1. Leaper DJ, van Goor H, Reilly J, Petrosillo N, Geiss HK, Torres AJ, et al. Surgical site infection - a European perspective of incidence and economic burden. Int Wound J. 2004. 1:247–273.
2. Kim JM, Park ES, Jeong JS, Kim KM, Kim JM, Oh HS, et al. Nosocomial Infection Surveillance Committee of the Korean Society for Nosocomial Infection Control. Multicenter surveillance study for nosocomial infections in major hospitals in Korea. Am J Infect Control. 2000. 28:454–458.
3. Ahn YJ, Sohng KY. Factors related to surgical site infections in patients undergoing general surgery. J Korean Acad Fundam Nurs. 2005. 12:113–120.
4. Lee JH, Han HS, Min SK, Lee HK, Lee JH, Kim YW, et al. Surveillance of surgical wound infections among patients from the department of surgery: prospective trial. J Korean Surg Soc. 2004. 66:133–137.
5. Lee S, Kim S, Lee J, Lee K. Risk factors for surgical site infection among patients in a general hospital. Korean J Nosocomial Infect Control. 2007. 12:9–20.
6. Park ES, Kim KS, Lee WJ, Jang SY, Choi JY, Kim JM. The economical impacts of surgical site infections. Korean J Nosocomial Infect Control. 2005. 10:57–64.
7. Sakong P, Lee JS, Lee EJ, Ko KP, Kim CH, Kim Y, et al. Association between the pattern of prophylactic antibiotic use and surgical site infection rate for major surgeries in Korea. J Prev Med Public Health. 2009. 42:12–20.
8. Chang W, Park HG, Kim H, Youm W. Analysis of risk factors in poststernotomy sternal wound infection and mediastinitis after open-heart surgery. Korean J Thorac Cardiovasc Surg. 2003. 36:583–589.
9. Chang WH, Dong WY, Kim H, Oh HC, Han JW, Kim HJ. An influence of modified robicsek sternal wiring after median sternotomy on the postoperative sternal wound infection. Korean J Thorac Cardiovasc Surg. 2009. 42:763–769.
10. Chung JH, Ahn KR, Kim MN, Kim CS, Kang KS, Yoo SH, et al. Intraoperative and postoperative complications in the patients undergoing the pectus excavatum repair by the Nuss procedure: a retrospective study. Korean J Anesthesiol. 2008. 54:646–650.
11. Song SW, Yi G, Lee S, Youn YN, Sul SY, Yoo KJ. Perioperative indicators of stress response and postoperative inflammatory complications in patients undergoing off-pump coronary artery bypass surgery: a prospective observational study. Circ J. 2008. 72:1966–1974.
12. Park CK, Jheon S. Results of surgical treatment for pulmonary aspergilloma. Eur J Cardiothorac Surg. 2002. 21:918–923.
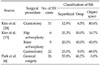
13. Choi YH, Park ES, Chang KH, Yeom JS, Song YG, Chang B, et al. Surgical site infection rates according to patient risk index after cardiovascular surgery. Korean J Nosocomial Infect Control. 1998. 3:11–22.
14. Choi HJ, Park JY, Jung SY, Park YS, Cho YK, Park SY, et al. Multicenter surgical site infection surveillance study about prosthetic joint replacement surgery in 2006. Korean J Nosocomial Infect Control. 2008. 13:42–50.
15. Kim ES, Chang YJ, Park YS, Kang JH, Park SY, Kim JY, et al. Multicenter surgical site infections surveillance system report, 2007: in total hip and total knee arthroplasties and gastrectomies. Korean J Nosocomial Infect Control. 2008. 13:32–41.
16. Kim YW, Han HS, Lee RA, Choi YM, Kim OY. Risk factors of wound infection in biliary surgery: a prospective study. J Korean Surg Soc. 1999. 57:94–99.
17. Lee JH, Kim J, Cheong JH, Hyung WJ, Choi SH, Noh SH. Gastric cancer surgery in cirrhotic patients: result of gastrectomy with D2 lymph node dissection. World J Gastroenterol. 2005. 11:4623–4627.
18. Lee JH, Kim JJ, Kim YH, Jang JK, Son HJ, Peck KR, et al. Increased risk of peristomal wound infection after percutaneous endoscopic gastrostomy in patients with diabetes mellitus. Dig Liver Dis. 2002. 34:857–861.
19. Lee HH, Shim KN, Kwon JM, Jung SA, Yoo K. Complications of percutaneous endoscopic gastrostomy and risk factors of peristomal wound infection. Korean J Med. 2004. 67:15–21.
20. Hong DH, Yu CS, Kim DD, Jung SH, Choi PH, Park IJ, et al. Postoperative complications and recurrence in patients with Crohn's disease. J Korean Soc Coloproctol. 2008. 24:13–19.
21. Jeong YI, Mun SP, Chang JH, Kim KC, Min YD, Kim SH, et al. The risk factors associated with surgical site infection after an abdominal operation. J Korean Surg Soc. 2008. 75:177–183.
22. Kim HB, Ahn HS, Kwon JS, Jung IM, Ahn YJ, Heo SC, et al. Validation of POSSUM-physiological score as predictors of post-operative morbidity and mortality after emergency operation for peptic ulcer complications. J Korean Surg Soc. 2009. 77:391–398.
23. Park JM, Jin SH, Lee SR, Kim H, Jung IH, Cho YK, et al. Complications with laparoscopically assisted gastrectomy: multivariate analysis of 300 consecutive cases. Surg Endosc. 2008. 22:2133–2139.
24. Kim HY, Kim YK, Uh Y, Whang K, Jeong HR, Choi HJ, et al. Risk factors for neurosurgical site infections after craniotomy: a nationwide prospective multicenter study in 2008. Korean J Nosocomial Infect Control. 2009. 14:88–97.
25. Lee JA, Kim MS, Kim DH, Lim JS, Park KD, Cho WH, et al. Postoperative infection and survival in osteosarcoma patients. Ann Surg Oncol. 2009. 16:147–151.
26. Kim BO, Kim SW, Lee SM, Shin H. Relationship of glucose control and wound infection in diabetics after lumbar spine surgery. J Korean Neurosurg Soc. 2005. 37:44–47.
27. Kim CB, Kim MS, Hong JH, Lee HY, Yu SH. Is laparoscopic appendectomy useful for the treatment of acute appendicitis in Korea? A meta-analysis. Yonsei Med J. 2004. 45:7–16.
28. Kashimura N. Surgical site infection (SSI) prevention and its medicoeconomic effect. J Jpn Soc Surg Infect. 2005. 2:67–72.
29. Graves N, Halton K, Paterson D, Whitby M. Economic rationale for infection control in Australian hospitals. Healthc Infect. 2009. 14:81–88.
30. Justinger C, Moussavian MR, Schlueter C, Kopp B, Kollmar O, Schilling MK. Antibacterial [corrected] coating of abdominal closure sutures and wound infection. Surgery. 2009. 145:330–334.
31. Rozzelle CJ, Leonardo J, Li V. Antimicrobial suture wound closure for cerebrospinal fluid shunt surgery: a prospective, double-blinded, randomized controlled trial. J Neurosurg Pediatr. 2008. 2:111–117.
32. Fleck T, Moidl R, Blacky A, Fleck M, Wolner E, Grabenwoger M, et al. Triclosan-coated sutures for the reduction of sternal wound infections: economic considerations. Ann Thorac Surg. 2007. 84:232–236.







 ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download