OR, 0.300; P = 0.020) was an independent factor in promoting recanalization in multivariate analysis.
Isolated calf vein thrombosis (CVT) is comprised of muscular (soleal and gastrocnemius sinus) and deep (posterior tibial, anterior tibial, and peroneal veins) venous thrombosis (DVT) in the calf. Unlike proximal DVT, the clinical importance of CVT has often been underestimated. CVTs are more frequently detected and its clinical significance has been discussed since ultrasonography (US) was first used for the diagnosis of DVT [1,2]. The prevalence of CVT is 5 to 12% in patients with symptomatic venous thrombosis [3]. CVT may develop in 15% of asymptomatic patients after hip and knee surgery, and in 45% of patients after coronary bypass grafting [4-6].
For the treatment of CVT, international guidelines recommend three months of oral anticoagulation therapy at the full therapeutic dosage [7]. However, in clinical practice, we have encountered frequent resolution of CVT after short-duration anticoagulation therapy, as well as cases of spontaneous resolution. Therefore, questions have been raised regarding the optimal duration of anticoagulation for patients with CVT and risk factors for delayed recanalization after anticoagulation.
The purposes of this study were to observe recanalization rates in CVT patients at 1 and 3 months, and to determine the risk factors related to delayed recanalization of CVT.
Approval was obtained from our Institutional Review Board to review medical records and the results of imaging studies. We selected CVT patients diagnosed and treated between September 2007 and April 2010 from the patient database of the vascular lab. Asymptomatic patients were diagnosed as a surveillance protocol in orthopedic surgery or neurosurgery for the high risk patients. Only the patients who had follow-up duplex US (iU 22, Phillips, Best, The Netherlands; ACUSON Antares, Simens AG, Munich, Germany) for 1 month or longer were included in this study.
Patients with concurrent proximal DVT or a prior history of unilateral leg swelling were excluded from this study. Diagnoses of acute CVT were made based on duplex US findings and diagnosis of pulmonary embolism (PE) was made with CT scan. All duplex US examinations were performed by three experienced registered vascular technologists. Veins in both lower extremities were examined with duplex US from the inferior vena cava to the calf veins following a standardized method. In brief, compressibility, presence of venous flow, and presence of intravenous echoic material in the anterior tibial, posterior tibial, and peroneal veins, as well as the soleal and gastrocnemius veins, were examined in legs in a dependent position.
After detection of CVT, all the patients were recommended to prescribe anticoagulation therapy if possible, except the patients with contraindication to anticoagulation or risk of bleeding. For the purpose of anticoagulation, nineteen patients (17.3%) were treated only with low-molecular-weight heparin (LMWH) (median, 5 days; range, 1 to 5) and 67 patients (60.9%) were treated with LMWH and overlapped sufficiently and followed by oral anticoagulants (warfarin) for 37.0 days (range, 11 to 268 days) targeting 2 to 3 international normalized ratio of prothrombin time. Fifteen patients (13.6%) were prescribed oral anticoagulants for longer than six months due to concurrent PE or persistence of major risk factors for venous thromboembolism (VTE). Twenty-four patients (21.8%) who were incompliant to our prescription of anticoagulation therapy were managed conservatively with elastic compression stockings and leg elevation. Finally, oral anticoagulation therapy was performed 64% (60 of 94 limbs) in symptomatic patients and 61% (34 of 56 limbs) in asymptomatic patients, respectively.
Wearing elastic compression stockings was recommended for all patients. Early ambulation was also encouraged if possible. When follow-up duplex US at one month showed persistence or incomplete resolution of CVT, anticoagulation therapy was extended for two more months or more. Duplex US examinations were performed at 1 and 3 months after diagnosis of CVT for all patients.
To determine the risk factors of delayed recanalization of the calf vein, the coexisting risk factors of DVT (recent surgery, trauma, lengthy air or car travel, immobilization, coexisting cancer, use of oral contraceptives), location of CVT (muscular vs. tibial and peroneal vein), presence of calf pain or swelling, oral anticoagulation or not were included in the statistical analysis. We compared recanalization rate in 3-month follow-up duplex scan between oral anticoagulation with warfarin group (n = 67) and no oral anticoagulation group (n = 43) using the Kaplan-Meier method. In addition, we tried to identify the risk factors of delayed recanlaization of CVT.
