Abstract
Diagnosing pseudoaneurysms of the popliteal artery is usually straightforward in physical examinations and imaging findings. However, when a pseudoaneurysm shows a soft tissue mass with adjacent osseous change, it can mimic a bone tumor or a soft tissue sarcoma. We present a case of a 65-year-old man who had a pseudoaneurysm of the popliteal artery showing soft tissue mass and insinuating into the intramedullary cavity of the tibia. This presented case emphasizes the importance of considering pseudoaneurysms in the differential diagnosis of an apparent soft tissue mass with pressure erosion in adjacent bone.
The region around the knee is the most common presenting site for the development of a pseudoaneurysm. Common causes of pseudoaneurysms around the knee include blunt trauma, penetrating trauma, fractures, previous surgical procedures, infections, and in rare cases osteochondromas [1]. The presentation of a pseudoaneurysm mimicking a musculoskeletal tumor is very rare [1-3]. In this study, we report a case of a pseudoaneurysm of the popliteal artery insinuating into the intramedullary cavity of the tibia, mimicking a bone tumor or a soft tissue sarcoma.
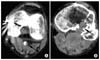
A 65-year-old man presented with severe pain, decreased sensory, and motor weakness of the left lower leg for one day. His medical history included surgery for an ipsilateral knee due to trauma several years previous, but he did not have any recent history of trauma before pain. He had been diagnosed with hypertension 3 months prior and had no history of diabetes mellitus. From physical examination, the left lower leg below the knee was pale and cold. The pulses of the dorsalis pedis artery and posterior tibial artery were not detected. The clinical diagnosis was acute occlusion of the popliteal artery, and thereupon computed tomography (CT) angiography was performed by multidetector computed tomography (MDCT) (Somatom Sensation 16, Siemens, Forchheim, Germany). From MDCT angiography, the left popliteal artery at the femoral condylar level had an eccentric nonenhancing portion, representing intraluminal thrombus (Fig. 1A). At the tibial plateau level, instead of normal intravascular enhancement, a lobulated mass obscured the popliteal artery and insinuated into the adjacent cortex and medullary cavity of the tibia, resulting in an intraosseous mass with erosion and surrounding sclerosis (Fig. 1B). Anteriorly, an obliquely oriented radio-dense line projecting into the intraosseous mass was seen, representing a prior screw fixation site (Fig. 1B). The differential diagnoses of the findings of MDCT angiography were a series of popliteal mass with involvement of the popliteal artery and adjacent bone, such as a popliteal pseudoaneurysm with thrombus formation, soft tissue sarcoma, or a primary malignant bone tumor. Considering the evidence of prior transfixation of a screw, and the finding of a thin sclerotic rim of tibia representing pressure erosion, the radiologist suggested a pseudoaneurysm of popliteal artery with erosion into adjacent tibia along the tract of the screw fixation was more likely than soft tissue sarcoma or a primary malignant bone tumor.
The pulse of the popliteal artery of the patient became progressively weaker, and the surgeon thus decided to perform an emergency mass excision and recanalization of the popliteal artery. After spinal anesthesia, a roughly 10 cm sized longitudinal incision was made at the popliteal fossa. The gastrocnemius muscles were retracted and the popliteal artery was exposed. A vascular origin mass resembling a pseudoaneurysm was identified. The surgeon attempted to excise the mass but it showed severe adhesion with a neurovascular bundle along with luminal narrowing. The surgeon thus decided to perform a two-step operation composed of a thromboembolectomy to restore the arterial pulse as the first step and total mass excision in elective surgery time as the second step. After making a short incision in the inguinal region, the left femoral artery was exposed. The left femoral artery was intact and there was no evidence of arteriosclerosis. Heparinization was done. Catheterization of the common femoral artery was performed using a 3-Fr Forgaty catheter (Edwards Lifesciences LLC, Irvine, CA, USA). After a large amount of non-organized thrombus was removed, the popliteal arterial pulse returned. However, the catheter did not pass into the distal level of the popliteal artery and the pulse again became weaker over time. A small incision at the distal level of the popliteal artery was hence made and further embolectomy was performed. The thrombus was removed at the distal and proximal level of the popliteal artery. However, the catheter did not pass into the tibioperoneal trunk and the pulse of the posterior tibial artery was not restored. After confirmation that the pulse of the dorsalis pedis artery had been restored, the incision of the popliteal artery was closed. The wound was closed with the use of postoperative HemoVac.
