Abstract
Primary splenic tumors are rare and mainly found incidentally on radiologic studies. Among them, sclerosing angiomatoid nodular transformation (SANT) of the spleen is a new entity defined as a benign pathologic lesion. Most SANTs have no clinical symptoms and are occasionally accompanied by other splenic diseases such as malignancies. So, the exact diagnosis of the nature of the splenic tumor is mandatory for further treatment. But, preoperative diagnosis is not easy since it is difficult to obtain the tissue from the spleen for pathological study. Recently, laparoscopic splenectomy has become the more standard procedure for the spleen for diagnosis and treatment. Here, we report a rare case of SANT diagnosed following laparoscopic splenectomy.
Solid tumors of the spleen are relatively rare, with an incidence of 0.007% of all operation and autopsy specimens [1]. It is usually found incidentally on abdominal computed tomography (CT) or ultrasonography. It is difficult to rule out the malignancy by preoperative radiologic studies. Sometimes, fine needle aspiration (FNA) biopsy is used to determine pathologic diagnosis. But this may be associated with bleeding and the risk of tumor dissemination [2]. Therefore, splenectomy is necessary for diagnosis and treatment of the splenic tumors. Recently, laparoscopic splenectomy has become the standard technique for the surgical management of hematological splenic diseases and tumors [3,4].
Sclerosing angiomatoid nodular transformation (SANT) of the spleen is a rare vascular benign lesion that is characterized by Martel et al. [5]. Most patients with SANT have no obvious clinical symptoms and are discovered incidentally through routine evaluation. Since there have been no case introduced in Korean literatures, we report a case diagnosed as SANT of the spleen after laparoscopic splenectomy.
A 23 year old female was admitted to our hospital for evaluation of splenic tumor which was incidentally diagnosed by abdominal CT. Her previous histories and physical examinations were unremarkable. CT examination revealed about 5 × 4 cm sized solid tumor in the spleen, showing low density on pre, early phase, and progressive enhancement on delayed phase (Fig. 1). She wanted pathologic confirmation by operation, and was undergone laparoscopic splenectomy.
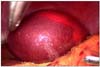
Under general anesthesia, the patient was placed in right lateral decubitus position with the table slightly extended in order to widen the operative field during splenectomy. Three trocars were used along the left subcostal margin and one trocar for the camera port at the umbilicus. Under the pneumoperitoneum of 12 mmHg, dissection was performed using Harmonic ACE (Ethicon Endo-Surgery, Cincinnati, OH, USA). Attending to injury of splenic tumor, we detached following areas; 1) splenic flexure, 2) anterior aspect of the hilum with short gastric vessel, 3) posterior aspect of the left gutter with separation of attachments to the kidney, and 4) some of the attachments to the upper pole of the spleen. After mobilization of the spleen, the vascular pedicle was divided at the level of the splenic hilum by laparoscopic stapling device (Echelon Flex, Ethicon Endo-Surgery) with a special care not to injure the pancreatic tail. Then the spleen was placed in a plastic bag, and taken out through the opening of the most lateral port with additional wound extension by about 3 cm. The normal splenic tissue was fractured using a ring clamp as much as can leave the splenic tumor intact for pathologic diagnosis (Fig. 2).
The spleen shows a well-demarcated, solitary mass, measuring 5.2 × 4.5 cm in dimension. The mass is dark brown with a central large stellate fibrotic scar (Fig. 3). Microscopically, the spleen shows an unencapsulated but well-demarcated mass, composing multiple irregular fibrotic nodules (Fig. 4A). The center of nodules show many small-sized vessels and extravasated red blood cells, so called angiomatoid nodule (Fig. 4B). The periphery of the nodules show abundant collagen fibers infiltrated by many plasma cells, lymphocytes and some eosinophils. The spindle cells of the nodules show positivity for vimentin and α-smooth muscle actin on immunohistochemistry. No cells show positivity for anaplastic lymphoma kinase gene (ALK), S-100. The vascular endothelial cells show CD31 and CD34 immunoreactivity (data not shown).
SANT is rare and newly defined pathological disorder of the spleen with nodular vascular proliferation of the red pulp with prominent sclerosis [5]. SANT usually affects middle-aged adults and shows a female predominance. Most of cases are asymptomatic and discovered accidentally, usually on imaging study. In gross examination of spleen, SANT shows a solitary, well-circumscribed nodule that is distinct from the surrounding splenic parenchyma. In microscopic examination, it consists of three basic cellular components (spindle cells, inflammatory infiltrate, and endothelial vascular proliferation). These cellular components are mixed with each other, creating the angiomatoid nodules of the SANT. These nodules are wrapped by collagen fibers and are intervened by inflammatory and sclerotic responses. SANT shows a distinct immunophenotype. The angiomatoid nodules of the SANT are composed of several morphologically and immunophenotypically distinct blood vessels: a cord capillary-like type that co-expresses CD34 and CD31 but not CD8, a sinusoid-like type that expresses CD8 and CD31 but not CD34, and small veins that express only CD31 [6]. Our pathologic results shows CD31 and CD34 immunoreactivity. Although it remains to be further studied, its clinical prognosis was reported to be excellent with complete cure by splenectomy [6]. Martel et al. [5] reported that SANTs cases showed no evidence of recurrence, which suggests that SANT of the spleen is a completely benign lesion.
Many patients presenting with solid lesions in the spleen will eventually be diagnosed with a malignant tumor, but it is difficult to rule out the possibility of a malignant neoplasm preoperatively based on conventional imaging studies. So it is mandatory to make pathologic confirmation for diagnosis and treatment of solid tumor. Sometimes fine-needle biopsy from the spleen has been used to ascertain tissue diagnosis. However, this procedure has some problems with bleeding or tumor dissemination [2]. Therefore, in most cases, splenectomy is recommended for diagnosis and treatment. With the development of laparoscopic instruments and techniques, laparoscopic surgery has continued to be popularized in almost all fields of surgery. Since the introduction of laparoscopic splenectomy by Delaitre and Maignien [7] in 1992, now laparoscopic splenectomy has been recognized as a safe and effective treatment for hematologic disorders and other splenic diseases [3,8]. Compared with open splenectomy, it is a safer procedure with the advantages of less postoperative pain and complications, early recovery from the procedure, shorter hospital stay, and a much smaller wound incision [9,10]. From this point of view, laparoscopic splenectomy is a good procedure for the diagnosis as well as the treatment that is safer to avoid bleeding and peritoneal dissemination of tumor cells than FNA and allows adequate histological evaluation, especially when malignancy cannot be ruled out. In conclusion, the authors consider that laparoscopic splenectomy can be performed for most splenic tumors such as SANT. SANT is a rare pathologic disease with good prognosis and acceptable for surgical diagnosis and treatment by laparoscopic splenectomy.
Figures and Tables
Fig. 1
Preoperative abdominal computed tomography demonstrates an expansible low density mass (white arrow).
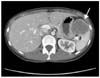
Fig. 3
The spleen shows a well-demarcated, unencapsulated, dark brown mass with central stellate fibrotic scar on cut section.
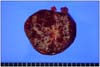
Fig. 4
Microscopic findings in sclerosing angiomatoid nodular transformation of spleen. (A) The tumor shows multinodular lesion surrounded by fibrosis. The nodules are irregular and composed of many small-sized vessels. The fibrotic area shows abundant collagen fibers and inflammatory cells hematoxylin-eosin (H&E, ×40). (B) The high power view of angiomatoid nodular lesion, it shows many vessels, extravasated red blood cells and inflammatory cells (H&E, ×100).