Data analyses were performed using IBM SPSS ver. 18.0 (IBM Co., New York, NY, USA). Continuous variables were described as mean ± SD, and the Student's t-test was used for comparisons. Categorical variables were described as number and percentage and chi-Square test was used for comparison. The recanalization rates of CVT at 1 and 3 months were calculated using the Kaplan-Meier method. For the assessment of risk factors of delayed recanalization of CVT, a simple logistic regression test in univariate analysis and binary logistic regression test in multivariate analysis were used. P-values less than 0.05 were considered statistically significant.
During the study period, data for 292 limbs with isolated CVT in 213 patients were collected at a single institute. One hundred fifty limbs (51.4%) in 110 patients (87 females; mean age, 63.4 ± 11.2 years; range, 23 to 80 years) were available to follow-up examinations and included in this study.
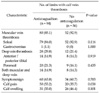
A comparison of patient demographics and coexisting risk factors for VTE between patients who received anticoagulation and those who did not is shown in Table 1. There were no significant differences in the frequencies of risk factors between the two groups except for cases in which the patient had a history of recent surgery, which were more common in anticoagulation group than in the no anticoagulation group (94% vs. 74.4%, P = 0.003). The most common coexisting risk factor for DVT was recent surgery, which occurred in 95 patients (86.4%), of which orthopedic surgery (knee or hip replacement arthroplasty) was the most prevalent (77 patients, 70%).
The distributions of CVT and symptoms/signs are shown in Table 2. Thrombosis was located in the unilateral calf in 70 patients (64%) and was bilateral in 40 patients (36%). One hundred thirty-two thromboses (88%) involved the muscular veins (soleal sinus, 131 limbs; gastrocnemius vein, 1 limb), while deep vein were involved in 40 limbs (27%) (tibial vein, 22 limbs; peroneal vein, 29 limbs), and both muscular and deep calf veins were involved in 22 limbs (14.7%). There was no significant difference in the distribution of CVT between the anticoagulation and no anticoagulation groups. CVT was symptomatic in 94 limbs (62.7%) and calf pain was more prevalent in the anticoagulation group than in the no anticoagulation group (53.2% vs. 35.7%, P = 0.038). Symptomatic PE developed in 6 (5.5%) of the CVT patients.
Follow-up examinations with duplex US of CVT were performed in all patients at 1 month and in 128 limbs (85.3%) of 92 patients (83.6%) at 3 months. During the follow-up periods of 3 months, we observed complete recanalization of the calf vein in 94 limbs (62.7%), partial recanalization in 29 (19.3%), and no recanalization in 25 limbs (16.7) with CVT on duplex US. As shown in Fig. 1, according to Kaplan-Meier estimates, the recanalization rate of CVT was significantly higher in the oral anticoagulation group than in the no oral anticoagulation group (84% vs. 64.8%, P = 0.008) (Fig. 1). However, no significant difference was detected in the recanalization rate between muscular CVT and deep CVT (81% vs. 85%, P = 0.564).
According to our univariate risk factor analysis for recanalization of CVT, immobilization, coexisting cancer, recent surgery, and anticoagulation therapy significantly influenced the recanalization of CVT (Table 3). Multivariate analysis revealed that immobilization (P = 0.029; OR, 4.191) and coexisting cancer (P = 0.043; OR, 2.789) were independent risk factors associated with delayed recanalization of CVT, whereas anticoagulation therapy (P = 0.020; OR, 0.300) was likely to promote the recanalization of CVT (Table 4).
Among 110 CVT patients, progression to proximal DVT and PE was detected in 1 (0.9%) of limbs and 6 (5.5%) of patients, respectively. During the follow-up period, three patients (2.7%) died of cancer or gastrointestinal bleeding, however there was no recurrence of CVT or PE during the follow-up period.