The next day, a second operation was performed for removal of mass and bypass surgery anastomosis for the popliteal artery. After administration of spinal anesthesia, a vertical incision was made at the left popliteal fossa, exposing the popliteal artery. The mid- and distal level of the popliteal artery was displaced posteriorly by the mass with adhesion. Heparinization was done. A section of the saphenous vein about 10 cm in length was harvested. After clamping at the proximal level of the popliteal artery, the mid-level of the popliteal artery was incised. An approximately 7 × 5 mm sized oval shaped intimal defect was seen at the anterior surface of the popliteal artery, insinuating into the posterior surface of the tibia. Via the intimal defect, a thrombosed pseudoaneurysm was observed (Fig. 2). Curettage was performed at the organized thrombus in the pseudoaneurysmal sac. Instead of bypass anastomosis, patchy closure and angioplasty were performed at the intimal defect using the harvested lesser saphenous vein, because the native popliteal arterial lumen was relatively intact and the dimension of the harvested vein was too small. The wound was closed with the use of postoperative HemoVac.
Follow-up CT angiographies on post-operative day one showed restored arterial flow in the left lower leg and no residual pseudoaneurysm. The patient was free of symptoms and the pulse of the dorsalis pedis was intact. The patient gradually recovered from sensory and motor deficit. After one month, his pain and sensory and motor deficit had almost disappeared and good dorsalis and posterior tibial pulses were confirmed. From follow-up CT angiographies performed after one year, mild fusiform dilatation of the popliteal artery was noted but the distal run-off arteries were still intact.
Pseudoaneurysms result from arterial wall disruptions with hematoma into the surrounding tissues and containment by a reactive fibrous capsule [2]. The center of the hematoma undergoes organization and recanalization, resulting in direct continuity with the vessel lumen [2]. Pseudoaneurysms are usually progressive and have complications, including thrombosis, embolization, and rupture [2]. In the present case study, the intraluminal thrombus secondary pseudoaneurysm caused complete occlusion into the popliteal artery, necessitating immediate surgery.
The diagnosis of a pseudoaneurysm is more straightforward in the setting of a pulsatile popliteal mass with bruit, and reduced ankle pulse [2]. However, pulsation cannot be detected in some instance and a bruit is generally only associated with recent penetrating trauma [2]. Imaging study consequently has an important role. Doppler ultrasonography is most commonly used in the diagnosis of pseudoaneurysms, as it can depict the characteristic blood flow pattern [4]. Meanwhile, conventional angiography is known to be the most sensitive radiological method for the diagnosis and detection of pseudoaneurysms of arterial origin [2]. In the present case, MDCT angiography was used to make the correct diagnosis. MDCT angiography has many benefits, including being rapid, accurate, and relatively operator independent [5], and accordingly is suitable for emergency situations such as the present case. According to a study by Soto et al. [6], MDCT angiography had a sensitivity of 95.1% and a specificity of 98.7% in the detection of vascular lesions, including pseudoaneurysms, of the proximal parts of the extremities.
The presentation of a pseudoaneurysm mimicking a musculoskeletal tumor is very rare. Most reported cases were related to adjacent osseous change. Gantz et al. [3] reported a pseudoaneurysm at the cruris mimicking a malignant soft-tissue tumor with osseous changes at the fibula. Erler et al. [1] reported a case of a distal femoral arterial pseudoaneurysm with an intraosseous component mimicking a malignant mesenchymal tumor. Correct diagnosis is essential, as these unusual features of pseudoaneurysms can lead to different evaluation algorithms, such as an orthopedic oncological approach and inappropriate treatment, as in the case report of Erler et al. [1].