References
1. Moriyama S, Inayoshi A, Kurano R. Inflammatory pseudotumor of the spleen: report of a case. Surg Today. 2000. 30:942–946.
2. Caraway NP, Fanning CV. Use of fine-needle aspiration biopsy in the evaluation of splenic lesions in a cancer center. Diagn Cytopathol. 1997. 16:312–316.
3. Stephens BJ, Justice JL, Sloan DA, Yoder JA. Elective laparoscopic splenectomy for hematologic disorders. Am Surg. 1997. 63:700–703.
4. Walsh RM, Brody F, Brown N. Laparoscopic splenectomy for lymphoproliferative disease. Surg Endosc. 2004. 18:272–275.
5. Martel M, Cheuk W, Lombardi L, Lifschitz-Mercer B, Chan JK, Rosai J. Sclerosing angiomatoid nodular transformation (SANT): report of 25 cases of a distinctive benign splenic lesion. Am J Surg Pathol. 2004. 28:1268–1279.
6. Teng X, Yu X, Wang G, Xu L, Lai M. Sclerosing angiomatoid nodular transformation of the spleen. Anal Quant Cytol Histol. 2008. 30:125–132.
7. Delaitre B, Maignien B. Splenectomy by the laparoscopic approach: report of a case. Presse Med. 1991. 20:2263.
8. Rosen M, Brody F, Walsh RM, Tarnoff M, Malm J, Ponsky J. Outcome of laparoscopic splenectomy based on hematologic indication. Surg Endosc. 2002. 16:272–279.
9. Lee SG, Kim MC, Kim HH, Kwon HC, Jung GJ. Treatment result of laparoscopic versus open splenectomy in benign splenic diseases. J Korean Surg Soc. 2005. 68:230–234.
10. Bellows CF, Sweeney JF. Laparoscopic splenectomy: present status and future perspective. Expert Rev Med Devices. 2006. 3:95–104.




 Citation
Citation Print
Print


 XML Download
XML Download