Isolated CVT is a common finding but was often ignored until US was used for the diagnosis of venous thrombosis. Incidence of CVT is known to be 100 times higher than that of symptomatic DVT [8,9]. It is assumed that most of these small thrombi resolve completely via natural mechanisms of thrombolysis, although some of them progress to symptomatic or proximal DVT [10]. The clinical importance of CVT arises from its potential risk of progression to the proximal vein and risk of PE. Some cases of CVT have been known to progress into the deep veins as well as to symptomatic PE [11,12]. MacDonald et al. [13] reported on the progression rate of isolated CVT to the level of adjacent tibial or peroneal veins or higher in 22 (16.3%) of the 135 limbs studied and 4 (3%) extensions to the popliteal vein during a 3-month follow-up in a cohort followed by duplex US without any treatment. Schwarz et al. [12] conducted a prospective nonrandomized study including 84 isolated muscular CVTs and showed a significantly higher rate of progression to the deep calf veins (25%) in the 32 patients (38%) who had not undergone anticoagulation therapy [12]. These two studies showed that the proximal extension or progression rates of CVT were higher in patients who were not treated with anticoagulation therapy, and the extension occurred early after the diagnosis in most of the patients. Gillet et al. [14] reported no extension or recurrence rates of CVT at 3 months, but a high (18.8%) rate of VTE recurrence in symptomatic CVT patients in a midterm follow-up (mean, 26.7 months) [14]. In the present study, we observed very low rate (0.9%) of CVT progression to the deep (tibial) vein, and no patient showed recurrent VTE or symptomatic PE during the follow-up period. Previous research regarding the relationship between CVT and PE has proven equivocal. Although Gillet et al. [14] reported on the development of PE in 7% of cases of isolated CVT, others reported 13 to 15% fatal PE in patients with asymptomatic isolated CVT after surgery [15]. Spontaneous resolution of CVT is known to occur, with a 50% reduction of signs and symptoms at one month and complete resolution of symptom or signs by one year in most patients [16]. However, post-thrombotic manifestations develop in 4% of patients, and valvular incompetence occurs in 20 to 24% of patients [17]. MacDonald et al. [13] reported that complete recanalization of the calf vein at 1 and 3 months occurred in 20.7% and 44.6% of cases of muscular CVT, respectively. In our study, overall recanalization rates at 1 and 3 months were 23% and 82%, respectively. There was a significant difference in the recanalization rates between the anticoagulation group and the no anticoagulation group (84% vs. 64.8, P = 0.008). Furthermore, oral anticoagulation therapy was one of the independent factors responsible for the promotion of recanalization of CVT, according to the findings of multivariate analysis.
Although the American College of Chest Physicians guidelines [7] recommend 3 months of anticoagulation therapy for patients with CVT, many physicians and vascular surgeons stop anticoagulation earlier, when the calf vein thrombus and related symptom have disappeared. By understanding the risk factors of delayed recanalization, we can develop a more detailed therapeutic guideline for determining optimal durations of anticoagulation for specific groups of CVT patients to avoid unnecessary anticoagulation therapy.
Seventy-seven percent of CVT patients in our study received immediate anticoagulation therapy after diagnosis of CVT and were treated for a median of 37 days. Among the patients group, thrombus extension occurred in one limb (0.9%) from the muscular vein to the tibial vein.
There were no known risk factors associated with delayed recanalization of CVT. In the present study, we found that coexisting cancer or immobilization had significantly lower recanalization rates, and longer anticoagulation therapy is required for such patients.
This study has limitations including study design that was not randomized and therefore may suffer from selection bias. Second, the maximum 3-month follow-up interval is not sufficient to observe the long-term complications of CVT or recurrence of venous thrombosis. Third, we could not check consistently the hypercoagulability state of the patients like as protein C or S and don't have enough data to analyze because most of the patients were in other department like as orthopedic surgery.