Although vertebral erosion caused by an aortic pseudoaneurysm was reported [7], in other locations, especially for a popliteal arterial pseudoaneurysm, there have been few cases with adjacent bony erosion, because the popoliteal artery is relatively distant from adjacent bone in comparison with the aorta. According to Bilotta et al. [8], the diagnosis of an aneurysm should be considered if an enlarging mass is identified at a site typical for aneurysm formation. In particular, the feature of arterial encasement, which is uncommon for sarcomas [8], can be utilized for the diagnosis. In our case, arterial encasement and a pressure erosion pattern of bony change led to a correct diagnosis, corresponding to the findings of Bilotta et al. [8].
The treatment of a pseudoaneurysm is generally surgical, such as resection and evacuation of the pseudoaneurysm with repair of the damaged artery, which may include ligation and grafting [9]. Recently, for iatrogenic and small pseudoaneurysms, ultrasound-guided thrombin injection has gained popularity [10].
The present case emphasizes the importance of considering a pseudoaneurysm in the differential diagnosis of an apparent soft tissue mass with pressure erosion in adjacent bone. Identification of factors including a site that is typical for aneurysm formation, arterial encasement, and a pressure erosion pattern of bony change may help achieve the correct diagnosis and surgical treatment is indicated as usual.
Figures and Tables
Fig. 1
Images of arterial phase of multidetector computed tomography angiography of left lower extremity. (A) Left popliteal artery at the femoral condylar level shows an eccentric low attenuated portion, representing intraluminal thrombus (arrow). (B) At the tibial plateau level, instead of normal intravascular enhancement, a lobulated mass (empty arrows) obscured the popliteal artery and insinuated into adjacent cortex and medullary cavity of tibia resulting intraosseous mass with erosion and surrounding sclerosis (black arrow). Anteriorly, an obliquely oriented radio-dense line (white arrow) projected into the intraosseous mass was seen representing prior screw fixation site.
References
1. Erler K, Ozdemir MT, Oguz E, Basbozkurt M. Does false aneurysm behave like a sarcoma? Distal femoral arterial false aneurysm simulated a malign mesenchymal tumor: a case report and review of the literature. Arch Orthop Trauma Surg. 2004. 124:60–63.
2. Keller PM, Simon MS. Post-traumatic false aneurysm simulating a soft tissue tumor. Orthopedics. 1988. 11:641–643.
3. Gantz ED, Sweet MB, Jakim I. False aneurysm mimicking an aggressive soft-tissue tumor: a case report. J Bone Joint Surg Am. 1988. 70:1090–1092.
4. Fitzgerald EJ, Bowsher WG, Ruttley MS. False aneurysm of the femoral artery: computed tomographic and ultrasound appearances. Clin Radiol. 1986. 37:585–588.
5. Novelline RA, Rhea JT, Rao PM, Stuk JL. Helical CT in emergency radiology. Radiology. 1999. 213:321–339.
6. Soto JA, Múnera F, Morales C, Lopera JE, Holguín D, Guarín O, et al. Focal arterial injuries of the proximal extremities: helical CT arteriography as the initial method of diagnosis. Radiology. 2001. 218:188–194.
7. Usselman JA, Vint VC, Kleiman SA. CT diagnosis of aortic pseudoaneurysm causing vertebral erosion. AJR Am J Roentgenol. 1979. 133:1177–1179.
8. Bilotta W, Walker H, McDonald DJ, Sundaram M. Case report 651: Thrombosed, leaking popliteal aneurysm. Skeletal Radiol. 1991. 20:71–72.
9. Parry DJ, Kessel D, Scott DJ. False aneurysm of the peroneal artery: an unusual complication of femoro-peroneal bypass grafting. Cardiovasc Surg. 2002. 10:54–57.
10. Paulson EK, Nelson RC, Mayes CE, Sheafor DH, Sketch MH Jr, Kliewer MA. Sonographically guided thrombin injection of iatrogenic femoral pseudoaneurysms: further experience of a single institution. AJR Am J Roentgenol. 2001. 177:309–316.




 Citation
Citation Print
Print



 XML Download
XML Download