Abstract
Serous cystic neoplasms of the pancreas are almost always benign lesions. However, there are some case reports of malignant serous neoplasms of the pancreas. It is very difficult to distinguish malignant and benign tumors. Indeed, only clinicopathologic findings of locoregional invasion and metastasis represent a malignancy. We report a serous cystadenocarcinoma of the pancreas that was initially considered to be colon cancer. Post-operatively, the tumor was confirmed to be a malignant serous cystic tumor of the pancreas. One year later, the patient remains disease-free.
Ten to twenty percent of pancreatic cysts are neoplastic, while only 1% of pancreatic cysts are malignant [1]. Serous and mucinous cystic neoplasms are two types of tumors of the exocrine pancreas, and have different biological behaviors.
Mucinous cystic tumors are typically slow-growing, but carry a significant potential for malignancy, and thus resection is often indicated. In contrast, serous cystadenomas are considered benign tumors with almost no malignant potential [2]. In 1989, George et al. [3] published the first well-documented serous cystadenocarcinoma and proposed it as a new entity.
We report herein a patient with a pancreatic serous cystadenocarcinoma that was initially considered a tumor originating from the colon.
The patient was a 64-year-old woman with no underlying diseases. She had dizziness and hematochezia for several months, and sought evaluation at the emergency room. An abdomen-pelvic computed tomography (CT) was obtained and routine laboratory testing was performed.
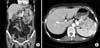
The abdomen-pelvic CT showed a 12 × 9 cm mass adjacent to the stomach that invaded the spleen and pancreas. In addition, there was a tract formation between the mass and transverse colon (Fig. 1). The origin of the mass was not determined, but the transverse colon was suspected. Several small nodules in the liver were thought to represent metastases, so a liver magnetic resonance imaging (MRI) was obtained. On the liver MRI, the small nodules in the liver were shown to be benign cysts. There were no specific lesions involving the lung and other organs.
The hemoglobin was 6.3 g/dL. There were no other abnormal laboratory findings. She was given a blood transfusion.
The patient underwent segmental resection of the colon, a distal pancreatectomy, and a splenectomy. There was no regional lymph node enlargement or malignant ascites.
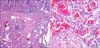
The gross examination revealed a large hemorrhagic mass of the pancreatic tail, with adhesions to the parenchyma of the spleen and all layers of the colon. There was a fistula tract between the mass and colonic mucosa. Multilocular microcystic spaces with diffuse hemorrhage were noted (Fig. 2). The mass appeared to replace most of the distal pancreas.
Microscopically, the tumor consisted of numerous microcysts of various sizes with clear cytoplasm (Fig. 3). The histopathologic findings were compatible with serous cystadenocarcinoma of the pancreas, showing invasive growth into the spleen and colon.
There are two categories of pancreatic cystic neoplams (serous and mucinous cystic pancreatic tumors) [1]. Mucinous cystic neoplasms of the pancreas have a relatively high potential for malignancy, thus surgical removal is the standard treatment [4]. The majority of serous cystic neoplasms of the pancreas are benign. The prevalence of cancer among serous cystic tumors has been reported to be 3% since 1989 [2]. However, serous cystic neoplasms, despite their low prevalence and benign histologic features, have malignant potential and can fulfill all criteria of cancer, including local infiltrative growth and formation of distant metastasis [3,4].
The pre-operative differentiation between a benign serous cystadenoma and a malignant serous cystadenocarcinoma is difficult. Indeed, the correct diagnosis of serous cystadenocarcinoma was not made pre-operatively in any of the cases, including the current case [5]. The benign and malignant variants appear identical histologically, with the only distinguishing feature being gross or microscopic evidence of invasiveness. Thus, the utility of cytology or histology obtained from a core needle biopsy is limited [6]. The pre-operative differentiation of benign from malignant cystic lesions of the pancreas using radiologic examinations is not reliable, except for cases with metastatic disease.
It is difficult to diagnose as a malignant tumor at the time of primary surgery in the absence of invasion to adjacent organs or metastases. In some patients, other organ metastases have been reported to occur several years after the primary procedure. In general, the tumors are very slow-growing and patients have a long life expectancy from the time of diagnosis. Therefore, patients should be followed for a long time.
The opinion that serous cystic neoplasms of the pancreas are always benign may have contributed to the recommendation that resection should be performed only when there is evidence of local invasiveness, distant metastasis, or related symptoms [7]. Even when metastatic lesions are present, surgical resection of primary tumors and metastatic lesions is the most effective treatment [8]. Serous cystadenocarcinomas of the pancreas invade adjacent organs, such as the spleen, regional lymph nodes, and duodenum. In several cases, the tumor spreads to distant organs like the liver, lung, and bone marrow [2].
In the current case, the tumor invaded the colon and spleen. We could not assume the origin of the mass. Post-operatively, a serous cystadenocarcinoma was diagnosed without evidence of distant metastasis, but with extensive tumor invasion into surrounding structures; it was unusual that there was fistula formation to the transverse colon.
Figures and Tables
Fig. 1
Computed tomography of the pancreatic tumor. The tumor invaded the transverse colon (A) and spleen (B).
References
1. Becker WF, Welsh RA, Pratt HS. Cystadenoma and cystadenocarcinoma of the pancreas. Ann Surg. 1965. 161:845–863.
2. Strobel O, Z'graggen K, Schmitz-Winnenthal FH, Friess H, Kappeler A, Zimmermann A, et al. Risk of malignancy in serous cystic neoplasms of the pancreas. Digestion. 2003. 68:24–33.
3. George DH, Murphy F, Michalski R, Ulmer BG. Serous cystadenocarcinoma of the pancreas: a new entity? Am J Surg Pathol. 1989. 13:61–66.
4. Horvath KD, Chabot JA. An aggressive resectional approach to cystic neoplasms of the pancreas. Am J Surg. 1999. 178:269–274.
5. Alfieri S, Pericoli Ridolfini M, Bassi C, Gourgiotis S, Caprino P, Pederzoli P, et al. Cystic tumors of the pancreas: diagnosis, management and results. Chir Ital. 2008. 60:493–508.
6. Kehagias D, Smyrniotis V, Kalovidouris A, Gouliamos A, Kostopanagiotou E, Vassiliou J, et al. Cystic tumors of the pancreas: preoperative imaging, diagnosis, and treatment. Int Surg. 2002. 87:171–174.
7. Kimura W, Makuuchi M. Operative indications for cystic lesions of the pancreas with malignant potential: our experience. Hepatogastroenterology. 1999. 46:483–491.
8. Eriguchi N, Aoyagi S, Nakayama T, Hara M, Miyazaki T, Kutami R, et al. Serous cystadenocarcinoma of the pancreas with liver metastases. J Hepatobiliary Pancreat Surg. 1998. 5:467–470.




 ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download