In conclusion, for patients with isolated CVT, no oral anticoagulation resulted in a higher rate of delayed recanalization compared with oral anticoagulation therapy. Risk factors associated with delayed recanalization of the calf veins were coexisting cancer and recent long-term immobilization, and CVT in patients with such risk factors are more likely to require longer anticoagulation than in patients with other risk factors.
Figures and Tables
Fig. 1
Comparison of recanalization rates (by Kaplan-Meyer calculation) between anticoagulated versus non-anticoagulated groups of calf vein thrombosis patients.

References
1. Labropoulos N, Webb KM, Kang SS, Mansour MA, Filliung DR, Size GP, et al. Patterns and distribution of isolated calf deep vein thrombosis. J Vasc Surg. 1999. 30:787–791.
2. Simons GR, Skibo LK, Polak JF, Creager MA, Klapec-Fay JM, Goldhaber SZ. Utility of leg ultrasonography in suspected symptomatic isolated calf deep venous thrombosis. Am J Med. 1995. 99:43–47.
3. Gottlieb RH, Widjaja J. Clinical outcomes of untreated symptomatic patients with negative findings on sonography of the thigh for deep vein thrombosis: our experience and a review of the literature. AJR Am J Roentgenol. 1999. 172:1601–1604.
4. Gottlieb RH, Widjaja J, Tian L, Rubens DJ, Voci SL. Calf sonography for detecting deep venous thrombosis in symptomatic patients: experience and review of the literature. J Clin Ultrasound. 1999. 27:415–420.
5. Oishi CS, Grady-Benson JC, Otis SM, Colwell CW Jr, Walker RH. The clinical course of distal deep venous thrombosis after total hip and total knee arthroplasty, as determined with duplex ultrasonography. J Bone Joint Surg Am. 1994. 76:1658–1663.
6. Reis SE, Polak JF, Hirsch DR, Cohn LH, Creager MA, Donovan BC, et al. Frequency of deep venous thrombosis in asymptomatic patients with coronary artery bypass grafts. Am Heart J. 1991. 122:478–482.
7. Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ, et al. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008. 133:6 Suppl. 454S–545S.
8. Nordstrom M, Lindblad B, Bergqvist D, Kjellstrom T. A prospective study of the incidence of deep-vein thrombosis within a defined urban population. J Intern Med. 1992. 232:155–160.
9. White RH. The epidemiology of venous thromboembolism. Circulation. 2003. 107:23 Suppl 1. I4–I8.
10. Lohr JM, Kerr TM, Lutter KS, Cranley RD, Spirtoff K, Cranley JJ. Lower extremity calf thrombosis: to treat or not to treat? J Vasc Surg. 1991. 14:618–623.
11. Righini M, Paris S, Le Gal G, Laroche JP, Perrier A, Bounameaux H. Clinical relevance of distal deep vein thrombosis. Review of literature data. Thromb Haemost. 2006. 95:56–64.
12. Schwarz T, Schmidt B, Beyer J, Schellong SM. Therapy of isolated calf muscle vein thrombosis with low-molecular-weight heparin. Blood Coagul Fibrinolysis. 2001. 12:597–599.
13. Macdonald PS, Kahn SR, Miller N, Obrand D. Short-term natural history of isolated gastrocnemius and soleal vein thrombosis. J Vasc Surg. 2003. 37:523–527.
14. Gillet JL, Perrin MR, Allaert FA. Short-term and mid-term outcome of isolated symptomatic muscular calf vein thrombosis. J Vasc Surg. 2007. 46:513–519.
15. Giannoukas AD, Labropoulos N, Burke P, Katsamouris A, Nicolaides AN. Calf deep venous thrombosis: a review of the literature. Eur J Vasc Endovasc Surg. 1995. 10:398–404.
16. Lohr JM, Fellner AN. Isolated calf vein thrombosis should be treated with anticoagulation. Dis Mon. 2010. 56:590–600.
17. Meissner MH, Caps MT, Bergelin RO, Manzo RA, Strandness DE Jr. Propagation, rethrombosis and new thrombus formation after acute deep venous thrombosis. J Vasc Surg. 1995. 22:558–567.




 ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download